![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
308 Cards in this Set
- Front
- Back
|
Four things techs are legally prohibited to do
|
Diagnose, prognose, prescribe, surgery
|
|
|
FDA - What it stands for and what do they do?
|
Food and Drug Administration
The United States federal agency that regulates the manufacture and distribution of food additives and drugs that will be given to animals |
|
|
Drug Names: Proprietary, Chemical and Non-Proprietary
|
Chemical: describes the chemical composition of a drug
Proprietary or Trade Name: Unique name given by manufacturer of the drug. Ex: Tylenol Non-Proprietary or Generic name: More concise name given to the chemical compound. Ex: acetaminophen |
|
|
Dosage Regimen -
Information Required |
The general amount of drug that needs to be given over time; or a general description of how drug is to be given. Includes size, amount, frequency, and number of doses .Ex: Give 2 mg/kg every 8 hours for ten days.
|
|
|
Dosage Forms
|
The description of a drug's physical appearance or type. Ex: caplets, cream, suspension
|
|
|
Drug Information: Package Inserts
|
Included with each container of drug. Provide essential information as required by the FDA and most frequently updated resource.
|
|
|
Drug Information: Formularies
|
Small booklets containing common drug doses. Also can include more info as it pertains to veterinary use that's not on the label. Other larger books are also available but can become outdated quikly, but they do provide more information than what's on package inserts.
|
|
|
Drug Information: Reference Books (PDR)
|
Contains human drug information and helpful when an animal has ingested a human med or when needing pediatric doses of a drug not available in veterinary form.
|
|
|
Information Listed in Drug References
|
RX, trademark, Trade Name, Non-Proprietary Name, Class (if controlled), How Supplied (e.g. vials, caplets), phonetic spelling in some cases, ingredients, reactions, indications, precautions, warnings, contraindications
|
|
|
Controlled Substance
|
Federally controlled (by the DEA) drug, more potential to become addicted and subject to abuse
|
|
|
USP - What it stands for and what they do?
|
United States Pharmacopeia - an organization that sets the standards for manufacture of drugs sold in the US.
|
|
|
Inert Ingredients
|
Preservatives, stabilizers,liquid media or other additives that make up the dosage form.
|
|
|
Drug Indications
|
Purposes for which the drug may be used. Specific FDA approved uses
|
|
|
Drug Precautions
|
Fairly rare adverse reactions or mild side effects.
|
|
|
Drug Warnings
|
More serious or frequent side effects than those found in precautions. Can be potentially life threatening.
|
|
|
Drug Contraindications
|
Circumstances in which the drug should not be used. Ex: do not use this drug if you have liver disease
|
|
|
Drugs: Off-Label and Extra-Label Use
|
Drug is being used in a manner other than what's on the drug's label or listing. Also for extra label, includes different dose or route, use in another species, or another purpose intended.
|
|
|
Active Ingredient
|
The drug itself
|
|
|
Ampule
|
Small, airtight glass container that has one dose; neck broken to get at drug
|
|
|
Caplets
|
Powdered drug compressed into capsule shape
|
|
|
Depot Drug
|
A drug formulated to prolong absorption of the drug from the administration site. Designed to provide a more sustained, effective drug concentration in the body. Same as Repository
|
|
|
Dosage
|
Same as dosage regimen:
The general amount of drug that needs to be given over time; or a general description of how drug is to be given. Ex: Give 2 mg/kg every 8 hours for ten days. |
|
|
Dose
|
Amount of drug that is administered at one time to a patient. Ex: 1 ml
|
|
|
Elixer
|
Orally administered solution of drug dissolved in alcohol
|
|
|
Emulsion
|
Suspension in which drug is mixed with a liquid fat or oil.
|
|
|
Enteric-coated Tablet
|
Special coating over powdered drug that protects it from stomach acid and prevents dissolution of the tablet until it's in a more alkaline enviroment of the small intestine.
|
|
|
Extract
|
A therapeutic agent derived from a plan or animal source rather than synthesized chemicals in a lab. Ex: pancreatic enzyme powder extract
|
|
|
Gel Caps
|
Powdered drugs placed in gelatin capsules
|
|
|
Generic Equivalent
|
After exclusive rights to manufacture a drug expire, drugs produced by a company other than the original developer are called generic equivalent. Properties of these drugs are equivalent to the original compound but sold for lower proce.
|
|
|
Generic Name
|
Non proprietary name; more commonly used chemical name. Ex: acetominophen
|
|
|
Injectable Dosage Form
|
Administered by needle and syringe
|
|
|
Liniment
|
Drugs dissolved or suspended in an oil base and are rubbed in
|
|
|
Lotion
|
Drug suspension or solution that's dabbed, brushed or dripped onto skin without rubbing
|
|
|
Molded Tablet
|
Powdered drug that's compressed into a disk form
|
|
|
Multidose Vial
|
Glass vial of injectible medication that's designed for use multiple times Ex: PenG
|
|
|
Ointment
|
Suspension or solution that's designed to liquify at body temperature. For external use
|
|
|
Paste
|
Semisolid orally administered drugs designed to keep their form at body temp. Used a lot in large animal med.
|
|
|
Repository Form
|
A drug formulated to prolong absorption of the drug from the administration site. Designed to provide a more sustained, effective drug concentration in the body. Same as Depot
|
|
|
Single-Dose Vial
|
Injectable drug that is packaged in a single dose vial. Ex: vaccines
|
|
|
Solution
|
A drug that's completely dissolved in a liquid that does not precipitate out when left standing.
|
|
|
Suspension
|
A drug that's "suspended" in a liquid but not completely dissolved. They will precipitate out and need to be shaken before administration.
|
|
|
Sustained-Release Formulation
|
Oral dosage form that's designed to release only small amounts of the drug into the intestinal lumen over an extended period. Don't work too great in vet med
|
|
|
Syrup
|
A a drug suspension or solution dissolved in sugar water.
|
|
|
Tincture
|
An alcohol solution meant for application to the skin. Ex: tincture of iodine
|
|
|
Topical Application
|
Application to the skin
|
|
|
Trade Name
|
Proprietary name. Ex: Tylenol
|
|
|
Troche
|
Lozenges - not used in vet med
|
|
|
Drug Adverse Reaction/Side Effect
|
Any effect of the drug other than it's intended beneficial effect.
|
|
|
Antineoplastic Agent
|
Cancer drug; generally poisonous to mammalian cells
|
|
|
Apothecary System
|
Old system, not used much in Vet med but know grains and fluid ounces
|
|
|
Metric System: Definition and Common Terms
|
System that's most commonly used for drug dosages in Vet med
1kg = 1000 g and 2.2 lbs 1 g = 1000 mg 1 mg = 0.001 g 1 mg = 1000 mcg 1 L = 1000 ml 1cc = 1ml = 1g |
|
|
Carcinogenic Effect
|
Can induce cancer or preneoplastic changes in animals and humans
|
|
|
Insulin: Dosage ML vs Units
|
IU aka U-100
1 ml = 100 International Units (IU) U40 1 ml = 40 Units |
|
|
Compounding Drugs: Definition and Examples
|
Any manipulation to produce a dose form of a drug in any form other than what's been approved by the FDA. Ex: formulating Tapazole into a topical paste to apply on the ear pinnea; creating a smaller capsule dose of a human drug for animals
|
|
|
Cytotoxic Drugs
|
Drugs that are especially poisonous to mammalian cells
|
|
|
Dosage Range
|
Allows the Vet to select a dosage for the patient based on a range. Ex: give 2-4 mg/kg
|
|
|
Household Measurement System: Common Conversions to Metric
|
1 oz = 30 ml
1 Tbl. = 15 ml 1 tsp. = 5 ml |
|
|
MSDS
|
Material Safety Data Sheet
Sheet that lists guidelines for protective precautions, cleanup and first aid for exposure for all hazardous compounds. |
|
|
Mutagenic Effect
|
Can cause birth defects in a human fetus
|
|
|
OSHA
|
Occupational Safety and Health Administration
They developed guidelines for safe storage, use and disposal of chemicals and drugs |
|
|
OTC
|
Over the Counter
A drug that does not require a prescription to obtain |
|
|
Percentage Solution
|
The number of grams of drug (solute) in 100 ml of liquid (solvent) Ex. a 20% solution has 20g of drug in 100 ml of liquid
|
|
|
Prescription Drugs
|
A drug that is considered potentially toxic if misused, toxic, or too readily misused is considered a prescription drug. They can only be dispensed upon the lawful order of a licensed veterinarian.
|
|
|
Schedule Drugs
|
Same as controlled drug.
|
|
|
Teratogenic Effect
|
Same as mutagenic - can cause birth defects in a human fetus.
|
|
|
DEA
|
Drug Enforcement Agency
Provides authorization for Vets to use or buy controlled substances. |
|
|
USDA
|
US Department of Agriculture
Food safety for meat, poultry, eggs, etc. |
|
|
EPA
|
Environmental Protection Agency
Protect the environment and public health |
|
|
What phrase must the label for Rx drugs contain?
|
Caution: Federal law restricts this drug to use by or on the order of a licensed veterinarian.
|
|
|
Prescriptions vs Drug Orders: What can Techs do?
|
Fill drug orders and dispense medications as instructed by veterinarians within their practice.
|
|
|
Prescriptions vs Drug Orders: Labels for Dispensed RX Drugs - What info is required and what addtl. info for food animals?
|
Name, address, tel# for vet, name and address for client, patient ID, drug name, concentration and number of units, clear instructions for dosage, frequency, duration of treatment, cautionary statements (give on empty stomach) and for food animals, specified withdrawal or discard times
|
|
|
Containers for Dispensing Meds
|
While not required to use childproof containers in the veterinary field, we are morally and ethically obligated to inform clients when containers are not childproof and to advise them to keep the medication out of the reach of children
|
|
|
Storage of Drugs: Environmental Considerations - what are they?
|
Temperature
Sensitive to light Sensitive to moisture Ionizing radiation Vibration Lack of preservatives in reconstituted drugs |
|
|
Controlled Substances/Schedule Drugs:What Regulatory agency enforces?
|
DEA - Drug Enforcement Agency
|
|
|
Controlled Substances/Schedule Drugs: What do DVMs need in order to use, prescribe or buy?
|
DEA certification number
|
|
|
Controlled Substances/Schedule Drugs: Requirement for Computer Drug Logs
|
Legitimate if the software allows only minor editing of log entries and creates an uneditable note file of any such changes made to the record. Many states require back up hard copies.
|
|
|
Controlled Substances - Classes and Drug Examples
Class IC-I |
Class IC-1: Extreme abuse potential; None aproved for use in the US
Heroin, LSD, Marijuana |
|
|
Controlled Substances - Classes and Drug Examples
Class II |
High abuse potential; may lead to severe physical or psychological dependence
Opium derivatives - pentobarbitol, morphine Demerol, euthanasia solutions |
|
|
Controlled Substances - Classes and Drug Examples
Class III |
Some abuse potential; may lead to low/moderate physical or high psychological dependence
Pentothal, Telazol (Ket-Val), hydrocodone, ketamine, euthanasia solutions, testosterone |
|
|
Controlled Substances - Classes and Drug Examples
Class IV |
Low abuse potential; may lead to limited physical-psychological dependence
Phenobarbital, diazepam (Valium), Butorphanol, Talwin |
|
|
Controlled Substances - Classes and Drug Examples
Class V |
Low abuse potential; subject to state and local regulation
Lomotil, Winstrol-V |
|
|
Storage and Handling of Cytotoxic and Hazardous Drugs: Guidelines for Safe Storage, Use and Disposal of Chemicals and Drugs
|
- Store separately from other drugs and pay attention to environmental requirements, like temperature and light
- Clearly label - Prepare just before deliver to patient - Administer in a low-traffic, well ventilated area - Wear proper protective attire - Use lines and syringes with screw on attachments to prevent spilling - Recheck calculated dose - Promptly dispose of all items used in a sealed, plastic bag immediately after use - Dispose as hazardous waste in a punctureproof leakproof container |
|
|
Storage and Handling of Cytotoxic and Hazardous Drugs: How can accidental exposure occur?
|
- Storing meds and biologicals in the fridge with food
- Eating lunch in the work area where exposure to meds, biologicals, etc. can occur - Not following good personal hygeine and safety practices |
|
|
Nociception - Definition
|
Special kind of nerve cell in skin and deep tissues. Transduction, conduction and central nervous processing of signals generated by the stimulation of the nociceptors. Nociceptors send nerve impulses along a chain of at least 3 neurons
|
|
|
Nociceptors aka Pain Pathway - The Four Phases
|
- Transduction: noxious stimuli to the nociceptor; stimulus of sensory nerve endings
- Transmission: propagation of the nerve impulses thru the peripheral nervous system - Modulation: occurs in the spinal cord which modifies the transmission of the stimuli; neurotransmitters involved - Perception: final process that will deviate the animal's behaviour and emotional response (crying, chewing, BP) |
|
|
Pain - Definition
|
An unpleasant sensory or emotional experience assosicated with actual or potential tissue damage.
- Physiological: recognition of sensation from heat, cold or pressure - Pathological: result from inflammation or neuropathic processes |
|
|
Good Nursing Tecniques to Minimize Pain
|
- Drugs
-Keep patient warm and dry - Patient positioning - Comfortable bedding - Ample opportunities to go potty - Turn the patient - Quiet surroundings - Cool bath if warranted - TLC |
|
|
Two Main Types of Pain - Defined
|
Somatic - skin, sq, muscle, bones, joints (stabbing, throbbing, aching)
Visceral - organs (cramping, burning) |
|
|
Levels/Intensity of Pain and Examples (SX and Conditional)
|
* Mild to Moderate - OVH, Castration, Routine Dental
* Moderate - Laparotomy, Cystotomy, Gastrotomy, Mass Removal * Moderate to Severe - FX Repair, ACL, Mammary Gland, Enucleation, Ear SX, Declaw * Severe to Excruciating - Neuropathic, Multiple FX, Bone Cancer |
|
|
Kinds of Pain:
Acute |
Surgical
Can usually be TX with analgesics |
|
|
Kinds of Pain:
Chronic |
Slow onset; Long Duration; may be unresponsive to drug therapy
Osteoarthritis, IVDD, Cancer, |
|
|
Kinds of Pain:
Referred |
Pain felt in another body part other than one affected
Ex: painful limb from a verterbral disc problem |
|
|
Kinds of Pain:
Hyperesthesia |
Increase in sensitivity to stimuli like touch or sound
"wind-up phenomenon" |
|
|
Kinds of Pain:
Neuropathic |
Due to damage of a peripheral nerve or spinal cord itself; usually poorly responsive to meds
|
|
|
Common Signs of Pain
|
- Increased HR and RR
- Decreased appetite - Dilation of pupils - Salivation - Vocalization - Attitude and facial expression changes - Guarding painful site - Restlessness or unresponsiveness - Failure to groom - Abnormal gait - Rolling |
|
|
Most severe pain typically occurs ___ hours post-op
|
24
Must closely monitor patient as we typically don't know their normal behavior |
|
|
Neuroleptanalgesia -
Definition |
Use of an opioid with a tranquilizer to provide a more potent sedation and offers better analgesia through SX and for a time afterward
|
|
|
Things to Remember when Using Opioids as Analgesics
|
- If used as a pre-med, doesn't last very long post-op
- Most effects are gone 2-4 hours after administration - Can be used with other agents, such as NSAIDs or local anesthetics to provide post-op analgesia |
|
|
Multimodal or Balanced Analgesia/Pain Management-
Definition |
Using more than one type of analgesia to relieve pain (using meds from different classes).
This works because there are several mechanisms by which pain is produced. Ex: NSAIDs and opioids - Can reduce the amount of meds necessary to relieve pain - Can minimize side-effects - Using pre-, intra-, and post surgical techniques allows for better control of pain |
|
|
Opioid Analgesics -
How they Work |
- Relieve pain by binding with specific receptors in the CNS and peripheral tissue
- Inhibit or block pain receptors - One of the most effective drug classes in relieving mod-severe pain |
|
|
Opioids -
Info and Side Effects |
- Excellent pain relieving properties
- Reversal agent - Naloxone - Wide safety margin - Often used in combo with tranquilizers to attain a state of neuroleptanalgesia - Many are controlled substances - Can initially increase GI activity then decrease - Panting - Respiratory depression - Bradycardia - Sedation - Excitement in cats and horses - Addiction (pet owners) |
|
|
Opioid Receptors
|
- Mu: Morphine, analgesia, euphoria and physical dependence
- Kappa: analgesia and sedation - Sigma: vocalization and hallucinations - Delta: modify Mu |
|
|
Opioids for Moderate to Severe Pain
List only |
- Morphine
- Oxymorphone - Hydromorphone - Fentanyl |
|
|
Opioids for Moderate to Severe Pain
Morphine |
- Pure agonist with actions at the mu and kappa receptors
- Controlled substance - Class 2 - Used for visceral and somatic pain - Used in cats and dogs; be careful with cats and horses - Morphine Mania - Can cause vomiting so contraindicated in vomiting patients (e.g., post GI SX) - Induces histamine release if given too fast IV; causes facial swelling - Provides 2-3 hr for severe pain and 4-6 hrs for mild to moderate pain - Given slow IV (not cats), IM, SQ, IA, epidurally and spinally |
|
|
Opioids for Moderate to Severe Pain
Oxymorphone |
- Mu agonist
- Controlled substance Class 2 - Greater analgesic potency and sedative effect than morphine with fewer side effects and longer duration of analgesia - Relatively $$$ - Provides 1-5 hrs analgesia - Less vomiting than morphine - Does not induce histamine release - Sometimes patients pant more, hyper responsive to sound and may show bradycardia - Given IV, IM, SQ or epidurally |
|
|
Opioids for Moderate to Severe Pain
Hydromorphone |
- Mu and kappa agonist
- A little less potent than oxymorphone but with a similar duration of effect - Much less $$ than oxymorphone so may see this a lot more in the real world - Side effects similar to morphine (panting, bradycardia, excessive sedation and excitement at higher doses - Less potential of causing excitement in cats than morphine |
|
|
Opioids for Moderate to Severe Pain
Fentanyl |
- Very potent (80-100X that or morphine)
- Rapid onset but short duration of effect - IV drip (CRI) or as a patch; also IM, SC or epidurally - Can induce sedation, panting, hypersensitivity to sound - Used in cats and dogs primarily for post-op pain after major SX or chronic, severe pain (cancer) - Lag time until patch kicks in - 6 hr cats, 12 hr dogs - Must wear gloves and never cut patch with gel - Area must be clipped but not shaved - Must be replaced every 3 days - Mylan Pharm. - generic patch with drug in the glue; can cut to desired size |
|
|
Opioids for Mild to Moderate Pain
List Only |
- Butorphanol
- Buprenorphine |
|
|
Opioids for Mild to Moderate Pain
Butorphanol |
- Agonist/antagonist
- Not a controlled substance - Partial agonist at Mu (antagonizes morphine) - Full agonist at kappa and sigma - Used for visceral pain in cats, dogs, horses - IV, IM, SC or PO - Short duration of analgesia - maybe 3/4 to 1-1/2 hr - Partially reverse the adverse effects of other opioids (morphine) but also reverses analgesic effects |
|
|
Opioids for Mild to Moderate Pain
Buprenorphine |
- Partial agonist
- Stimulates the mu receptors but less than morphine - Kappa antagonist - IV, IM or epidural - Works well in cats via oral transmucosal (OTM) route due to high pH of cat saliva (bioavailability ~100%, small volume and no real taste) - Takes longer to exert effects - 40 min - but provides longer duration of analgesia (6-12 hr IM and 18-24 hr epidural) |
|
|
Basics of Inflammation -
Process Defined |
Inflammation is the process that occurs in the body in response to tissue injury from physical, chemical, or biological trauma
|
|
|
The Point of Inflammation
|
- To counteract the injury by removing or walling-off the cause of injury
- To repair or replace the damaged tissue |
|
|
Clinical Manifestations of Inflammation
|
- Redness
- Heat - Swelling - Pain Think of a splinter in your finger |
|
|
If Inflammation Allowed to Continue...
|
Can cause further injury and tissue damage:
- Allergy - Shock (histamine release) - Proud Flesh (horses) and Cockers with otitis externa |
|
|
Arachidonic Acid Cascade -
Defined |
Branch 1:
- Cyclooxygenase (COX) - Prostaglandins - Thromboxanes Branch 2 - Lipoxygenase (LOX) - Leukotrienes |
|
|
Inflammation -
Chemicals Released During Cell Damage |
- Prostaglandins
- Leukotrienes - Histamine - Cytokines |
|
|
Bodies Response to Inflammation
|
- Increased blood flow/perfusion to damaged area (WBCs)
- Leads to dilution of the offending agent, fibrin to immobilize and phagocytic cells to get rid - HOWEVER, overreaction can make it worse: anaphylaxis, pain, cell death |
|
|
Cyclooxygenase -
Definition |
- One of the enzymes in the inflammatory cascade
- Responsible for making prostaglandins |
|
|
COX 1
|
- Maintains physiologic functins like renal blood flow and synthesis of the gastric mucosa (good prostaglandins)
|
|
|
COX 2
|
Stimulates formation of prostaglandins which mediate (cause) inflammation and pain (bad prostaglandins)
**Want drug to inhibit this** BUT can also play a role in ulcer healing and maintenance of renal blood flow during stress |
|
|
Fever-
Info and Causes |
- Chemical mediators released by damaged cells can cause fever
- Stress that raises body temp NOT considered to be fever - Fever an important clinical indicator of disease |
|
|
Purpose of Fever
|
- Destruction of invading viruses or bacteria by heat inactivation
- Facilitating biochemical reactions in the body (many reactions increase with heat) |
|
|
Pyrogen -
Definition |
A substance which can induce fever
Think Pyro=Fire |
|
|
Exogenous Pyrogens -
Defined |
Come from Outside the body, such as viruses and bacteria
|
|
|
Endogenous Pyrogens -
Defined |
Come from Inside the body and are usually chemical mediators, such as prostaglandins; can be induced by something outside the body or they can be released directly from damaged cells
|
|
|
NSAIDS -
Definition, how they work and general info |
- Non-Steriodal Anti-Inflammatory Drugs
- Work by inhibiting cyclooxygenase (unlike opioids which work centrally on opioid receptors) - Drugs in this class have varying degrees of analgesia effects - Some have anti-pyrexia (anti-fever) properties - NSAIDs that inhibit only COX 2 have decreased GI side effects |
|
|
NSAIDS -
General Adverse Effects |
- GI ulceration and bleeding as may interefere with normal mucus coating of the stomach
- Nephrotoxicity (e.g., overuse of ibuprofen) - Bone marrow suppression - Bleeding tendencies - Hepatoxicity |
|
|
NSAIDS -
Contraindications and Precautions |
- Use caution in patients with liver or renal insufficiencies
- Contraindicated in animals with bleeding disorders (von Willebrand's DZ) - DO NOT USE CONCURRENTLY WITH STERIODS OR OTHER NON-STEROIDALS (ULCERS) - Use with caution in animals with hypoproteinemia - 1 or 2x yearly blood panels to monitor kidney and liver functions with long term use |
|
|
NSAIDs -
Acetylsalicylic Acid |
- Aspirin (abbrev. ASA)
- Analgesic, anti-inflammatory, anti-pyrexia, anti-platelet effect - Vet med used for: - mild-mod pain associated with osteoarthritis - Pulmonary artery DZ 2ndary to heartworm infestation (rt side of heart) - Cardiomyopathy in cats - Buffered form preferred |
|
|
NSAIDs -
Phenylbutazone |
- Bute, Butazolidin
- Used predominantly in horses but also approved in dogs - Analgesic, anti-pyretic, anti-inflammatory - Used in horses for mild-mod pain with lameness, fever reducer, anti-inflammatory - Long term use causes ulceration of the right dorsal colon and renal failures - In cattle one dose requires 30 days w/d time |
|
|
NSAIDs -
Flunixin Meglumine |
- Banamine
- Predominantly used in horses but approved for cattle - Used off label for dogs with parvo*** - Use extreme care- very potent and takes temp down rapidly - sometimes too rapidly - Analgesia (visceral pain - colic), anti-inflammatory, anti-pyrexia (in endotoxemia - parvo puppies) - Usually given IV |
|
|
NSAIDs -
Carprofen |
- Rimadyl chewable tabs (keep away from dogs and kids)
- Approved for use in dogs - DJD DZ or post op - Anti-inflammatory and analgesic - Safer than aspirin on GI system but still must watch for signs, including V&D, melena (black tarry stool due to bleeding in upper GI) - Labs reported susceptible to acute hepatic failure |
|
|
NSAIDs -
Ketoprofen |
- Ketofen, Orudis (human)
- Analgesic, anti-inflammatory, anti-pyretic - Approved for use in horses but off label in cats and dogs - Used for MS pain and inflammation in horses and post op pain in cats and dogs - Monitor animals for V and anorexia, melena |
|
|
NSAIDs -
Etodolac |
- Etogesic
- Seems more selective for inhibition of Cox-2 rather than Cox-1 - Used for pain and inflammation associated with osteoarthritis in dogs - NOT SAFE in dogs under 12 mos old - In addition to other NSAID side effects, can cause irreversible KCS in some dogs |
|
|
NSAIDs -
Meloxicam |
- Metacam, Mobic (human)
- A Cox-2 preferential NSAID - Fewer side effects than other NSAIDs, GI possible but low, renal toxicity low; unknown hepatoxicity - Analgesia and inflammation associated with osteoarthritis and post op pain - Maintenance dose is 1/2 of loading dose - Can use off-label in cats with caution |
|
|
NSAIDs -
Deracoxib |
- Deramaxx
- Predominantly inhibits Cox-2 and spares Cox-1 at therapeutic doses - Treats post op pain and pain/inflammation associated with osteoarthritis on dogs - Chewable tabs - keep away from dogs and kids |
|
|
NSAIDs -
Tepoxalin |
- Zubrin
- **Dual inhibitor of both COX and LOX- blocks both arms of the arachidonic acid cascade. - Blocking LOX means reduction in leukotrienes which contribute to inflammatory responses in joints and GI tract - Side effects include GI and others like incoordination, incontinence, polyphagia, flatulance, hair loss, trembling - Rapidly disintegrating tablet once in the mouth |
|
|
NSAIDs -
Firocoxib |
- Previcox
- Inhibits Cox-2 while sparing Cox-1 - Used to treat pain and inflammation associated with canine osteoarthritis - Chewable tablets - keep away from dogs and kids |
|
|
Acetominophen
|
- Tylenol
- Not really an NSAID - NO ANTIINFLAMMATORY - Anti-pyrexic and analgesia only - Can be used in dogs in proper doses - NEVER used in cats - they can get methemaglobinemia-blood cannot carry O2, dyspnic, also swollen head - Antidote for cats acetylcystine IV |
|
|
NSAIDs -
Ibuprofen |
- NEVER used in dogs and cats
- Major toxicity including acute renal failure |
|
|
Other Anti-Inflammatories that Are Not Steroids -
DMSO |
- Dimethyl sulfoxide
- Free radical scavenger that has anti-inflammatory and analgesic effects; effects compared to opioids - Easily penetrates the skin; serves as a carrier agent in promoting skin absorption of drugs and toxins - More effective anti-inflammatory for acute inflammation rather than chronic - Animals can taste when applied topically or IV - garlic smell |
|
|
Other Anti-Inflammatories that Are Not Steroids -
Adequan |
- Known as PSGAG (polysulfated glycosaminoglycan)
- Cosequin another brand name - Kind of like a more potent glucosamine - Not related to anything else in this class - Reduces inflammation by reducing prostaglandins released in joint injury and thickens synovial fluid - IM or IA - aseptic technique!! - In dogs dose-related coagulopathy (bleeding disorder) has been described |
|
|
Glucocorticoids -
General Info |
- AKA Corticosteriods, Steroids
- Have an effect on every cell type and system in mammals: CV, CNS, Endocrine, Blood, GI, Liver - **Rarely a cure but a treatment for the symptoms of a DZ - Augment the body's natural immune or inflammatory response to make the animal feel good, even if only temporarily - Cats usually require higher doses (generally pred) - Dosage depends on use (anti-inflammatory vs immunosuppressive) **Can lower seizure threshold** |
|
|
Steriods -
Some Uses |
- Stimulate appetite
- Adrenal insufficiency (Addison's) - Allergies - Asthma - Autoimmune disorder (thrombocytopenia, AIHA) - Neoplasia - Increased CSF pressure - Shock/toxemia |
|
|
Steroids -
Adverse Effects/Warnings |
- Usually associated with long term therapy, especially higher doses
- PU, PD - Polyphagia - Panting - Weight gain - Dull haircoat - Elevated liver enzymes - GI ulcers - Behavioral changes - DM |
|
|
Steriods -
Common Ones Used |
Most to least potent:
Mometazone (7.7X more potent) Betamethasone Dexamethasone Flumethasone Triamcinolone Methylprednisone (Depo Medrol) Methylprednisolone Sodium Succinate Prednisone/Prednisolone |
|
|
Prednisone/Prednisolone
|
- Prednisone is activated by the patient's body into Prednisolone
- Usually considered interchangeable - Some cats are not efficient at the conversion and do better on prednisolone (weird livers, lack liver enzymes) |
|
|
Local Anesthetics -
General Info |
- Work by preventing the generation and conduction of nerve impulses in peripheral nerves
- Nerve function loss - first to last: pain, warmth, touch, deep pressure, motor function - Absorption of locals into the systemic circulation must be considered in all patients - Changes in renal and hepatic function will prolong drug clearance from the body and increase the potential for side effects |
|
|
Local Anesthetics -
Methods of Use |
- Topically: skin, eye, ear, larynx
- Infiltration: injected into sq or muscle tissue, IT - IV: Bier Block distal extremity Regional: epidurals, diagnostic nerve block |
|
|
Local Anesthetics -
Epidural |
- Placed in epidural space of the SC
- Are not placed above the unbilicus as this can cause respiratory paralysis - Used for some orthopedics, amputations, and C-sections |
|
|
Local Anesthetics -
Side Effects, Warnings |
- Relatively free of harmful side effects when used at appropriate doses
- Most potentially harmful side effects occur after accidental IV administration or absorption of lg. amount after regional administration: - CNS excitement rather than depression - CV - arrhythmias - Allergies - rash or hives, anaphylaxix - Paresthesia - oins and needles when local is wearing off - **ALWAYS ASPIRATE - Use of epinephrine is sometimes employed to cause vasoconstriction in the area for less bleeding, less absorption, prolonged effect of local |
|
|
Local Anesthetics -
Proparacaine |
- Rapid acting and uses for ophthalmic procedures
- Primarily anesthesizes the cornea - Short duration 5-10 min - Fridge and protect from light |
|
|
Local Anesthetics -
Lidocaine |
- Rapid onset of action and short duration (60-120 mins)
- 78% of dose reaches the general circulation - Absorption slowed and effect prolonged if used with epi - Burns when first injected; can use sodium bicarbonate to stop burn 1:10 ratio (1sb to 9 lido) - Supplied in 1 and 2% |
|
|
Local Anesthetics -
Mepivicaine |
- Trade name Carbocaine
- About equally as potent at lido but longer duration (90-180 min) and has less vasodilation |
|
|
Local Anesthetics -
Bupivicaine |
- Trade name Marcaine
- Longer acting and about 4x more potent than lidocaine - Onset of action slow to intermediate and duration is 3-10 hours - Commonly used for regional and epidural nerve blocks - CNS and cardiac toxicity result from lower doses and blood levels than those reported for lidocaine - ASPIRATE - Dose is calculated for entire patient (e.g., declaws split between the two paws) |
|
|
Other Pain Meds -
Tramadol |
- Dual action: Mu agonist and monoamine reuptake inhibitor
- Analgesia compared to demerol - Can be used with NSAIDs or mu agonists (multimodal) - Side effects rare, but include GI upset, sedation, tastes bad |
|
|
Other Pain Meds -
Amantadine |
- Oral NMDA receptor agonist
- Used to TX Parkinsons in people |
|
|
Other Pain Meds -
Gabapentin |
- Neurontin
- Anticonvulsant with purported adjunctive analgesic action - MOA unknown - Best application may be for neuropathic pain (shingles) - $$$ |
|
|
Other Pain Meds -
Amitriptyline |
- TCA (tricyclic antidepressant)
- Trade name Elavil - Used as adjunct to other analgesics (especially opioids) for chronic pain - Also used for symptomatic TX of idiopathic feline LUTD |
|
|
Nervous System -
Description and Functions |
- The body's primary communication and command center
- Sensory - Senses changes in the environment and w/in the body - Integrative (analysis) - Interprets the information - Motor (action) - Responds to the interpretation by bringing about an appropriate action |
|
|
Central Nervous System (CNS) - Definition and Composition
|
Control Center
- Brain and spinal cord - All sensory information must be relayed to the CNS before it can be interpreted and acted upon. |
|
|
Peripheral Nervous System (PNS) - Definition and Composition
|
- Nerve processes that connect the CNS with the glands, muscles, and receptors in the body
Comprised of: - 12 prs. cranial nerves (spinal nerves) - Attached to underside of brain - Conduct impulses between brain and structures in the headm neck and thorax |
|
|
Cerebral Cortex
|
- A part of the brain that drugs act on
- Interprets sensory input, memory, learning |
|
|
Thalamus
|
- Part of the brain that relays sensory date from the cerebellum, spinal cord, and brain stem to the cerebral cortex
- Also responsible for pain perception |
|
|
Medulla Oblongata
|
- Brainstem
- "Centrally acting" drugs (e.g., antitussives) work on this part of the brain - Carries sensory and motor impulses between the brain and spinal cord - Controls vital functions: vomiting, coughing, swallowing, BP, temp, breathing, hunger |
|
|
Hypothalamus
|
- Part of the brain that controls the pituitary gland which in turn controls the endocrine system
- Controls and regulates the ANS |
|
|
Reticular Formation
|
- Part of the brain that contains the reticular activating system which is responsible for waking, sleeping, and consciousness
|
|
|
Neuron -
Definition |
- A nerve cell
- Has a nucleus surrounded by cytoplasm |
|
|
Axons
|
- Part of neuron
- Carry messages away from the cell body - Can be short or long and end in telodendra nerve endings - Synaptic end bulbs |
|
|
Dendrites
|
- Part of neurons
- Receive messages and carry toward the cell body |
|
|
Ganglion
|
- A knot-like network of nerve cell bodies outside the CNS
|
|
|
Afferent Nerve Cells
|
- In the PNS
- Carry information from receptors in the periphery of the body TO the CNS - Sensory |
|
|
Efferent Nerve Cells
|
- In the PNS
- Carry impulses FROM the CNS to muscles and glands - Motor |
|
|
Somatic Nervous System
|
- Under voluntary control
- The brain makes the decision - Stimulates muscle fibers through motor (efferent) nerves - Sends neurotransmissions for action |
|
|
Autonomic Nervous System
|
- Involutary - functions are automatic
- Efferent (motor) nerves to to cardiac muscle, smooth muscle and glands (intestines) - Made up of two divisions: sympathetic and parasympathetic - ANS target tissues usually receive both para- and sympathetic nerve fibers EXCEPT adrenal medulla, sweat glands and hair follicles - these are sympathetic only |
|
|
The ANS Controls Visceral Functions Such As....
|
- GI motility (peristalsis)
- Rate and force of heart beat - Glandular secretion - Pupil size |
|
|
Neurotransmitters
|
- A chemical "bridge" that allows messages to be passed to one or many neurons
- Diffuse across the synapse and bind to post-synaptic neuron |
|
|
Sympathetic (Adrenergic) Neurotransmitters - List
|
-Epinephrine (adrenalin)
- Norepinephrine - Dopamine - Gamma-amniobutyric acid (GABA) |
|
|
Sympathetic (Muscarinic) Neurotransmitters - List
|
- Acetylcholine: sweat glands, smooth muscle of the blood vessels
|
|
|
Parasympathetic (Cholinergic) Neurotransmitters - List
|
- Acetylcholine
|
|
|
Parasympathetic (Cholinergic) Sites/Receptors
|
- Nicotinic: stimulated by low doses of nicotine
- Muscarinic: stimulated by muscarine and parasympathiomimetic drugs **Acetylcholine is the neurotransmitter which stimulates both of these receptors** |
|
|
Sympathetic (Adrenergic) System Receptors - List
|
- Alpha 1: Stimulatory
- Alpha 2: Stimulatory - Beta 1: Inhibitory - Beta 2: Inhibitory - Dopaminergic: tissues and/or organs affected by dopamine |
|
|
General Alpha Description
|
- Causes excitatory or increased activity of their target organ EXCEPT in the GI tract
- Activated primarily by norepinephrine - Epinephrine, however, has a profound effect in fight or flight - Cats are especially sensitive to stimulation of Alpha receptors - vomiting center (medulla oblongata) |
|
|
Alpha 1 Receptors - Details
|
- Blood vessels of the skin and GI tract: contraction of smooth muscles> vasoconstriction> blood goes to heart and skeletal muscle
- Intestine: decreases motility - Glands: decreases secretions - Eye: mydriasis (pupil dilation) - Urinary bladder sphincter |
|
|
Alpha 2 Receptors - Details
|
- Ends of adrenergic neurons> regulate release of norepinephrine**
- Plays a role in general alertness** - Skin and skeletal muscle: vasoconstriction - Pancreas inhibits secretion of insulin |
|
|
General Beta Description
|
- Causes relaxation or decreased activity of their target organ EXCEPT heart muscle
- Beta receptor stimulation of the heart causes increased heart rate and contractility of the heart muscle - This allows increased amounts of blood to leave the heart and it's diverted from inactive organs and to those flight or flight (skeletal, brain, liver) - Activated by epinephrine |
|
|
Beta 1 Receptor - Details
|
- Heartbeat
- Heart> increased rate> contractility, conduction velocity - Stimulation> Tachycardia |
|
|
Beta 2 Receptor - Details
|
- Arterioles (except in skin and bones)/veins: vasodilation
- Trachea/bronchioles: Beta 2 agonists> relaxation of smooth muscle> bronchodilation - Newer drugs are selective beta 2 agonists to avoid also stimulating Beta 1, causing tachycardia - Albuterol, Terbutaline |
|
|
Dopaminergic Receptors
|
Vasodilation> kidneys> heart (coronary) and GI tract (mesentery)
|
|
|
Agonist - Definition
|
- A drug that competes for the same receptor site as another drug or natural substance (neurotransmitter)
- Enhances or stimulates the receptors properties |
|
|
Antagonist - Definition
|
- A drug that competes for the same receptor site as another drug or natural substance (neurotransmitter)
- Does NOT product a physiological effect by itself |
|
|
Pharmacokinetics - Definition
|
The study of how a drug interacts with the body and hoe the body excretes the drug
|
|
|
Drugs Affect the CNS By...
|
- Mimic the effect of neurotransmitters
* Bind to the receptor sites themselves (Direct) *Stimulate release of neurotransmitter from end bulbs but do not bind (Indirect) * Inhibit the breakdown of the neurotransmitter (anticholinesterase agent) |
|
|
Stimulation of Parasympathetic (Cholinergic) Nervous System Causes....
|
**Rest and Digest**
- Decrease in heart rate - Decrease in respiratory rate - Increase in GI activity - Constriction of pupils - Constriction of bronchioles |
|
|
Stimulation of Sympathetic (Adrenergic) Nervous System Causes.....
|
**Fight or Flight**
- Increase heart rate - Increase respiration rate - Decrease in GI activity - Dilation of pupils (increases peripheral vision) - Constriction of blood vessels in smooth muscle - Dilation of vessels in skeletal muscle - Dilation of bronchioles - Increase in blood glucose levels |
|
|
-ergic: Definition
|
Does the work of; stimulates
|
|
|
-lytic: Definition
|
Prevents; tears down the work of
|
|
|
-mimetic
|
Mimics; has a similar effect
|
|
|
Classes of ANS Drugs - List
|
- Parasympatiomimetic = Cholinergic
- Parasympathilytic = Anticholinergic - Sympathomimetic= Adrenergic - Sympatholytic = Antiadrenergic |
|
|
Parasympathomimetic - Definition
|
- Cholinergic agents
- Stimulation of the parasympathetic nervous system |
|
|
Parasympatholytic - Definition
|
- Anticholinergic agents
- Block action of the parasympathetic nervous system |
|
|
Sympathiomimetic - Definition
|
- Adrenergic agents
- Stimulate the sympathetic nervous system |
|
|
Sympatholytic - Definition
|
- Antiadrenergic agents
- Block action of the sympathetic nervous system |
|
|
Parasympathetic/Cholinergic Drugs - Mode of Action and Uses
|
- Stimulate receptor sites mediated by acetylcholine
- Mimic effects of parasympathetic nervous system - Uses: * Decrease intraoccular pressure * Control vomiting * Treat urinary retention * Stimulate GI motility |
|
|
Parasympathetic/Cholinergic Drugs - Examples
|
- Direct: Combine with the cholinergic receptors and mimic the action of acetylcholine
* Pilocarpine + reduces intraoccular pressure * Metoclopramide (Reglan) = controls vomiting; increases peristalsis -Indirect: Inhibit breakdown of acetylcholine * Organophosphate compounds/poisons (toxic) * SLUD = salivation, lacrimation, urination, defecation |
|
|
Pilocarpine
|
- Direct acting cholinergic (parasympathomimetic)
- Reduces intraoccular pressure in glaucoma |
|
|
Metoclopramide
|
- Direct acting cholinergic (parasympathomimetic)
- Trade name Reglan - Controls vomiting; increases peristalsis - Contraindicated in patients with GI obstruction |
|
|
Parasympatholytic / Anticholinergic Drugs - Mode of Action and Uses
|
- Block the action of acetylcholine at the muscarine receptors
- Used for: * Decrease GI motility (V&D) * Preanesthetic to help prevent bradycardia, increase vagal tone, reduce secretions * Dilate pupils for eye exams * Treats sinus bradycardia (large and ahtletic dogs) |
|
|
Parasympatholytic / Anticholinergic Drugs - Examples
|
- Atropine: preanesthetic, decrease secretions, prevents bradycardia, dilate pupils
- Glycopyrrolate: similar to Atropine but does not cross blood-brain barrier; must use this instead of Atropine in rabbits because of natural atropinase - Aminopentamide (Centrine): anti V&D - Pralidoxime (2PAM): reactivates acetylcholinesterase to treat organophosphate toxicity - Propantheline (Pro Banthine): treats diarrhea, urinary incontinence, bradycardia, and to reduce colonic peristalsis in horses |
|
|
Atropine
|
- Anticholinergic (parasympatholytic)
- Contraindicated for certain types of glaucoma - Antitode for organophosphate and MU mushroom toxicities - Crosses blood brain barrier - Preanesthetic to decrease salivary secretions and treat bradycardia - Dilate pupils for ophtho exam and to decrease ciliary spasm - CPCR drug for asystole (flatline) |
|
|
Glycopyrrolate
|
- Anticholinergic (parasympathiolytic)
- Contraindicated for certain types of glaucoma - Longer duration in body than Atropine - Effects similar to Atropine but does NOT cross the blood-brain barrier - Must be used in rabbits instead of Atropine due to natural atropinesterase |
|
|
Aminopentamide
|
- Anticholinergic (parasympatholytic)
- Trade name Centrine - Anti-emetic and anti-diarrheal by decreasing spastic colon |
|
|
Pralidoxime
|
- Anticholinergic (parasympatholytic)
- aka 2-PAM - Reactivates acetylcholinesterase to treat organophosphate toxicity |
|
|
Propantheline
|
- Anticholinergic (parasympatholytic)
- Trade nama Pro-Banthine - Treats diarrhea, urinary incontinence, bradycardia, and to reduce colonic peristalsis in horses to allow rectal exam |
|
|
Sympathomimetic/Adrenergic Drugs - Modes of Action and Uses
|
- aka Agonists
- Action or site mediated by epinephrine or NE - Classified to the specific receptor-type they affect (alpha 1 or 2, beta 1 or 2) - Adverse effects - tachycardia, arrythmias, nervousness - Used for: * Stimulate heart during arrest * Allergic reaction * Glaucoma * Asthma * Prolong local anesthetic * Reverse bronchoconstriction (anaphylactic shock) * Strengthen heart (CHF) * Correct hypotension (vasoconstriction) * Urinary incontinence |
|
|
Sympathomimetic/Adrenergic Drugs - Examples
|
- Epinephrine (adrenalin)
* Anaphalaxis, severe asthma, CPCR * Increases HR and cardiac output; dilates bronchioles * Dilates blood vessels in skeletal muscles * Increases metabolic rate -Norepinephrine (noradrenalin) * Mostly an alpha agonist with some beta effects * Vasopressor (increases blood pressure) - Dopamine * Dopaminergic and Beta 1 receptors; treats shock, CHF, and to increase renal perfusion, increase blood pressure *Ephedrine, Albuterol, Terbutaline are all Beta Agonist bronchodilators |
|
|
Epinephrine
|
-Adrenergic/sympatomimetic
- Synthetic adrenalin - Contraindicated in patients with glaucoma * Increases metabolic rate * Breaks glycogen bonds *TX anaphylaxix, severe asthma, CPCR** * Increases HR and cardiac output * Dilates the bronchioles * Dilates blood vessels in skeletal muscles * Can be cocktailed with local anesthetic to prolong effect |
|
|
Norepinephrine
|
- Adrenergic (sympathomimetic)
- Noradrenalin - Like epinephrine but acts to regulate physiological acts, not related to stress - Mostly an alpha agonist with some beta effects - Vasopressor (raises blood p[ressure) by constricting blood vessels |
|
|
Dopamine
|
- Adrenergic (sympathomimetic)
- Dopaminergic and Beta 1 receptors - At llw doses constricts arterioles in sites other than the brain and kidneys - Increases blood pressure - Used to treat shock, CHF, and to increase renal perfusion |
|
|
Sympathomimetic/Adrenergic Drugs - Alpha 2 Agonist - Mode of Action, Description and Uses
|
- Not controlled
- Used for sedation/tranq - Are reversible - Stimulate the Alpha 2 receptors in the CNS causing a decrease in the level of norepinephrine - Also Alpha 2 receptors on the heart and blood vessels Effects: * sedation, muscle relaxation, analgesia, emesis, thermoregulatory, bradycardia, vasoconstriction - Use for premed or short procedures; makes cats vomit - Must keep environment quiet - ONLY IN HEART HEALTHY patients - Contraindicated in patients with a history of seizures - Cannot use with an anticholinergic |
|
|
Sympathomimetic/Adrenergic Drugs - Alpha 2 Agonist - Examples
|
- Xylazine
- Detomidine (Dormosedan) horses - Medetomidine (Domitor) - Dexmedetomidine (Dexdomitor) |
|
|
Medetomidine (and derivatives)
|
- Adrenergic (sympathiomimetic)
- Alpha 2 Agonist - Detomidine (Dormosedan) horses - Medetomidine (Domitor) - Dexmedetomidine (Dexdomitor) - More potent than Xylazine - Reversal agent is Atipamezole in equal IM - Can give IM or IV |
|
|
Xylazine
|
- Adrenergic (symapathomimetic)
- Alpha 2 Agonist - Trade names Rompun, Anased - Scary drug when monitoring - Reveral agent Yohimbine - 2 concentrations: small animal 2% - 20 mg/ml; large animal 10% - 100 mg/ml - Cattle 10X more sensitive to this drug than horses |
|
|
Sympathomimetic/Adrenergic Drugs - Beta Agonist - Examples
|
- Isoproterenol
- Dobutamine - Terbutaline - Ephedrine - Albuterol |
|
|
Isoproterenol
|
-Adrenergic (sympathomimetic)
- Beta Agonist - Used to reat acute bronchial constriction, cardiac arrythmias (complete AV block) and occasionally for shock and heart failure |
|
|
Dobutamine
|
-Adrenergic (sympathomimetic)
- Beta 1 agonist - Used for short term treatment of heart failure by increasing contractility and rate - Short half life in humans |
|
|
Terbutaline
|
-Adrenergic (sympathomimetic)
- Beta Agonist - Bronchodilation - Relaxing the smooth muscle around airways |
|
|
Ephedrine
|
-Adrenergic (sympathomimetic)
- Beta Agonist - Also used to treat urinary incontinence and topical nasal uses - Bronchodilation - Relaxing the smooth muscle around airways |
|
|
Albuterol
|
-Adrenergic (sympathomimetic)
- Beta Agonist - Bronchodilation - Relaxing the smooth muscle around airways |
|
|
Sympathomimetic/Adrenergic Drugs - Various Examples
|
-Phenylephrine (Neo-Synephrine)
- Phenylpropanolamine (PPA) |
|
|
Phenylephrine
|
-Adrenergic (sympathomimetic)
- Alpha Agonist - Trade name Neo Synephrine - Used as a nasal vasoconstrictor - Helps decrease congestion |
|
|
- Phenylpropanolamine (PPA)
|
-Adrenergic (sympathomimetic)
- Trade name Proin - Thought to stimulate both Alpha and Beta receptors by increasing the release of norepinephrine - Used to treat urinary incontinence in dogs - hormone related in females (typically) |
|
|
Sympatholytic/Antiadrenergic Drugs - Mode of Action and Uses
|
- Adrenergic blocking agents or antagonists
- Classified according to the receptor they block (e.g., Alpha blockers, Beta blockers) |
|
|
Sympatholytic/Antiadrenergic Drugs - Alpha Blockers (examples)
|
- Yohimbine: Reversal for Xylazine
- Atipamezole - Antisedan reversal for medetomidine - Acepromazine - caused vasodilation, decreases seizure threshold, decreases BP - Phenoxybenzamine - hypotensive agent (vasodilation) - Adverse effects include hypotension, tachycardia, etc. |
|
|
Yohimbine
|
-Antiadrenergic (sympatholytic)
- Alpha blocker (aka Alpha 2 Antagonist) - Reversal agent for Xylazine in cats and dogs |
|
|
Atipamezole
|
-Antiadrenergic (sympatholytic)
- Alpha blocker (aka Alpha 2 Antagonist) - Reversal agent for medetomidine, dexmedetomidine, anddetemodine |
|
|
Tolazoline
|
- -Antiadrenergic (sympatholytic)
- Alpha blocker (aka Alpha 2 Antagonist) - Reversal agent for Xylazine (in horses) and Detomidine |
|
|
Phenoxybenzamine
|
-Antiadrenergic (sympatholytic)
- Alpha blocker (aka Alpha 2 Antagonist) - Hypotensive agent (vasodilator) |
|
|
Sympatholytic/Antiadrenergic Drugs - Beta Blockers - Examples
|
- Propanolol
- Timolol |
|
|
Propanolol
|
-Antiadrenergic (sympatholytic)
- Beta Blocker - Used as an antiarrythmic in hyperthyroid cats - Decreases HR, cardiac output and renin release - Adverse effects include bradycardia, hypotension, worsening of heart failure, heart block, syncope (fainting) |
|
|
Timolol
|
-Antiadrenergic (sympatholytic)
- Beta Blocker - Trade name Timoptic - Reduces intraoccular pressure - Ophtho drug for glaucoma - Adverse effects include bradycardia, hypotension, worsening of heart failure, heart block, syncope (fainting) |
|
|
Phenothiazines - General Information
|
- Acepromazine, chlorpromazine
- Not controlled substances - Used as tranquilizer/sedative - Block post-synaptic dopamine recceptors in the CNS - Effects: * Sedation, anti-emetic, anti-arrhythmic, antihistimine - DO NOT use for allergy testing - Possible penile prolapse (permanent) in horses - Can raise seizure threshold - Can cause excitement in some animals, bradycardia, 3rd eyelid prolapse, - Uses: preanesthetic, itching, vomiting - motion sickness, fireworks! |
|
|
Acepromazine
|
**DO NOT exceed 3mg for injectable ever**
- Phenothiazine - Antiadrenergic (sympatholytic) - Alpha blocker - No analgesia - Preanesthetic (one of the most commonly used) - Sedative for fireworks - Causes vasodilation, decreases seizure threshold, decreased blood pressure - Adverse effects: 3rd eyelid prolapse (temp); penile prolapse in horses (perm) |
|
|
Chlorpromazine
|
- Phenothiazine
- Primarily used for it's anti-emetic effects - Can decrease seizure threshold |
|
|
Benzodiazepines - General Information
|
- Diazepam, zolazepam, midazolam
- Controlled Substance Class 4 - Depresses levels of CNS but exact MOA unknown - Effects: antianxiety, relaxes skeletal muscle, anticonvulsant, no analgesia -Uses: restraining agent, sedative, anti anxiety, appetite stimulant - Reveral agent is flumazenil - GIVE SLOW IV; use caution with all but healthy patients - Can cause excitement when used alone - CATS - use brand name valium only!!! - Can cause birth defects in humans |
|
|
Diazepam
|
- Benzodiazepine
- Trade name Valium - Sedative/tranquilizer - Anti convulsant - Comes in concentration 5 mg/ml - Give IV only preanesthetic or oral - Can be absorbed in plastic - Mixed in equal volumes with Ketamine in the same syringe; figure out Ketamine dose first **Should not be mixed with any other drugs** |
|
|
Midazolam
|
- Benzodiazepine
- Trade name Versed - Sedative/Tranquilizer - Anticonvulsant - Unlike diazepam it can be mixed with other agents - Well absorbed IM |
|
|
Zolazepam
|
- Benzodiazepine
- Combined with tiletamine in Telazo - Powder - must be reconstituted - Similar cocktail to Ket/Val |
|
|
Barbiturates - General Information
|
- Phenobarbital, Pentobarbital, Thiopental
- IV cath must be patent or severe tissue reaction perivascular - Controlled substance - Three classes: long acting 8-12 hrs; short 45 min-2 hrs; ultrashort 5-30 min - Give to effect - MOA: CNS depression, inhibit release of ACH and norepi (alertness) - Lipid soluable so no sight hounds -Effects: resp and cardiac depression; cats very sensitive - Uses: sedative, anticonvulsant, anesthetic, Euthanasia solution |
|
|
Phenobarbital
|
- Barbiturate
- Controlled substance - Class 4 - Long acting (8-12 h) - Used for epilepsy, goal to decrease seizure frequency and severity - Long term therapy can cause PU/PD, polyphagia, liver dysfunction (at higher doses) - May be dosed in grains - Dose-dependant respiratory depression |
|
|
Thiopental
|
- Barbiturate
- Controlled substance - class 2 - Ultra short acting (5-30 min) - Used for induction of anesthetic or super short procedures - Thio = sulfur in chemical compound |
|
|
Pentobarbital
|
- Barbiturate
- Controlled substance - Class 2 - Short acting (45 min-2 hrs) - Mostly used to control seizures due to toxins, poisoning (metaldehyde = snail/slug bait) - ALSO one of the main ingredients in euthanasia solutions |
|
|
Euthanasia Solutions Containing Pentobarbital
|
- Trade Names Beuthanasia-D, FP-3, Sleepaway
- Additives for cardiac depression change from class 2 to class 3 drug - Cause death by severely depressing the medullary respiratory and vasoconstriction center - Minor muscle twitching/agonal breathcan occur; anesthetic helps prevent the agonal breath - Solutions are thick so can dilute with warm tap water - Never to be used in food (human or animal) animals |
|
|
Dissociative Agents
|
- Ketamine, Telazol most commonly used in small animal
- Controlled substance Class 3 - NMDA = N-methyl D-aspartate antagonists - Overstimulation of CNS **catalepsis** - Apneustic respiration - Exaggerated reflex responses (laryngeal, palpebral) - Hypersalivation - Increased muscle tone - Lowers seizure threshold - Do not use in animals with head trauma or suspected CSF pressure elevations - IM injection hurts - Do not use in patients with heart, liver or kidney issues, or glaucoma/eye globe issues - For Ket/Val figure out Ket dose first then add the same mL of valium |
|
|
Ketamine
|
- Dissociative
- Controlled substance Class 3 - Often used in conjunction with other drugs, like valium, ace, xylazine - Good for somatic pain, not visceral - Small animal concentraion 100 mg/ml - Ket/Xyl good for horses, not great with small animals |
|
|
Tiletamine
|
- Dissociative
- Trade name is Telazol - Controlled substance Class 3 - Powder form that needs to be reconstituted - Great for use with aggressive animals as well absorbed IM |
|
|
Propofol
|
- Trade names Propoflo and Rapinovet
- Short acting hypnotic unrelated to other anesthetics - MOA not well understood - Must give slow IV - Can cause significant respiratory depression and apnea - No analgesia - Lipid (egg lecithin) based and no preservatives - Rec. use within 6 hrs after opening - Good for sighthounds, patients with cardiac and liver DZ |
|
|
Guifenesin
|
- nickname GG
- Used primarily in equine med (IV) for muscle relaxant effects - Also relaxes laryngeal and pharyngeal muscles - Used as an expectorant in humans |
|
|
Inhalent Anesthetics -
General Information |
- MOA - Unknown
- Most are eliminated through the lungs - Lipid soluable so they quickly leave the blood and enter the brain - Contraindicated in patients with malignant hyperthermia (pigs) |
|
|
Concentration Gradient -
Definition |
- Chemicals move from an area of high concentration to an area of low concentration
- This is a passive process |
|
|
Vapor Pressure -
Defined and Common Inhalents |
- The measure of how readily a liquid transforms into a gas
- Temperature dependent - Tells you how readily the liquid form transforms to gas form in the vaporizer - Agents with a higher pressure evaporate easily, so a precision vaporizer is required Highest to Lowest: * Halothane * Isoflurane * Sevoflurane * Methoxyflurane |
|
|
Solubility Coefficient -
Defined and Common Inhalents |
- Blood/gas coefficient is a measure of the agent's distribution between the blood phase and gas phase
- A desirable agent is less soluble in the blood, making more of it available in gas form to quickly exert its effects on the brain - Lower coefficient > faster induction and recovery Lowest to Highest: *Sevoflurane *Isoflurane *Halothane *Methoxyflurane |
|
|
MAC - Defined and Common Inhalents
|
- Minimum alveolar concentration
- The lowest concentration of anesthetic that produces no response in 50% of the patients exposed to a painful stimulus - Tells you how potent the agent is - Lower MAC > more potent Lowest to Highest: * Methoxyflurane * Halothane * Isoflurane * Sevoflurane |
|
|
Isoflurane - Description
|
- Low solubility; rapid induction and recovery
- High vapor pressure; need precision vaporizer - MAC - less potent than Halothane - Anesthesia maintained at 1.5-2.5% - Smells bad - Low rubber solubility - Low fat solubility so good for kidney and liver issues - Fewer adverse effects on the heart |
|
|
Sevoflurane
|
- Lower vapor pressure than Iso, so needs precision vaporizer
- Vaporizer up to 8%, anesthesia maintained at 2.5-4% - MAC is higher than Iso, so Sevo is less potent than Iso. - Solubility very low so even faster recovery and indiction than Iso - good for masking and chamber inductions - $$$ about 10X more than Iso - Can react with Baralyme and produce Compound A which can cause kidney damage; flush with O2 to rid - Fewer adverse effects on the heart |
|
|
Nitrous Oxide
|
- N2O
- Comes in blue tank - Does not need it's own vaporizer - Always mixed with O2 2:1 ratio; should never be used alone as cannot achieve surgical plane with this alone - Low solubility coefficient so can cause further distension (bad for GDV, pneumothorax) - Never used in a closed anesthetic circuit - Always flush with straight O2 after using nitrous |
|
|
Halothane
|
- As of 8/09, unavailable for more than a year
- Vapor pressure is high so requires precision vaporizer - Moderately low solubility coefficient but higher than Iso and Sevo so induction and recovery takes longer - up to 1 hour for recovery - Moderately fat soluble so about 12% is metabolized by liver and excreted by kidneys - Lower MAC than Iso so more potent; moderate rubber solubility - Biggest problem is it sensitizes the heart muscle to catecholimines (epi) so it may induce arrhythmias |
|
|
Methoxyflurane
|
- Nephrotoxic; prolonged recovery times but cheap
- Solubility coefficient and lipid solubility much higher than Iso and halothane so induction and recovery are slow and about 50% of drug removed by the liver and excreted by the kidneys - Very low MAC so most potent inhalent - High rubber solubility - Requires a preservative that may gunk up the vaporizer - Most potent respiratory depressant of all the inhalents |
|
|
Personality, emotions and fears are the result of what?
|
A balance or imbalance of a wide variety of chemical neurotransmitters
|
|
|
Four behaviours than may benefit from behaviour modifying drugs?
|
- Fears and phobias
- Separation anxiety - Compulsive disorders - Age-related disorders |
|
|
Can drug therapy be used alone?
|
No - drug alone is not enough. They support the behaviour modification that the client still needs to do with the animal.
|
|
|
Three Major Groups of Behaviour Modifying Drugs
|
- Antipsychotic (includes phenothiazines)
- Antidepressant (includes TCA, SSRI, MAOI) - Anxiolytic (includes the benzodiazepine group) |
|
|
How Do Behaviour Modification Drugs Work?
|
They change the concentrations of selected neurotransmitters in the brain with the intent of decreasing or enhancing specific mental activity (increase or decrese the action of a neurotransmitter).
|
|
|
Antipsychotic Drugs
|
- Acepromazine
- Chlorpromazine |
|
|
Anxiolytic Drugs
|
- Benzodiazepines
- Buspirone: has fewer side effects than benzodiazepines; also used to treat urine spraying in cats |
|
|
Antidepressants - TCA
|
- Tricyclics
* Amitriptyline (Elavil)- excessive grooming, spraying in cats, feather plucking in birds * Clomipramine (used for OCD, male aggression |
|
|
Antidepressants - SSRIs
|
- Selective Serotonin Reuptake Inhibitors
* Fluoxetine * Sertaline (Zoloft) * Paroxetine (Paxil) - Used for aggression, OCD, anxiety - These are thought to be safer than TCIs as they have less of a depressant effect on the heart |
|
|
Antidepressants - MAOIs
|
- Monoamine Oxidase Inhibitors
* Selegiline - Anipryl - used to treat K9 cognitive dysfunction (old dog senility) and Cushing's DZ - Works by increasing the amount of dopamine found in select cells in the CNS and enhances dopamine effect. - High abuse potential in racing horses - Also beware of human "drug" shoppers (meth) |
|
|
Synthetic Progestins
|
- Affect hormone levels by inhibiting pituitary secretion of FSH and LH
* Ovaban (megestrol acetate) used in cats for urine, aggression and anxiety * Depo-Provera (medroxyprogesterone) used in dogs for aggressive behaviour; cats for feline psychogenic alopecia/dermatitis - Serious side effects including neoplasia, endometritits, personality changes, DM, PU/PD, weight gain, lethargy, depression, permanent local alopecia, atrophy and depigmentation |
|
|
Antimicrobials - Classification
|
- Spectrum of Activity (type of organism it fights)
- -cidal vs -static (kill vs prevent replication |
|
|
MIC - Definition
|
- Minimum Inhibatory Concentration
- The lowest concentration of drug which will inhibit growth of microorganisms - Pathogen must be susceptible - Drug must reach site of infection |
|
|
Goal of Antimicrobial Therapy
|
Kill or disable with pathogen without killing the host
|
|
|
Antibiotic Resistance - Definition
|
If the MIC is so high that there are significant side effects, the bug is considered to be resistant to the drug
|
|
|
Resistance - General Info
|
- Genetic changes passed on
- Mutation of chromosomes |
|
|
R Plasmid - Definition
|
- Additional piece of DNA responsible for resistance
- Separate from Chromosomes - In bacteria and protozoa |
|
|
How to Prevent Resistance
|
- Appropriate use of drugs - type, schedule, strength, etc.
- Educate clients to follow all instructions and give all meds |
|
|
Residues - Definition
|
- Presence of drug or chemical in animal tissues or food products
- Not degraded by cooking or pasturization |
|
|
Harmful Effects of Residues on Humans
|
- Hypersensitivity
- Killing of beneficial GIT bacteria leading to resistant (pathogenic) bacteria to proliferate |
|
|
Withdraw Time - Definition
|
- Time frame typically in days that drugs must be withdrawn from the animal (that's to be used for food- people or animals)
|
|
|
Bactericidal - Definition
|
A drug that kills outright
|
|
|
Bacteriostatic Drug - Definition
|
- A drug that does not kill outright but prevents replication
- Requires actively dividing cells to work |
|
|
Five Ways Antimicrobials Work
|
- Cell Wall - disrupt and lyse (penicillins, cephalosporins)
- Cell membrane - make leaky (antifungals) - Inhibit protein synthesis (lincosamides, macrolides, tetracyclines and aminoglycosides) - Interfere with critical enzymes or bind with intermediate compounds that bacteria need (Sulfonamide abs) - Impair production of bacterial nucleic acids - RNA & DNA (some antifungals, quinolones) CAUTION as these can also attack mammalian DNA |
|
|
Lipophilic Drugs - Definition
|
Drugs that more easily move across phospholipid cell membranes and into places such as the brain, eyes and prostate
|
|
|
Hydrophilic Drugs - Definition
|
Drugs that finid it more difficult to penetrate the cell membranes
|
|
|
Cross Resistance - Definition
|
When bacteria become resistant to one drug in a class, they most likely becomre resistant to others in the same class (e.g., penicillin and amoxicillin)
|
|
|
Cross Reactivity - Definition
|
When an allergy develops to one drug in a class, you are most likely allergic to others in the same class
|
|
|
B-lactamase
|
An enzyme produced by some bacteria, esp. Staphylococci, that attacks the B-lactam ring of an AB making it resistant to the drug
|
|
|
B-lactam Antibiotics
|
Cephalosporins
|
|
|
Classes of Antimicrobials -
Penicillins |
- Work against some gram - and +
- Bactericidal - Disrupt cell wall - Hydrophilic - Cross reactive - High [ ] in urine so good for UTIs - Hypersensitivity most common adverse effect - May destroy good GIT bacteria, so beware of SUPERINFECTION - DO NOT use in guinea pigs, ferrets, rabbits, hamsters,snakes, birds, turtles, and chinchillas |
|
|
Classes of Antimicrobials -
Cephalosporins |
- B-lactam ab
- Classified by generation (1-3) - Work against some gram - and + Staphylococcus and Streptococcus depending on generation - Hypersensitivity less than penicillin - Superinfection with 1st gen - Examples - Cephalexin, Keflex, Cefadroxil, Clavamox (includes amoxicillin) - Bactericidal - Disrupt cell wall - Hydrophilic - High [ ] in urine so good for UTIs |
|
|
Classes of Antimicrobials -
Aminoglycosides |
- Used to TX serious bacterial infections
- Bactericidal - Act on ribosomal protein production - Highly effective against aerobic bacteria, but NOT anaerobes - Synergistic relationship with penecillins and cephalosporins (they break down cell wall so aminos can attack) - Much broader spectrum coverage - used in parvo puppies - Hydrophilic - Cross resistance not as common as with Penicillins - Can cross placenta and harm fetus - Nephro and oto toxicity - cats esp. sensitive to vestibular ototoxic effects - Ineffective in presence of cellular debris (pus) - Example - Gentamicin, neomycin, streptomycin |
|
|
Classes of Antimicrobials -
Quinolones and Fluoroquinolones |
- floxacin suffix
- Bactericidal - 1st one Baytril, now have Zeniquin, Orbax, Cipro etc. - Disrupts bacterial DNA function - Effective against gram + and - skin, respiratory and UT infections Great for Pseudomonas, not for streptococcal infections - Highly effective against aerobic bacteria, but NOT anaerobes - HIGHLY lipophilic and one of the few good abs for prostate infections - 1/4 of enrofloxacin is metabolized to cipro - DO NOT use in growing dogs as adversely affects developing joint cartilege - May lower seizure threshold - Exceeding label dose in cats can cause changes in retina and blindness - Should be reserved for more severe infections to minimize development of resistance |
|
|
Classes of Antimicrobials -
Tetracyclines |
- Bacteriostatic - NEED functioning immune system
- Commonly used for rickettsial DZs (salmon poisoning, Rocky Mt. spotted fever) - Older drugs: hydrophilic (tetra) - Newer drugs: more lipophilic (doxy); also broader spectrum) - Bind to ribosomes and disrupt protein synthesis - Chelated in the gut by mineral divlent cations (Ca++ - dairy, Mg - antacids, FE - iron supplements, Cu - copper - Lipophilic - Excretion: Enterohepatic Circulation, must reduce dose with renal DZ - Chelation with Ca++ discolors adult teeth (during development) and may slow bone development if given at high doses - Beware of superinfection when given PO - Expired drug becomes nephrotoxic - Fanconi's syndrome - glucose in urine w/o diabetes - Baseni's prone |
|
|
Classes of Antimicrobials -
Sulfanamides |
- Sulfa - 1st antimicrobial to have widespread use
- Can be combined with other drugs to make them bactericidal and increase efficacy - Sulfadimethoxine - Albon: used to treat coccidia; Tribrissen - Inactivate enzymes needed for folic acid synthesis - Bacteriostatic BUT potentiated compounds are -cidal - Lipophilic - Drug of choice for some protozoa (cocci and toxoplasmosis) - Cross placenta - can harm fetus - Significant [ ] in urine so good for some UTIs - CAN CAUSE KCS in dogs, requires lifelong Tx woith cyclosporine (used in human med to prevent rejection in organ transplants) - Can also cause skin reactions (urticaria), thrombocytopenia, leukopenia, anemia - Cats severe salivation if tablet broken |
|
|
Classes of Antimicrobials -
Lincosamides |
- Bacterial protein inhibitors
- Bacteriostatic or -cidal depending on [ ] at infection site - Clindamycin (Antirobe) greaqt for anerobic bacteria (abscesses, deep pyoderma, periodontal DZ) MOA - unknown - Possible neurologic side effects - Metronidazole (Flagyl) used to treat Giardia and anaerobic bacteria (is bactericidal) - Tastes awful |
|
|
Classes of Antimicrobials -
Antifungals |
- TX for superficial (dermatophyte) or deep/systemic (valley fever, aspergillosis - nasal common in German Shep) mycoses
- Most have potentially severe side effects - Azoles/Imidazole derivatives: oral include keto-, itra- and fluconazole; topical micon-, clotrimazole (TX for dermatophytes, yeast - otitis externa) - Griseofulvicin- used to TX dematophytes on cats, dogs and horses; oral particles must be very small to be absorbed in GIT; micro and ultramicrosize formulations; teratogenic in cats: cleft palates, other skeletal, skull and NS defects |
|
|
Drugs that Lower the Seizure Threshold
|
- Phenothiazines (ace, chlorpromazine)
- Alpha 2 Agonists (Xylazine, Medetomidine) - Dissociatives (Ketamine, Tiletamine [Telazol]) - Quinolones (Baytril, Cipro) |
|
|
Nervous System
|
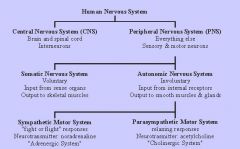
|

