![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
Oedema |
Increased accumulation of fluid (only a clinical sign) Expansion of the interstitial fluid compartment |
|
|
Dependent oedema |
The fluid tends to sink with gravity so that the ventral abdomen and limbs are mainly affected |
|
|
Pitting Oedema |
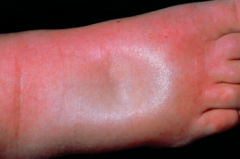
Severe diffuse s/c oedema, a finger pushed into the expanded interstitium leaves an indentation |
|
|
Hydrothorax |
Accumulation of oedema in pleural cavity. |
|
|
Hydropericardium |
Accumulation of oedema fluid in pericardial sac. |
|

Ascites |
Accumulation of oedema fluid in the peritoneal cavity. |
|
|
Anascara |

Severe, generalised oedema involving cavities in subcutis. |
|
|
Starling equilibrium |
At rest, the hydrostatic pressure forces fluid out of the arteriolar end of the capillary to the tissue spaces. At the venous end, the hydrostatic pressure has decreased and osmotic pressure of plasma proteins exceeds venous hydrostatic pressure. Fluid is reabsorbed. |
|
|
Three major factors controlling Starling Equilibrium.. |
a. A Functioning cirulatory system b. A functional lymphatic system c. Serum albumin levels |
|
|
4 Main mechanisms that underpin oedema |
a. Increase in blood hydrostatic pressure b. Increase vascular permeability c. Decrease in plasma colloidal-osmotic pressure d. Lymphatic obstruction |
|
|
Increased blood hydrostatic pressure |
Due to an increase in venous pressure rather than arterial. 2 types: 1. General (L sided heart failure--> pulmonary oedema; R sided heart failure--> generalised oedema) 2. Local (thrombus, tumour) |
|
|
Increased vascular permeability |
Oedema of inflammation!! Opening of interendothelial gaps, allowing leakage of plasma protiens, as well as inflammatory cells. |
|
|
Decreased plasma colloidal osmotic pressure |
A measure of the colloidal solutes to draw water towards them (mainly ALBUMIN). Hypoalbumenia causes decreased plasma colloid osmotic pressure. |
|
|
How does hypoalbumenia arise? |
1. Inadequate albumin production (starvation, chronic liver disease) 2. Net loss of albumin (glomerular disease, loss via GIT) *tends to result in generalised oedema |
|
|
Lymphatic obstruction |
Leads to oedema. Almost always localised because underlying lesion is localised. |
|
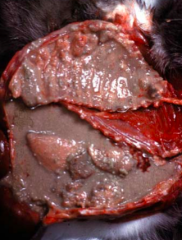
Pulmonary oedema |
Alveoli are kept dry as a result of normal fluid dynamics. 2 causes of pulmonary oedema: 1. haemodynamic 2. microvascular injury |
|
|
Haemodynamic cause of pulmonary oedema |
Due to increased hydrostatic pressure, secondary to L sided heart failure. Blood pushes back to lungs! |
|
|
Microvascular injury cause of pulmonary oedema |
Capillaries in the pulmonary vascular bed are damaged (broken endothelial cells). |
|
|
Pathogenesis of pulmonary oedema |
1. Fluid exceeds capacity of lymphatic drainage 2. Fluid accumulates in interlobular septa, perivascular and peri-airway connective tissue 3. Alveolar walls fill with fluid 4. Alveolar spaces fill with fluid |
|
|
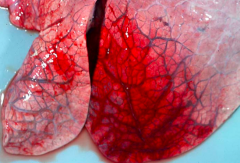
What does pulmonary oedema look grossly? |
Lungs are heavy, wet, exuding red tinged fluid on cut section. |
|

Transudate |
Clear, pale yellow Thin serous 0.05-0.5% protein, albumin No coagulatoin, no fibrinogen Low specific gravity Low cell content Underlying cause: all but inflammation |
|
Exudate |
Dark yellow, red or brown, cloudy/opaque Viscous Usually 2-4% protein Coagulation, Fibrinogen present High Specific gravity High cell content (macrophages, lymphocytes, neutrophils) Underlying cause: Usually inflammation |
|
|
Clinical consequences of oedema |
In brain and lungs can be fatal. Cerebral oedema--> respiratory problems! Pulmonary oedema--> hypoxia! |

