![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
Ventilation vs Respiration |
Ventilation: movement of air into and out of the lungs
Respiration: exchange of gases (O2 and CO2) - happens at tissues, b/w ties and blood, blood and lungs (includes ventilation) |
|
|
Types of Respiration (2) |
1) Aerobic- utilize O2 to break down fuel source
2) Anaerobic- no O2 required for fuel breakdown
Common Fuels: carbs (sugar), fats |
|
|
Tissue Respiration: Aerobic (general) |
- using O2, creating CO2 - Fuel + O2 --> H2O + CO2 - converts ADP --> ATP --> energy source for movement, protein synthesis, ion pumps.. etc (everything)
|
|
|
Rates in Aerobic Respiration
|
- rates at which consume O2 and produce CO2
VO2 (VdotO2)- Oxygen utilization - increases with exercise
VCO2 (VdotC02)- CO2 production - depends on fuel source and metabolism
|
|
|
Carbohydrates vs Fats as a Fuel Source |
Carbs (CHO) - 1 O2 puts 0.7 out - written VdotCO2 = 0.7*VdotO2
Fats (most efficient): - 1 O2 in puts 1 CO2 out - best way to generate ATP - VCO2 = VO2
|
|
|
Anaerobic Respiration |
- ATP production without O2 - mostly occurs when aerobic isn't enough - still have CO2 as a waste - Fuel --> Lactic Acid (decrease ph in blood) - Carbs--> Lactic Acid (La:H) --> La- + H+ (proton contributes to cramps) - augment aeorbic |
|
|
Anaerobic Respiration Cont. Bicarbonate Buffer |
- prevents blood pH fluctuations - H+ + HCO3- --> H2O + CO2 - H+ ion comes from lactic acid, bicarbonate ion free floating in blood |
|
|
Times when you have Anaerobic Respiration (2) |
Intense Exercise - Sore legs come from lactic acid build up, free nerve endings in your muscle sense this change in pH and relay it to brain as muscle sores
Myocardial Infarction - not enough O2 getting to muscle, lactic acid build up sensed by irritant receptors |
|
|
Is Anaerobic Efficient? |
- no - get 2 ATP for every carb - you get 36 ATP if you do aerobic - anaerobic occurs quickly though |
|
|
Mechanisms of Ventilation (Boyle's Law) |
Boyles Law: - PV = k
Breathing In: - increase volume, decrease pressure - expanded thoracic cage - atm pressure is greater than that in the lungs
Breathing Out: - decrease volume, increase pressure - pressure in lungs is higher than atmosphere so air exits
|
|
|
Compliance |
- how easy it is to make your lungs larger - related to elastic nature - a decrease in compliance where there's scar tissue
|
|
|
Mechanisms of Respiration (Dalton's Law) |
- exchanging gas between alveoli and blood and blood and tissues
Dalton's Law - [pressure] x [gas%] = Partial Pressure of gas
|
|
|
Partial Pressure of gas |
- each gas in a mixture gives off it's own partial pressure - dependent on the % that the gas occupies in the environment - diffusion depends on Ppgas |
|
|
Quiet (tidal) Inspiration (Atmospheric vs. Intrapulmonary) |
- increased thoracic capacity due to downward movement in the diaphragm (1-2 cm) - in Adult: 0.5L of air per inspiration (tidal volume) - increasing lungs/thoracic cage, get small difference in airways (2mmHg), enough to drive movement of air into lungs
Atmospheric: 760mmHg Intrapulmonary: 758 mmHg |
|
|
Forced Inspiration (what things are used, how much expansion, what force) |
- Diaphragm (8-10cm) - use of external intercostals (ribs up and out) - use of muscles that fix upper ribs (scalenes, sternocleidomastoid)... around 5-5.5L extra - Hydrostatic Force from pleural fluid that allows lungs to move with the thoracic wall and diaphragm |
|
|
Problem with Hydrostatic Force: Liquid and Air |
Pleural Effusion (Liquid) - when you put extra fluids into the space (ex from infection) - when lung does not follow thoracic wall
Air - bullet goes through, air gets in, lungs collapse, does not follow cage |
|
|
Stitch (Defn and where does it originate from?) |
- intense pain associated with thoracic cage - comes from using the external intercostals to their max when you're not used to using them - since pain originating from cage, it's conveyed by thoracic spinal nerves from intercostal spaces |
|
|
If Diaphragm experiencing intense pain? |
- referred pain to the neck and b.w shoulders - dermatomes of C3, C4, C5 |
|
|
Times When It's Hard to Breathe (3) |
- Pregnancy (limits inferior movement of diaphragm)
- Eating lots of food (Sits under left border of diaphragm)
- Corset (prevents expansion of thoracic cage) |
|
|
Expiration (Quiet vs Forced) |
Quit/ Tidal Expiration - elastic recoil of lungs and musculature (relaxes) - no musculature involved, lungs going back to normal
Forced Expiration - internal intercostal muscles contract - abdominal wall musculature (compress viscera) - muscles that fix inferior ribs (Quadratus Lumborum) pulling down on thoracic cage |
|
|
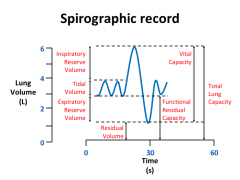
Measuring Lung Volumes (what is used, how it works) |
Spirograph- measures air going in and out of lungs
- when you inspire, the bell sinks and pen rises - when you expire, the bell rises and pen falls
gold standard |
|
|
Total Lung Capacity |
- volume of lungs at maximal inflation - sum of vital capacity and residual volume - in males around 6L |
|
|
Inspiratory Reserve Volume |
- additional volume you bring into the lungs about the quiet breathing that you normally do - up to your max - above your tidal volume |
|
|
Expiratory Reserve Volume |
- after you breathe out as much as possible - breathe out all of your air to your max - need to recruit abdominal muscles |
|
|
Vital Capacity |
- maximum amount of air you can move into or out of your lungs (breathing in and out) - sum of tidal volume, inspiratory reserve volume and functional expiratory reserve volume |
|
|
Residual Volume (and 2 reasons why it's important) |
- the air that lungs have even after you breathe out as much as possible (about 1.5L)
1) Prevent alveoli, trachea and bronchioles from collapsing at the end of an expiration
2) Prevent normoxia/hypoxia cycle --> still have O2 so still able to do gas exchange while breathing out
|
|
|
Functional Residual Capacity |
- Expiratory Reserve Volume + Residual volume - represents all of the air sitting in your lungs after you do a normal tidal expiration - "end tidal volume" - where your system goes into equilibrium --> if someone on a ventilator, you paralyze them to keep them at this volume |
|
|
Spirographic Record (Picture) |
|
|
|
Rates of Ventilation (2 types) |
- similar to cardiac output - dependent on breathing frequency + how much air is moved per breath - Minute or alveolar |
|
|
Minute Ventilation (at rest vs. max exercise) |
- how much air moving past your mouth in 1 minute - VdotE = rate that air moves in and out of mouth - VE = breathing frequency (fh) x tidal volume (Vt)
Rest: VE= 12 breaths/min x 500ml /breath = 6L/min
Max Exercise: 60 breaths/min x 3000mL/ breath = 180L/min
|
|
|
Alveolar Ventilation |
- how much air the alveoli is actually receiving - VA = rate that fresh air moves in and out of alveoli - Less than VE due to dead space volume of lungs (approx. 150mL, need to include in formula, VD = 150mL) - VA always less than VE
|
|
|
Dead Space Volume of Lungs |
- the volume of air occupying the non-respiratory segments of the airways - ex) nose, pharynx, larynx, trachea, bronchi, bronchioles, terminal bronchioles - air that does not participate in gas exchange
|
|
|
At rest equation for Alveolar Ventilation |
- (frequency of breathing) x (Total Volume of air- dead space volume of Lungs)
= fb x (Vt - Vd) = 12 x (500- 150) = 4.2 ml/min
Note: If VT is decreased (eg. chest pain, pregnancy) may need to have higher fb to maintain VA |
|
|
Impedances when Ventilating Lungs (2) |
1) Elastance 2) Resistance |
|
|
Elastance |
- a measure of the stiffness (elastic property)of the lungs - related to the forces needed to blow up a balloon - lungs with high elastance are stiff - slope of P/V is elastance - Elastance = 1/compliance (inversely proportional) |
|
|
Things related to High Elastance (2) |
Fibrosis - lots of scar tissue in lungs (lots of collagen) - resists stretching, not compliant - need greater pressure to get a change in V
Low Surfactant - less surfactant= higher water tension= alveolar collapse - may occur in newborns (since not a lot of surfacant production) |
|
|
Effect of Lung Surfactant on Lung Elastance |
- elastic tissues of lungs are highly compliant - surface tension of water has low compliance compared to lung elastic tissue - water lining alveoli decrease lung compliance - surfactant is a phospholipid released by type II pneumocytes and reduces the surface tension of water --> reduces the pressures needed to breathe --> produced continually after 27-28 weeks gestation
|
|
|
Forces Trying to Collapse the lung (2) |
Elastic Recoil - Each of the lobule (acinus) is wrapped in elastic tissue (part of reason why lung returns to normal when stretched
Water - greatest force of collapse
- 1/3 of elastic recoil property of lung is due to elastic tissue, 2/3 due to layer of water in alveoli |
|
|
Impedances When Ventilating Lungs: Resistance |
- related to the pressure need to generate air flow (essentially the pressure difference "drop" between two sides of a tube) - can be likened to drag which opposes air flow - biggest factor is diameter
|
|
|
Resistance Equation |
Resistance = (P1-P2)/V - The slope of the P V graph - Flow Vdot = Rate of volume in L/s - Need P1 to be higher than P2 for flow to occur (Vdot) - if something is extremely resistant, you need large pressures (large pressure differences) to get flow to occur |
|
|
Pathologies Related to Resistance (2) |
1) Asthma 2) Chronic Obstructive Lung Disease |
|
|
Asthma |
- Radius of vessels become smaller (airways constricted) - airways have to become more resistant, and you need more work (higher pressures) to make the same volume of air go by - recruit SCM and scalene |
|
|
Chronic Obstructive Lung Disease |
- Causes remodeling of airways (more smooth muscle and mucous) making the lumen smaller - makes the airways smaller - will not go away (chronic) |
|
|
Ventilation and Pleural Pressure |
- lung inside thoracic cage (chest wall) and separated from it by the pleural space (that contains a thin layer of serous fluid) - changes in lung volume occur when the muscles of ventilation move the chest wall and produce changes in pleural pressure (lungs follow) |
|
|
Tug of War between Lung and Chest |
- Lung tissue always trying to collapse (since it's elastic) -thoracic is always trying to expand - both pulling on pleural space from either side, results in a negative pressure - known as sub atmospheric pressure/ negative thoracic pressure
|
|
|
How does changes in lung volume occur? |
- when the muscles of ventilation move the thoracic cage, produce changes in pleural pressure - changes intrapulmonary pressure |
|
|
PIP and Ppl |
PIP= Intrapulmonary Pressure (pressure IN the lungs)
Ppl = Pleural Pressure (negative), in the pleural space |
|
|
Positive Ventilation/ Abnormal Way of Breathing/ Mechanical Ventilation |
- lungs inflated by increasing the pressure inside the alveoli (PIP/ intrapulmonary pressure)
- similar to mechanical ventilation of a patient
- increase the pressure and you get an increase in lung volume |
|
|
How We Really Breathe/ Normal Ventilation |
- lungs expanded by reducing the pressure surrounding the lungs to sub-atmospheric pressures (negative pressures) - done by changing the size of the thoracic cage - Pip decreases when lung volume increases, creating a pressure difference that enables us to intake air |
|
|
Breathing cycle : Before Inspiration |
- no breathing taking place, respiratory muscles relaxed - lung volume = functional residual capacity - equilibrium: (PIP -Patm) = 0, no airflow
Forces: - lung elastic recoil tends to make lungs empty - thoracic cage elastance tends to make the chest wall expand
- forces equally matched and results in a negative Ppl (pleural pressure) |
|
|
During Inspiration |

- inspiratory muscles are active, expanding thoracic cage
Forces: - lung elastic recoil makes lungs tend to be empty - thoracic cage elastance recoil makes the thoracic cage tend to expand - muscles forces make the cage tend to expand (disrupts equilibrium)
Result: - pulls lungs outward (larger) - greater lung recoil pressure so Ppl becomes more negative - negative Pip (sub-atm) -Pip overcomes the resistance of the airway and inspiration occurs - As lung expands, PIP becomes sub-atmospheric and air enters the lungs |
|
|
End of Inspiration |
- inspiratory muscles active, holding lung at fixed volume
Forces - Lung elastic recoil is increased due to the increased volume of the lungs - Thoracic cage elastance tends to make wall expand - muscle forces tend to make the chest wall expand - forces are equally matched resulting in and even more negative pleural pressure as these forces "pull" the pleural space
- PIP is zero (equal to atmosphere) and no air flow occurs |
|
|
During Expiration |
- inspiratory muscles inactive, allows passive recoil of the lung to drive expiration
Forces - Lung elastic recoil increased due to increased volume of lungs - thoracic cage elastance tends to make chest wall expand - lung elastic recoil is larger than the outward thoracic elastance, causes the lungs volume to decrease
- as lung volume decreases, PIP increases, causing expiration - as the lung volume continues to decrease, Ppl and lung elastic recoil will also decrease (less negative) |
|
|
When does Ppl become slightly positive? |
- during forced expiration, your lung technically collapsing but as no air can get in the space, everything equilibrates as soon as you stop the forceful contraction - Ppl becomes negative again |
|
|
Summary of Breathing Cycle (PIP vs Ppl) |
PIP - always negative - more negative during inspiration, as you have to make the PIP slightly less than Patm, forcing air in - more positive during expiration, as lung gets smaller, the volume decreases, and PIP increases, forcing air out
Ppl - always negative but fluctuates (helps keep lungs glued to thoracic wall), lung will collapse if not negative - more negative during inspiration - more positive (less negative) during expiration as lungs recoil back to natural shape |

