![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
210 Cards in this Set
- Front
- Back
|
What is the structure of the herpes structure?
|
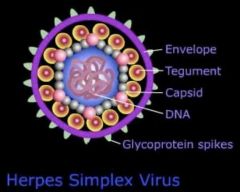
ds DNA of 125-229kbp
icosahedral symmetric capsid 162 capsomeres teguments envelope membrane from host |
|
|
How long can herpes virus remain in its host?
|
lifelong
|
|
|
What is the epidemiology of herpes virus?
|
Around 30-50% middleclass population are infected with herpes.
Whereas 80-100% of pooerer population are infected. |
|
|
How many kinds of human herpes virus are there?
|
8
|
|
|
Describe HHV6 and HHV7?
|
1 in 6 are infected
passed from mother to child Both cause roseola in children infect T cells |
|
|
Describe Kaposi sarcoma associated herpes virus
|
Mostly seen in immunocomptromised patients
|
|
|
Describe Epstein Barr virus
|
Infects B cells and is the main causative agent of infectious monocucleosis (sore throat, fever, fatigue)
|
|
|
Describe Cytomegalovirus
|
Amphitrophic. Mostly affects infants and immunocompromised
|
|
|
Describe HSV1, HSV2, and Varicella-zoster virus
|
Infects skin and nerves, and remains latent in the sensory neural ganglia. HSV causes labial and genital diseases whereas VZV causes chickenpox and zoster (zone of blisters)
|
|
|
Contrast HSV1 and HSV2
|
HSV1 causes less urogenital infections
HSV1 causes more labial infections, ocular keratitis, encephalitis, meningitis => more infections in the head region HSV1 causes less neonatal infections |
|
|
What are symptoms of herpes infection?
|
prodrome of pain
core sore gingivostomtitis |
|
|
How long is the incubation of herpes?
|
2-12 days
|
|
|
What is the treatment for herpes infection?
|
It is self limiting in immunocompetent people
We can use acyclovir, famciclovir, or valacyclovir |
|
|
What causes reactivation of herpes from the sensory ganglia?
|
stress
UV concurrent infections |
|
|
What does herpes look like?
|

Starts as a blister
Develops into crust herpes infection appear along a nerve root (dermatome) |
|
|
How are veneral disease transmitted?
|
Through sex. It requires the warm temperature and the moisture to protect its fragile structure.
|
|
|
How long is the incubation of varicella?
|
14-15 days
|
|
|
Which is more severe: varicella in adult or child?
|
adult
|
|
|
What are the symptoms for chickenpox?
|
fever, chills, myalgia, rash
|
|
|
What is progressive varicella?
|
A rare condition found 10-20% of pregnant women where the virus gets into the lungs, brain and other organs causing pneumonia , meningoencephalitis...
|
|
|
What is zoster?
|
localized recurrence of herpes virus lesion. These lesions are unilateral.
|
|
|
What are the symptoms for zoster?
|
pain, itch, and visible vesicles
|
|
|
What is the epidemiology of zoster?
|
Occurs more in the elderly
|
|
|
Where is VZV laying latent in the body?
|
Spinal ganglion
|
|
|
What is the trigeminal nerve
|
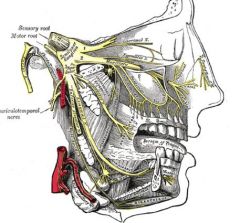
Nerves innervating the face. There are 3 branches; one controlling the eyes, one the cheeks, and one the jaw.
|
|
|
What is the difference in diagnosis between chickenpox and smallpox?
|
chickenpox is more localized in the core of the body whereas smallpox is distributed to the limbs
chickenpox does not leave scars |
|
|
What is the greatpox?
|
syphilis
|
|
|
How do we treat itchiness of herpes infection?
|
Calamine lotion
|
|
|
What is cytomegalovirus?
|
HHV5. A herpes virus which is not known to cause disease in immunocompetent individuals.
May cause rare congenital disease: mental retardation Causes fever, hepatitis, pneumonia in transplant patients Causes retinitis, pneumonia, esophagitis, and disseminated infections in AIDS patients |
|
|
How is CMV spread?
|
Vertically, From mother to child through maternal blood and/or breast milk
|
|
|
What is the epidemiology of the CMV?
|
generally around 60-80% of the population is infected
|
|
|
What is the Epstein Barr virus?
|
HHV4, aka kissing disease.
|
|
|
How is EBV spread?
|
saliva
|
|
|
What is the epidemiology of EBV?
|
90-95% of the population is infected
|
|
|
What is acute infectious mononucleosis?
|
A syndrome mainly caused by EBV:
fever, sore throat lymphadenopathy splenomegaly, hepatomegaly, palatal enanthem, jaundice, rash mononucleosis and atypical lymphocytosis |
|
|
How do we diagnose acute infectious mononucleosis?
|
Monospot test
|
|
|
What is African Burkitts's lymphoma?
|
carcinoma found in EBV infected Africans who are constantly being reinfected with malaria
|
|
|
How is EBV induced infectious mononucleosis characterised?
|
Early excess B cell and late excess T cell
(limited polyclonal B cell lymphocytic leukemia) |
|
|
What is the Kaposi sarcoma virus
|
KSV causes vascular neoplasm mainly found in immunocompromised individuals
|
|
|
Describe HSV life cycle
|
membrane fusion releases nucleocapsid
capsid with tegument migrates using microtubules to nuclear pores DNA is injected into cell nucleus and genome replication occurs in nucleus protein created by mRNAs are delivered into the nucleus and the virus is assembled there constructed virus are released, through the ER, by means of vesicles vesicles membranes fuse with cytoplasmic membrane of the cell releasing the virus |
|
|
Explain the reactivation of herpes virus
|
virus is transported from the cell body of the neuron
virus is released at the terminal end of the axon and reinfects skin cells at the primary locus of infection |
|
|
Describe latency associated trascript
|
Prevents apoptosis of the neuron
|
|
|
What is acyclovir
|
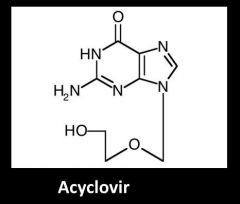
Non phosphorylated guanosine analogue antiviral drug
3' hydroxyl group is phosphorylated by HSV thimidine kinase and becomes incorporated during DNA replicated |
|
|
What is AST a sign of?
|
Liver cell damage/ destruction
|
|
|
What is alkaline phosphatase?
|
Enzyme found in cells that line the biliary tract. When ALP is elevated it signifies obstruction or damage to the hepatic bile ducts.
|
|
|
What is the course of Hepatitis B complication?
|
Acute hepatitis
Chronic hepatitis Cirrhosis Portal hypertension and hepatocellular carcinoma |
|
|
How do we treat portal hypertension and hepatocellular carcinoma?
|
Liver transplantation
|
|
|
What is liver cirrhosis?
|
Fibrotic tissue becomes distributed over the entire liver
|
|
|
How many types of hepatitis are there?
|
6 (From type A to F)
|
|
|
What causes HAV
|
picornavirus ((+)ssRNA)
|
|
|
What causes HBV?
|
hepadnavirus (dsDNA-RT)
|
|
|
What causes HCV?
|
flavivirus (((+)ssRNA)
|
|
|
What causes HDV?
|
delta virus ((-)ssRNA)
This is a satellite virus of hepadnavirus |
|
|
What causes HEV?
|
Calicyvirus ((+)ssRNA)
|
|
|
What causes HFV?
|
unknown
|
|
|
which hepatitis are transmitted through blood?
|
HBV, HCV, HDV
|
|
|
What is the incubation duration for hep A?
|
2-4 weeks
|
|
|
What is the long lasting effects of HAV?
|
There are no long lasting effects of HAV. Its pathology are self limiting.
|
|
|
What are the risk factors for HAV?
|
There is no risk factor for HAV. Most attacks are on younglings of 5-14 years old.
|
|
|
What are the major proteins in hepadnaviruses?
|
S, P, C (,X)
|
|
|
What are the risk factors for HBV?
|
Druggies
Sexually promiscuous people Sharers of intimate personal hygiene products |
|
|
Which part of the body can you find the most HBV ?
|
Blood (serum)
|
|
|
What are the 3 modes of transmission of HBV?
|
sexual
parenteral perinatal |
|
|
Where do we find the most HBV cases?
|
Sub Sahara Africa
Northern South America South East Asia Northern North America |
|
|
How are most chronic cases transmitted?
|
perinatally
|
|
|
What is the rate at which acute HBV virus become chronic?
|
10%
|
|
|
What are some drugs used to treat HBV?
|
Interferon
Lamivudine Adefovir Entecavir Telvivudine |
|
|
How is the HCV genome divided?
|
Structural (5') and Nonstructural (3')
There are 3 major S proteins and several NS proteins that require host and viral protease |
|
|
What are the risk factors for HCV?
|
Drug abusers
Contact with blood |
|
|
Why did HCV infection rate drop around 1988?
|
Blood screen for blood transfusion was available
|
|
|
Describe the progression of HCV from acute to chronic infection
|
Acute symptoms appear
Virus level heightens after 4 weeks Virus level diminishes after 4 months Virus undergoes quiescent phase Virus may reemerge to cause liver cirrhosis and liver cancer |
|
|
What is the rate at which HCV infections become chronic?
|
80-90%
|
|
|
Describe the epidemiology of HCV
|
170,000,000 are infected world wide
transmission is primarily through contact with blood |
|
|
Contrast HBV and HCV
|
HBV transmission rate is high through sex
HBV perinatal transmission is high HBV's progression to chronic is 10% vs HCV's ~85% |
|
|
What are symptoms of acute HCV infection?
|
It is clinically undetectable
|
|
|
How do we treat HCV?
|
IFN alpha injection (with ribavirin in chronic infections)
NS3 protease inhibitor |
|
|
Is HCV curable?
|
It will very soon be curable because combination drug therapies are very successful
|
|
|
Is there a vaccine for HCV?
|
No, HCV elicits too small a response therefore no protective immunity
Moreover HCV mutate easily in antigenic domains |
|
|
What surface antigen does delta virus have?
|
HBsAg (S,M, and L), hepatitis B surface antigen
|
|
|
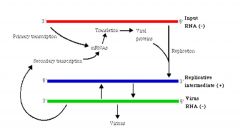
There are two type of RNA products the delta virus genome can make, what are they?
|
Antigenome (+) used to replicate genome
mRNA (+) used to translate into proteins |
|
|
Why is delta virus viroid like?
|
Rolling circle replication
repetitively transcribed into many consecutive tandems self cleavage allows tandem separation |
|
|
What is hepatitis E correlated with?
|
Severe bowel infections
|
|
|
How is hepatitis E transmitted?
|
fecally contaminated water
|
|
|
Where was Hendravirus first found?
|
In horses with flu-like illness in Brisbane
|
|
|
What is the origin of the Hendra virus?
|
Fox bat
|
|
|
How do we rapidly identify emerging infectious agents?
|
Automated PCR
can analyze more than 1,500 PCR reactions in 24 h |
|
|
How did horses get infected by bat derived Hendra virus?
|
Contamination of pasture by bat fetal tissues and fluids
|
|
|
What are the symptoms for Nipah virus infection?
|
fever, headache, drowsiness, pain, nausea, vomiting, weakness, problems with swallowing and blurred vision encephalitis
|
|
|
Where does Nipah virus come from?
|
Bats that suck on tree sap pots on trees
|
|
|
What is the spillover host for Nipah virus? what is it for Hendra virus?
|
Pigs for Nipah virus
Horses for Hendra virus |
|
|
What is the paramyxoviridae?
|
(-)ssRNA virus
|
|
|
Paramyxoviridae have what kind of membrane surface proteins?
|
F (fusion) protein
G (attachment) protein |
|
|
What are the N, L, P proteins of the paramyxoviridae?
|
Transcriptase complex
|
|
|
What is the replicative cycle of the paramyxoviridae?
|
(-) strand makes (+)mRNA
mRNA produces proteins which will turn on full length (+) transcripts (+) are transcribed into (-) strand |
|
|
What is special about the genome of the paramyxoviridae?
|
There are intergenic regions?
|
|
|
What are intergenic regions?
|
These are U filled stretches
When transcribed, the A-U interactions are weak => transcription here is unstable => causes polymerase to fall off or stutter |
|
|
What pathology does Henipavirus cause?
|
chronic meningitis/encephalitis
may remain latent in the brain or lung for a decade |
|
|
Other than Henipavirus, what is another paramyxovirus?
|
Measles virus
|
|
|
What pathology does measles cause?
|
Subacute sclerosing panencephalitis
|
|
|
In which population are subacute sclerosing panencephalitis found?
|
children and young adults (6-15 y.o.)
|
|
|
What are the symptoms for subacute sclerosing panencephalitis
|
progressive psychoneurological deterioration, personality change, seizures, myoclonus, ataxia, spasticity, coma.
|
|
|
How does measle viruses remain undetected by the active immune response?
|
Measle viruses have a membrane fusion protein which allows it to fuse the currently infected cell with another neighbouring cell. This allows it to remain within host cells at all time.
|
|
|
What causes subacute sclerosing panencephalitis?
|
An accumulation of measles capsid in neurons.
This accumulation is caused by a viral mutation that restricts expression of M proteins. Without this protein the virus cannot bud. |
|
|
What pathologies does EBV cause in immunosuppressed patients?
|
nasopharygeal carcinoma, gastric carcinoma, Hodgkin's lymphoma, B cell lymphoma
|
|
|
What pathologies does parvovirus cause?
|
The fifth disease (Erythema infectiosum) in children
Red blood cell aplasia (Reticulocytopenia) |
|
|
What causes MALT non Hodgkin's lymphoma?
|
Bacteria that stimulate prolonged lymphoid proliferation
examples of such bacteria: Helicobacter pylori (gastro) Campylobacter jejuni (small bowel) Chlamydia psittaci (ocular) Borrelia burgdorferi (cutaneous) |
|
|
What pathologies can HCV cause?
|
Marginal-zone lymphoma
|
|
|
What is HTLV 1?
|
ssRNA-RT
|
|
|
Describe the HTLV replication cycle
|
Envelope receptor binding
Capsid entry into cytoplasm RNA reverse transcription Capsid localization in the nucleus DNA integration into host Viral genomic RNA transcription Protein translation Virus assembly Virus budding |
|
|
How can we describe the symptoms relating to non Hodgkin's lymphoma?
|
Different levels of CD4 T cells abundance will lead to different pathologies (from least to most severe):
Burkitt's lymphoma (B cell lymphoma) Immunoblastic (worsened Burkitt's) Primary CNS lymphoma caused by EBV |
|
|
What is HAART?
|
Combination antiviral therapy to treat AIDS
|
|
|
What is the effect of HAART on non Hodgkin's lymphoma?
|
It decreased the rates of non Hodgkin's lymphoma
PS. small decrease in Hodgkin's lymphoma as well |
|
|
What are the symptoms of non Hodgkin's lymphoma?
|
Aggressive B cell neoplasm
High LDH Extranodular presentation |
|
|
What is the Multicentric Castleman disease?
|
B cells hyperproliferate at multiple locations
features: Inability to class switch immunoglobulins HHV8 is present causes: fever and splenomegaly lymphadenopathy Pancytopenia Elevated IL-6 Polyclonal hypergammaglobulinemia |
|
|
What causes Castleman disease?
|
HHV8, HIV and HBV together
|
|
|
What are the two types of Castleman disease?
|
Unicentric - grows at one place
Multicentri - dispersed growth |
|
|
How do we treat Castleman disease?
|
Unicentric - surgical removal
Multicentric - cortisone, Splenectomy, ART, Anti-IL6, Anti herpes drug (ganciclovir and cidofovir), CHOP-Rituximab |
|
|
What pathologies does HHV8 (Kaposi's sarcoma-associated herpesvirus) cause?
|
Karposi's sarcoma
Castleman's disease Primary effusion lymphoma Extracavitary primary effusion lyphoma |
|
|
What are some HHV8 oncogenic factors?
|
LANA-1, v-cyclin, v-FLIP, vIRF-3, v-IL6
|
|
|
What is primary effusion lymphoma?
|
Lymphoma that typically occur in body cavities such as the pleural space, pericardium, and peritoneum.
B cell markers: negative: CD19, Cd20, CD79a,and lack Ig expressions positive: Ki67, CD30, CD138 |
|
|
What is primary CNS lymphoma?
|
Lymphoma in the CNS found in very advanced HIV patients (CD4 <50)
usually EBV positive cerebral nodules |
|
|
How do we treat for Primary CNS lymphoma?
|
ART
|
|
|
What are the two gastroenteritis viral causative agents?
|
Rotavirus
Norovirus |
|
|
What is gastroenteritis?
|
acute infectious syndrome of the stomach lining and the intestine
symptoms: diarrhea, vomiting, abdominal pain, nausea, fever, and chills |
|
|
What can cause gastroenteritis?
|
Viruses- rota virus, adenovirus, calicivirus, astrovirus
Bacteria - E coli, salmonella, shigella, cholera Parasites - Giardia lamblia, Entamoeba histolytica, Cryptosporidium |
|
|
What are the ways by which pathogens induce gastroentritis?
|
toxins
|
|
|
What is the impact of diarrhea on public health?
|
2 million deaths annually of children under 5 years old
|
|
|
What is the treatment for diarrhea?
|
rehydration
|
|
|
What is the difference between Rotavirus, Adenovirus, Calicivirus, and Astrovirus?
|
They cause disease in people of different ages;
Rotavirus - 3-15 months old Adenovirus - 0-2 years old Caliciviruses - all ages Astrovirus - infants, young children and elderly |
|
|
Describe rotavirus
|
non enveloped
iscosahedral capsid with two protein shells (inner, outer) 11 segments of dsRNA |
|
|
How many kinds of rotaviruses are there?
|
7 (A-G)
|
|
|
Is there a vaccine for Rotavirus?
|
Yes, Rotarix and RotaTeq.
|
|
|
What special about the genome of the rotavirus?
|
It has 11 segments and 2 of which have alternative initiation sites
There are 4 non-structural proteins with one of them have one of the alternative initiation |
|
|
How does rotavirus mediate pathology?
|
enterotoxin
|
|
|
What makes up the outer layer of rotavirus?
|
VP4 and VP7
|
|
|
Describe the entry of rotavirus
|
VP4 -> VP8* and VP5*
entry process using VP8* and VP5* loses outer layer double layered particles are released into cytoplasm |
|
|
What can remove the outer layer of the rotavirus artificially ?
|
calcium chelator like EDTA
|
|
|
What does VP5* interact with?
|
integrins
|
|
|
What does the VP8* interact with?
|
sialic acid
|
|
|
What is the role of VP6?
|
to link VP7 to VP2
|
|
|
What is the role of the double layer protein (DLP) ?
|
to transcribe the RNA located in the inner core
|
|
|
What is the role of VP1?
|
It is the RNA dependent RNA polymerase RdRp
There are 4 channels in VP1; 1 channel for template input 1 channel for (+!)RNA output 1 channel for (-) RNA output 1 channel for NTP input |
|
|
What is the role of VP3?
|
guanylyl and methyl transferase
(5' cap adder) |
|
|
What is the role of VP2?
|
It is the capsid
|
|
|
What is significant about norovirus?
|
Account for 90% of nonbacterial gastroenteritis
|
|
|
Describe norovirus
|
Non enveloped
icosahedral virus (+)ssRNA |
|
|
How many types of noroviruses are there?
|
5 genogroups (GI - GV)
|
|
|
Which are the main genotypes of norovirus?
|
GI and GII
|
|
|
What is the Norwalk virus?
|
GI norovirus, the first viral gastroenteroitis causative agent
|
|
|
When is the virus shedded?
|
Before the onset of illness and continues lon gafter the illness
|
|
|
What are the surface proteins of norovirus?
|
S, P1, P2 (from inside to outside)
|
|
|
Describe the replication cycle and transcription process of norovirus
|
(+) genomic RNA makes full (-) transcript
(-) can transcribe full length (+) genomic RNA or subgenomic RNA for proteins |
|
|
What are (+)transcripts capped with in norovirus?
|
On both (+) genomic RNA and subgenomic RNA there is a protein cap called VPg used as a primer for transcription
|
|
|
What is the receptor for norovirus?
|
Histo-blood group antigens found on RBC, gut, respiratory epithelia
|
|
|
What are the major groups of histo blood group antigens
|
ABO, Lewis, and secretor families
|
|
|
What on the norovirus binds the HBGAs?
|
P2 subunit of VP1 surface protein
|
|
|
To which part of HBGA does norovirus bind?
|
ABO - Gal/GalNAc, alpha-1,2Fuc
(Galactose/N-Acetylgalactosamine, Fucose-alpha1,2) Lewis - alpha-1,2Fuc, alpha-1,4Fuc (Fucose-alpha1,2 , Fucose-alpha1,4 |
|
|
What are some host factors affecting susceptibility to norovirus?
|
non secretors are resistant to infection
|
|
|
What are non secretors?
|
Nonsecretors do not have a functional fucosyltransferase 2 gene.
|
|
|
What is the impact of respiratory diseases?
|
16% of death in Canada
18% mortality for children younger than 5 years of age (leading cause) 15% of all cancers in lung cancer 6-7% of world population has asthma 1.8 million deaths annually by TB 3-4 million deaths annually by acute infectious respiratory diesease |
|
|
What are the two types of respiratory infections?
|
Upper and lower respiratory tract infection
|
|
|
Contrast upper and lower respiratory tract infection
|
LRTI leads to lack of breath and 1-2% of these require hospitalization whereas URTI involve typical cold symptoms.
|
|
|
What are the two ways virus can cause pathology?
|
viral factors and immune factors
|
|
|
How do we treat viral respiratory infections?
|
Antivirals
Vaccines Antibiotics (for coinfections) Bronchodilators, corticosteroids |
|
|
What is the main cause of bronchiolitis?
|
Respiratory syncytial virus RSV
|
|
|
How often is there coinfection in respiratory infections?
|
20%
|
|
|
Describe rhinovirus
|
noneveloped picornavirus
(+)ssRNA accounts for 50% of common cold trophic for respiratory epithelium |
|
|
What are the two types of Rhinovirus
|
hRV-A and hRV-B serotypes
|
|
|
What are the receptors for rhinovirus?
|
ICAM1, LDLR
|
|
|
How do we treat rhinovirus?
|
There is no medication available becuase it is self limiting
|
|
|
Describe coronavirus
|
enveloped coronaviridae
(+)RNA accounts for 10-30% of common cold tropic for upper respiratory tract and GI tract |
|
|
Where is coronavirus assembled?
|
golgi
|
|
|
Describe Adenovirus
|
Non-enveloped adenovirdiae
icosahedral capsid dsDNA accounts for 3-5% of infections in children accounts for 2% of infections in adults tropic for respiratory tract, gastroentral, liver |
|
|
Describe Reovirus
|
Non-enveloped reoviridae
icosahedral capsid dsRNA (10 segments) does not cause disease in humans |
|
|
Describe parainfluenza virus
|
Enveloped paramyxoviridae
(-)ssRNA carry HA and NA |
|
|
What is the treatment for parainfluenza virus?
|
There is no medication for parainfluenze virus
|
|
|
What is the difference between parainfluenza virus and influenza virus?
|
parainfluenza virus' genome has one segment
influenza virus genome has 8 segments |
|
|
Describe respiratory syncytial virus
|
enveloped paramyxovirus
(-)ssRNA affects mainly elderly and immunocompromised 2/3 of infants are infected during their first year 90% of infants are infected one or more times by their second year |
|
|
How do we treat respiratory syncytial virus
|
There is no medication
|
|
|
What is the route of infection of RSV?
|
aerosol and direct contact through the nose and eyes
|
|
|
What are the symptoms of RSV infection?
|
rhinorrhea
cough fever bronchiolitis air trapping wheezing pneumonia necrosis of epithelial cells |
|
|
What are the types of RSV?
|
There is only one serotype of RSV
|
|
|
What is a syncytium?
|
A fused cell caused by RSV
|
|
|
What membrane protein mediates entry for RSV?
|
G protein
|
|
|
How does RSV escape active immune response?
|
By heavily glycosylating its G protein and 80% of G protein is secreted to neutralize antibodies.
Moreover the immune response in the respiratory tract is weak. Local IgA response are short lived. Serum antibodies are less effective, having to travel far into respiratory lumen. Infants themselves have a weaker immune system. |
|
|
Describe RSV entry process
|
G protein binds heparin or proteoglycans
F protein fuse membranes |
|
|
What does SH protein do?
|
viroporin and inhibits apoptosis
|
|
|
What do the RSV NS1 and NS2 do?
|
inhibit IFN induction and signaling
|
|
|
Hendravirus is another paramyxovirus. What is its membrane protein and what is its receptor?
|
Its surface protein is also the G protein however its receptor is the EphrinB2 and EphrinB3
|
|
|
Describe the RSV replication cycle and transcription process
|
(-)RNA genome is transcribed into both mRNA and antigenome
(+)RNA antigenome is transcribed back into (-)RNA genome |
|
|
How is virus detected in the cell?
|
RIG I pathway will produce IFNalpha/beta
IFNalpha/beta will activate the JAK/STAT pathway through IFN receptor |
|
|
How is RSV detected in the cell?
|
Extracellular: TLR2/6, TLR4
Endosome: TLR3 Cytoplasm: RIG I |
|
|
How does RSV evade the detection inside the host cell?
|
NS2 inhibits RIG-I and NFkappaB and JAK-STAT pathway
NS1 and NS2 inhibit IRF3 |
|
|
Describe influenza virus
|
Enveloped
(-)ssRNA (8 segments in influenza A, 7 in C) has HA and NA |
|
|
What are the different types of influenza viruses?
|
Influenza A - human, pig, bird, horse
Influenza B - human, seal Influenza C - human, pig Influenza A and B are major causes of human epidemics |
|
|
How many types of HA and NA are there?
|
There are 16 HA and 9 NA
|
|
|
What are the two ways influenza can mutate?
|
Antigenic drift and reassortment
|
|
|
What is a mixing vessel?
|
An intermediate host that express both human and animal influenza virus receptor
for example pig has both human and avian type influenza virus receptors |
|
|
What is the spanish flu?
|
H1N1 which killed 50 million people
high mortality rate in young addults people dies from pneumonia and viral pneumonia caused by immunopathology HA and PB2 contribute to virulence |
|
|
Where did H1N1 come from?
|
From North American avian flu to classical swine flu to human H3N2 and Eurasian avain like swine flue
|
|
|
Describe the influenza virus life cycle
|
Entry through binding sialic acid
Escape from endosome Enters the nucleus Exports mRNA and genomic RNA |
|
|
What is the difference between avian and human sialic acids?
|
Avian - sialic acid alpha 2,3 galactose (GI tract)
Human - sialic acid alpha 2,6 galactose (Tracheal) Pigs - tracheal tissue has both |
|
|
What determines the receptor specificity for the specific sialic acid
|
Receptor specificity is determined by amino acid residues of the HA receptor binding pocket
|
|
|
What is HA maturation?
|
Cleavage of HA0 into HA1 and HA2 by host protease at basic amino acid residue. There is only one protease for a specific locus in each type of tissue.
Influenza viruses with multiple basic amino acids allows infection in different tissues |
|
|
What is the helix bundle?
|
It is a 6-helical structure to pull the two membranes together to cause fusion
|
|
|
What is the influenza polymerase complex composed of?
|
PA, PB1, PB2
PB2 grabs 5' caps of host mRNA PA cleaves the cap PB1 will elongate the viral mRNA using the stolen cap |
|
|
How is the influenza virus assembled?
|
HA and NA binds to lipid raft domain on the plasma membrane
8 pieces of RNA is packaged M1 and M2 completes the assemble and budding |
|
|
What does influenza NS1 do?
|
limit IFN through inhibition of RIG I, PKR/PACT
limit antiviral state of host cell through inhibition of OAS block cellular mRNA maturation and export of premRNA enhance viral mRNA maturation |
|
|
How does antiviral work against influenza?
|
Zanamivir and oseltamivir blocks sialidase to block exit
Amantadine M2 protein to block entry |
|
|
What kind of vaccines are available for influenza?
|
Seasonal flue vaccines
Seed virus Inactivated virus Live attenuated vaccines Highly conserved membrain antigens (M2 protein) |

