![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
65 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is a virus? |
A virus is an infective agent that typically consists of a nucleic acid molecule in a protein coat, is too small to be seen by light microscopy, and is able to multiply only within the living cells of a host. It is an obligate parasite and therefore requires host cell for survival and replication. |
|
|
|
How do viruses work? |
Virus act in a process called the lactic cycle. They attach to the host cell, inject it’s nucleic acid into host cell, replicate’s viral RNA/DNA using the host’s metabolic apparatus, new viral proteins are assembled by host cell and finally the viruses are released via lysis of the host cell. |
|
|
|
Anti-viral Therapies? |
Nucleoside analogues are: Incorporated into viral DNA and inhibit replication. [Nucleoside analogues: These agents can be used against hepatitis B virus, hepatitis C virus, herpes simplex, and HIV. Once they are phosphorylated, they work as antimetabolites by being similar enough to nucleotides to be incorporated into growing DNA strands; but they act as chain terminators and stop viral DNA Polymerase. They are not specific to viral DNA and also affect mitochondrial DNA. Because of this they have side effects such as bone marrow suppression.] |
|
|
|
Human Herpes Viruses |
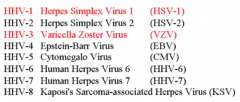
Human Herpes Virus is a very common DNA virus. There are both human and animal forms, and there at least 8 HHV’s that cause human disease. |
|
|
|
HSV1 and HSV2 |
Both HSV-1 (which produces most cold sores) and HSV-2 (which produces most genital herpes) are ubiquitous and contagious. They can be spread when an infected person is producing and shedding the virus. Primary +/- clinical symptoms [e.g. 1' herpetic gingivostomatits] Latency - virus is neurotropic - resides in sensory ganglion e.g trigem Reactivation - e.g. herpes labialis |
|
|
|
Describe the Primary Infection of HSV1/2 |
Direct contact with infected secretions--> Deep epithelial cells become infected --> Infected cells undergo lysis --> Inflammation causes oedema.Thin-walled vesicles form - full of virus --> Vesicles burst and crust over --> Healing. |
|
|
|
Where may the primary infection of HSV1/2 occur? |
Oral - 1º herpetic gingivostomatitis Genital/ rectal - Primary genital herpes Eyes - HSV keratitis Skin - Herpetic whitlow or Eczema herpeticumBrain - meningoencephalitis (rare) of encephalitis (v rare) |
|
|
|
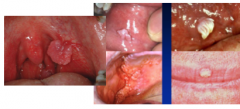
Describe the appearance of primary herpetic gingivostomatits |
Has an incubation period of 3-7. With the associates signs and symptoms of pyrexia, sore throat, fractious [irritable and quarrelsome]. We will see oral vesicles throughout the mouth that rapidly burst and inflamed gingivae (extremely painful with intense inflammatory action and ulcers). With 1ºHG patients may have difficulty eating, speaking and swallowing. As well as drooling and bad breath, and local cervical lymphadenopathy which may last about 10-14 days - usually self limiting. In adults - is primarily sexually acquired |

|
|
|
Management of Primary Herpetic Gingivostomatits? |
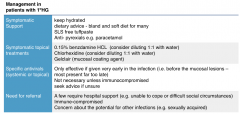
|
Symptomatic support, symptomatic topical treatments Specific Antivirals Antivirals Referral? |
|
|
HSV Latency? |
HSV’s are neurotopic [capable of infecting nerve cells] and infection is lifelong in the sensory ganglion e.g. oral in the trigeminal nerve. It does not replicate in the sensory nerves but can be reactivated from sensory nerves +/- clinical disease. |
Mechanisms are poorly understood - host immunity vs virus virulence. Triggers include - UV [sunshines], stress, menstruation, other illness. More likely if pt is immunoscompromised, |
|
|
Management of Herpes Labialis |
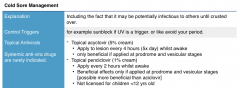
|
Explanation Control triggers Topical antivirals Systemic antiviral drugs? |
|
|
Recurrent Intraoral Hepres Lesions? |
Reactivation of latent HSV infection to give intramural lessons is rare, but does occur. In immune competent people it classically involves - hard palate or attached gingivae (i.e. keratinised mucosa). Can be severe in immunocompromised patients. |
|
|
|
HHV3 |
Varicella Zoater - chicken pocks and shingles(zoster) |
Spread by: Droplets from nasopharyngeal secretions (Chicken Pox). Vesicle fluid (Chicken Pox & Zoster) |
|
|
Iº Infection - chichen pox |
1. Infection of upper respiratory tract – droplet. 2. 1st Viraemia - incubation of ~14 days. 3. 2nd Viraemia - spread to skin and mucosa. 4. Prodrome - few hours to two days start to feel unwell, headache... 5. Skin rash & mucosal lesions. Chickenpox - mucosal - this is oft under diagnosed, vesicles on an erythmatous base rupture to give painful ulcers. Treat symptomatically. |
|
|
|
Describe the skin rash in Chickenpox |
Skin Rash Centripetal [tending to move towards centre] - trunk, scalp, face. Spots appear in crops - lesions at all stages: (7-10 days) itchy macules (flat) papules (raised) vesicles pustules scabs Risk of secondary bacterial infection |
|
|
|
Complications of Primary ZVZ infection? |
Viraemia = potential for systemic disease (particularly immunocompromised) pneumonitis, encephalitis, thrombocytopenia Secondary bacterial infection of scratched skin lesions - septicaemia |
|
|
|
Chickenpox Management |
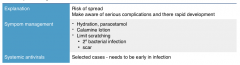
|
Explanation Symptom Management Systemic Antivirals |
|
|
VZV Latency |
VZV is neurotropic, and will reside in the sensory nerves e.g geniculate ganglion (facial nerve).Can be reactivated from nervous tissue. |
|
|
|
VZV Reactivation |
Mechanisms are poorly understood - host immunity vs virus virulence. Triggers include: Malignancy, other illness.......Stress: emotional, surgical. Trauma: localised or generalised. Symptomatic reactivation:< 50Y old: 0.7/1000/year.> 80Y old: 11/1000/year.20% adults have an attack of shingles.1% adults have two or more attacks |
|
|
|
Shingles |
Shingles and zoster, both mean belt. Infection mostly involves a truncal dermatome [an area of skin supplied by nerves from a single root]. Less commonly the head and neck - V1>V2 or V3.Mild systemic illness with low grade fever.skin rash is unilateral (bilateral is rare) |

|
|
|
Shingles - skin rash |
Paraesthesia over affected area. 2/3rds neuralgia - shooting painsPrecedes rash by 2 days - 3 weeks. Vesicular rashForms over 3-5 days.Scabs after 3-7 days.May be extremely painful or barely noticed. Secondary bacterial infection is common.May be mild to severe - look at anatomical distribution. Oral ShinglesThis is rarely observed - probably under diagnosed. Anatomical distribution can be striking. |

|
|
|
What are the complications of Shingles? |
Ophthalmic zoster - Ophthalmic division V nerve.Urgent ophthalmology option is essential Motor Zoster - Ramsay Hunt Syndrome. Post-herpetic neuralgia:Disseminated zoster - Especially immunocompromised |
|
|
|
Ramsay Hunt Syndrome |
Uncommon, but probably under-diagnosed.Geniculate sensory ganglion (VII nerve).Features include:Unilateral lower motor VII palsy.Ear pain.Vesicles involving external ear, soft palate + pharynx.Prognosis is usually good. Note: if you see someone with a facial palsy - always look for vesicles int he external ear and pharynx. |
|
|
|
HHV4 |
Epstein Barr Virus Infection is common and life-long - subclinical in the young, and later in life the higher the socio-economic class. It lies latent in B-lymphocytes. Asymptomatic expression of EBV in bodily fluids can occur intermittently. |
|
|
|
What diseases is EBV [HHV4] associated with? |
Infectious Mononucleosis. Hairy leukoplakia [white patches]. Burkitt’s lymphoma [cancer of lymph nodes]. Nasopharyngeal carcinoma [cancer of epithelial tissue of skin or lining internal organs] |
|
|
|
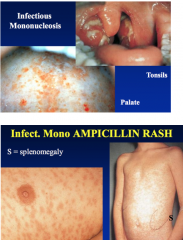
What is Infectious Mononucleosis? |
Glandular fever.Teenagers & young adults from higher socioeconomic groups in affluent societies.Spread via direct contact with infected saliva.Long incubation period - 30-50 days.Systemic illness |
|
|
|
Signs and Symtoms of Mononucleosis? |
SymptomsSore throat, +/- dysphagia.Feel ill - anorexia, malaise, fatigue, headache.. – Associated functional impairment.Recent studies suggest that Fever is probably not as common as was once thought. Systemic Signs Generalised lymphadenopathy - Especially cervical.Splenomegaly (up to 60%).Hepatomegaly (up to 10%) Oropharyngeal signs, rash etc |
|
|
|
Glandular and dentistry? |
Be aware of oro-pharyngeal involvement & functional impairment. Avoid AMPICILLIN and similar drugs. Those with hepatitis + jaundice may be at risk ofProlonged post-op bleed. Impaired drug metabolism. Headache & facial pain may be due to menigoencephalitis |
|
|
|
Hairy Leukoplakia? |
Associated with the EBV infection, affects the borders of the tongue (buccal mucosa). Appears ‘hairy’ or corrugated [ridged/grooved]. Can appear in multiple patches and is seen in the immunocompromised - HIV and transplant patients. |

|
|
|
HHV5 |
Cytomegalo Virus Infection is common and life long. There is no effective vaccine. Asymptomatic expression of CMV in bodily fluids can occur intermittently. The roles in human disease are poorly understood: Glange fever-like illness Reactivated in the immunocompromised - severe CMV during pregnancy is life threatening to the deveoping child |
|
|
|
Glandular Fever Like Illness |
Systemic infection with similarities to IM. Lymphadenopathy is not as marked as IM. Gross tonsillar involvement is unusual. Ampicillin can induce a rash. Serology - rise in antibody titres over 4-6 weeks.Symptomatic management |
EBV – [HHV4] (infectious mononucleosis). CMV [HHV5] HHV6 – rare cause in immunocompetent adults HIV: seroconversion. Toxoplasmosis (protozoan) |
|
|
HHV8 |
Relatively little is known about HHV8 - it was first identified in 1994 from patients with AIDs. It’s role in Kaposi’s Sarcomas remains poorly understood. Thought to accelerate KS development in patients with HIV |
|
|
|
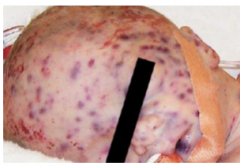
Kaposi's Sarcoma |
Mostly associated with HIV & AIDS. – But, not always. Red/bluish/violaceous macules or raised areas.Can become ulcerated. Usually only painful if ulcerated. Sites: Oral, mostly palate or gingivae. Skin, any site. |

|
|
|
Human Papilloma Virus |
The human papilloma virus is one virus with many different subtypes eg. HPV16. They are a group of small DNA viruses, and humans are the only natural reservoir. It is spread via direct contact: Epitheliotropic and cause epithelial hyperplasia. Some subtypes mostly infect mucosa (oral & genital). Other subtypes mostly infect skin. Infection of the oral mucosa is common and is mostly subclinical, acquisition can occur very early in life. Sexual activity is linked to acquisition rates but is not necessary. HPV can be cleared for the oral mucosa by the immune system, latent HPV can be reactivated. Over 40 types have been identified in the oral mucosa ranging from high risk types (16) to low risk. Transmission to the oral mucosa is by direct contact - this may or not be sexual contact. |
|
|
|
HPV and Cancer? |
HPV 16 and 18 Persistant infection is linked with Cervical, vulvar, vaginal, anal, penile and oropharyngeal cancers |
|
|
|
HPV Infection - oral |
Exophytic Warts [proliferating on the exterior surface of a structure in which the growth originated - basically grows outward]Some may be smooth, others are fronded [leaf like?]May reflect transfer from ant-genital mucosaincreased chance of other STDsMay be a sign of HIV/ AIDs Flat Lesions Focal epithelial hyperplasia (heck’s disease) |
|
|
|
HPV Immunisation and Smears? |
Girls immunised ideally pre sexual debut - HPV16 and HPV18
|
|
|
|
Measles |
Measles is an RNA paramyxovirus Highly infectious, notifiable disease |
|
|
|
MMR Vaccine |
an immunisation vaccine against measles, mumps, and rubella (German measles). It is a mixture of live attenuated viruses of the three diseases, administered via injection. Controversy - papers in the Lancet - many children not immunised this caused outbreaks. |
|
|
|
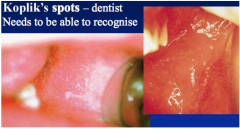
Measles Infection - prodome? |
Fever, runny nose, conjunctivitis, cough. Koplik’s spots - Buccal & labial mucosa.Irregular patches of erythema with a central minute bluishwhite speck:‘grains of salt’. Pathognomonic [specifically characteristic] |
|
|
|
Koplik's Spots? |
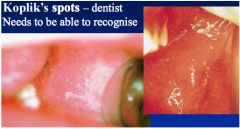
Measles infection Grains of salt |
|
|
|
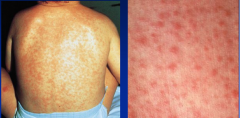
Measles Rash |
Starts on the forehead and neck.Spreads over the next 3-4 days to involve the trunk and then the limbs. |
|
|
|
Early Complications of Measles? |
Measles causes transient immune suppression & increased risk of opportunistic infections. Oral - HSV, Candida, bacterial... Eyes. Pneumonia |
|
|
|
Mumps |
paramyxovirus (RNA), causes a systemic infection - pancreas, CNS, testes and ovaries. |
|
|
|
Symptoms of Mumps |
General Fever, unwell.Meningitis, orchitis, oophoritis, pancreatitis... Sialadenitis [inflamm of salivary gland] Parotid > SMG > SLG. Bilateral or unilateral. Swelling stretches capsule – painful. Decreased salivary flow with risk of ascending secondary bacterial sialadenitis - good OH |

|
|
|
Hand, Foot and Mouth Disease |
Caused by a number of Enteroviruses (RNA) Coxackie A or B viruses Short Prodome - fever, malaise, LN, Sore throat Hands and feet - Vesicular exanthem |

|
|
|
Oral Lesions in HF&MD |
Mostly anterior oral cavity, but can involve any site including lips.Lesions:Vesicular —> crusts.Fewer and less severe than HSV. Herpangina - classically involves the uvula - angina (strangling choking?) v. similar to HFMD |
|
|
|
HIV |
A lentivirus and retrovirus. Virus is lymphotropic and neurotropic. |
HIV infects vital cells in the human immune system such as helper T cells (specifically CD4+ T cells), macrophages, and dendritic cells HIV infection leads to low levels of CD4+ T cells through a number of mechanisms, including pyroptosis of abortively infected T cells, apoptosis of uninfected bystander cells, direct viral killing of infected cells, and killing of infected CD4+ T cells by CD8 cytotoxic lymphocytes that recogniSe infected cells. When CD4+ T cell numbers decline below a critical level, cell-mediated immunity is lost, and the body becomes progressively more susceptible to opportunistic infections. |
|
|
Primary Infection with HIV |
May be asymptomatic or may present with glandular fever like syndrome |
|
|
|
HIV Post-Seroconversion |
can be yrs |
|
|
|
AIDs |
Immunosuppression as CD4 (helper t-lympocytes) counts drop leading to opportunistic infections and neoplasms |
|
|
|
Oral Features of HIV |
Important to recongise and manage. Candida, hairy leukoplakia [EBV], kaposi's sarcoma [HHV8], Non-hodgkin's lymphoma, Perio [NUG] |
|
|
|
HIV and Lymphadenopathy |
This is v. common, may be first indication. Rapid enlargement of previoosuly stable lymph nodes. May be generalised/localised, usually greater than 1mm |

|
|
|
HIV and Candida |
Acute pseudomembranous candidiasis, angular cheilitis and erythmatous candidiasis common. |
|
|
|
HIV and Hairy Leukoplakia |
White/red pathches along lateral border of tongue. These may be corrugated [EBV] More than 25% of HIV+ will develop HL at some point. |
|
|
|
HIV - Warts and Kaposi's sarcoma |
Warts are caused by HPV and Kaposi’s sarcoma is caused by HHV8. |
|
|
|
HIV and Gingivitis/peridontitis |
HIV-associated gingivitis has been renamed linear gingival erythema (LGE) and HIV-associated periodontitis has been renamed necrotizing ulcerative periodontitis (NUP). |
|
|
|
Management of HIV |
Management has been much improved in those living in wealthy countries. There are effective retrovirals that delay progress towards AIDs.HAART [ (Highly Active Anti-Retroviral Therapy] |
|
|
|
Risk of Transmission of HIV? |
Depends on: 1. known HIV infection 2. circumstance where a definite risk is recognised 3. No known HIV infection |
|
|
|
Summary of HSV infections |
Common. Lifelong +/- reactivation. Typically a clinical diagnosis. Management is usually straight forwards. Asymptomatic viral shedding. Cross infection control measures are very important. Potentially serious in immunocompromised |
|
|
|
Summary of VZV [HHV3] |
Common, lifelong. Chickenpox-/+ reactivation – Shingles. Oral involvement often missed. Post-herpetic neuralgia. Asymptomatic viral shedding. Cross infection control measures are very important. Potentially serious, especially in the immunocompromised. VZV immunisation being introduced to those 70Y or older. |
|
|
|
Summary of HPV |
HPV infection of the oral and pharyngeal mucosa is common:Most are infected at some point, but can clear the infections Low risk HPV subtypes can cause clinical lesions such as warts High risk HPV subtypes can cause OPC (which is becoming more common) HPV Immunisation (to reduce cervical cancer) may also help to reduce OPC |
|
|
|
Summary of Measles |
MMR vaccine effective in preventing infection Koplik’s spots. Rash involves head and neck first of all. Risk of secondary infections – e.g. HSV. Highly infectious - cross infection measures. Notifiable disease. Currently a rare infection in the UK, but this could change rapidly in the future. |
|
|
|
Summary of Mumps |
MMR vaccine effective in preventing infection. Sialadenitis of the major salivary glands. Highly infectious - cross infection measures. Notifiable disease. Currently a rare infection in the UK, but this could change rapidly in the future |
|
|
|
Summary of HIV |
Not all those infected with HIV have been diagnosed – importance of best cross-infection practices for all patient care. Oral lesions can be the presenting clinical feature of undiagnosed HIV. Be aware of - and address in your own clinical practice - the issues that can act as barriers to appropriate oral healthcare |
|

