![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
35 Cards in this Set
- Front
- Back
|
What are ANCA's?
|
Antineutrophil Cytoplasmic Antibodies (serum antibodies to neutrophils)
|
|
|
What are the two types of ANCA's and what do they bind?
|
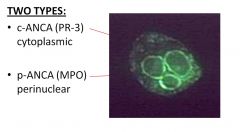
c-ANCAs bind proteinase 3 (Pr-3) located within the cytoplasm
p-ANCAs bind myeloperoxidase (MPO) located in teh perinuclear area |
|
|
What is the hypothetic mechanism of action of ANCAs?
|
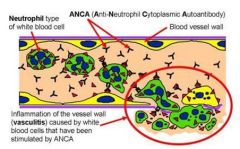
1. ANCAs bind to neutrophils with expressed MPO and PR-3 on their cell surface
2. Neutrophils accumulate in microvasculature 3. Neutrophils degranulate 4. Neutrophil granular content injures vessel wall and induces inflammatory reaction |
|
|
What is the epidemiology of Wegener Granulomatosis?
|
NECROTIZING GRANULOMATOUS VASCULITIS
Adults : any age, ave 50yrs M≥W C-ANCA (PR-3) |
|
What are three key features of Wegener Granulomatosis?
|

1. Granulomatous vasculitis of small vessels
2. Upper airway (especially middle) or lung necrotizing granulomas 3. Kidney lesions (necrotizing glomerulonephritis) |
|

What are clinical manifestations of Wegener Granulomatosis?
|
- Recurrent pneumonia
- Chronic sinusitis - Nasopharyngeal ulcers +/- SADDLE NOSE DEFORMITY -Kidney damage (nephritic syndrome) *Tx with immunosuppression : fatal if left untreated |
|
|
Large Vessel Vasculitides
|
*Granulomatous
- Giant Cell (Temporal) Vasculitis - Takayasu Arteritis |
|
|
Medium Vessel Vasculitides
|
*Anti-Endothelial or Immune Complex
- Polyarteritis nodosa -Kawasaki Disease |
|
|
Small Vessel Vasculitides
|
*ANCA or immune complex
- Microscopic polyangiitis - Churg-Strauss Syndrome -Wegener granulomatosis |
|
|
What is the epidemiology of Microscopic Polyangiitis? (p-ANCA {MPO})
|
Age ~50yrs
M≥F Whites>Blacks *Thought to be hypersensitivity reaction to drugs, toxins, microbes, etc. {Aspirin, penicillin, thiazide diuretics} |
|
|
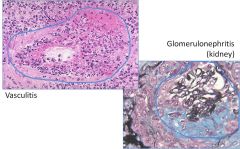
What is the histological feature of Microscopic Polyangiitis?
|
SEGMENTAL NECROTIZING VASCULITIS
-vasculitis without asthma or granulomas - Polymorpho / mononuclear infiltration - Fibrinoid necrosis |
|
|
What are the clinical features of Microscopic Polyangiitis?
|

- SKIN: palpable purpuric rash, lower extremities
- KIDNEYS: Glomerulonephritis (Nephritic Syndrome) - RESPIRATORY TRACT: Sinusitis, pneumonitis, cough, hemootysis - GI Tract: +/- bleeding *Tx by eliminating causative agent *Good prognosis except in lung or kidney involvement |
|
|
What is the epidemiology of Churg-Strauss Syndrome? (p-ANCA {MPO})
|
Adults: Ave age 50yrs
M≥F Very rare (1:1,000,000) *AKA: allergic granulomatosis and angiitis |
|
|
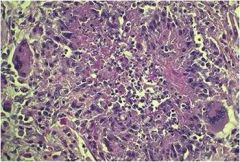
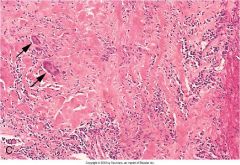
What is the histological feature of Churg-Strauss Syndrome?
|
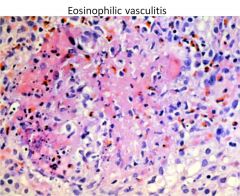
NECROTIZING GRANULOMATOUS VASCULITIS WITH EOSINOPHILS
|
|
|
What are the clinical features of Churg-Strauss Syndrome?
|

*BRONCHIAL ASTHMA
* ALLERGIC PARANASAL SINUSITIS * EOSINOPHILIA - Also, Transient pulmonary infiltrates and purpuric skin rash |
|
|
What is the epidemiology of Polyarteritis Nodosa? (PAN)
|
Young Adults
M≥F 30% Patients have HEPATITIS B ANTIBODIES |
|
|
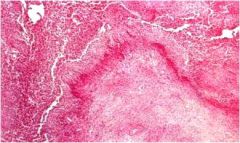
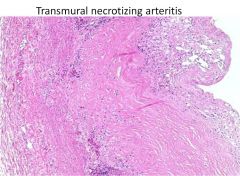
What is the histological feature of Polyarteritis Nodosa?
|
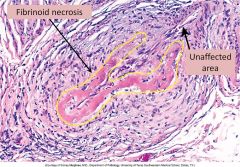
SEGMENTAL TRANSMURAL NECROTIZING ARTERITIS of medium-sized and small MUSCULAR arteries
-sharply segmental, transmural -mixed inflammantion - fibrinoid necrosis -nodular fibrosis (older lesions) * all stages of inflammation and healing may coexist in the same or different vessels |
|
|
Where does Polyarteritis Nodosa affect?
|

-KIDNEYS, GI Tract, Skin
- Causes nodular thickening of the vascular wall - +/- aneurysmal dilation (<0.5cm) with hemorrhage, thrombosis and infarctions in the supplied areas *Pulmonary Vasculature not affected. |
|
|
What are the clinical features of Polyarteritis Nodosa?
|
- KIDNEY: nephritic syndrome, renal failure
- GI Tract: abdominal pain and melena (black feces bc hemorrhage) - Musculoskeletal: diffuse muscular aches and pains - Integument: painful skin, SUBCUTANEOUS NODULES -Systemic: Fever, Malaise, Weight Loss *Tx with immunosuppression *Fatal if left untreated |
|
|
What is the epidemiology of Kawasaki Disease?
|
Infants and Young Children
- Leading cause of acquired heart diseases of children in North America and Japan -Induced by viral or bacterial superantigens - Anti-endothelial antibodies -AKA: Mucocutaneous lymph node syndrome |
|
|
What is the histological feature of Kawasaki Disease?
|
TRANSMURAL NECROTIZING ARTERITIS
- transmural inflammation - progresses to fibrosis and stenosis |
|
|
Where does Kawasaki disease affect?
|
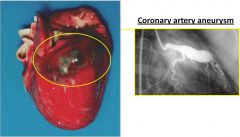
*CORONARY ARTERIES (70% all cases)
* skin, mucous membrane, lymph nodes *Can lead to CORONARY ARTERY ANEURYSM |
|
|
What are the clinical manifestations of Kawasaki Disease?
|
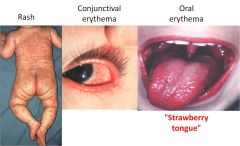
*SKIN RASH, lymphadenopathy, fever, malaise
*Conjunctival and ORAL EROSIONS / ERYTHEMA *Cardiac Manifestations Tx: aspirin and IV gamma-globulin *Disease is usually self limited but cardiac involvement may be fatal due to ACUTE MI OR RUPTURE OF CORONARY ARTERY ANEURYSM |
|
|
What is the epidemiology of Giant Cell (Temporal) Arteritis?
|
Most common vasculitis in adults
F≥ M ~50yrs of age *Cell mediated immune reaction (elastin antigen??) |
|

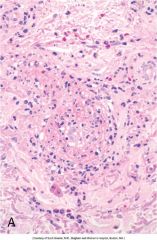
What is the histological feature of Giant Cell Arteritis?
|
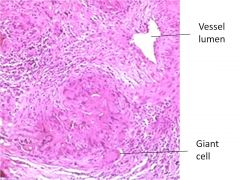
SEGMENTAL GRANULOMATOUS INFLAMMATION
- media and intima - MULTINUCLEATED GIANT CELLS - necrosis and fragmentation of the internal elastic membrane - Later stage: intimal thickening and medial fibrosis |
|
|
What arteries are affected in Giant Cell Arteritis and what is their gross appearance?
|
Cranial arteries
- SUPERFICIAL TEMPORAL -Ophthalmic -Facial Gross appearance: -Segmental nodular thickening - Lumen narrowing +/- Thrombosis |
|
|
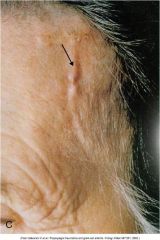
What are the clinical manifestations of Giant Cell Arteritis?
|
- Superficial temporal artery is thickend, swollen and tender
- Unilateral HEADACHE -Ipsilateral visual loss - Polymyalgia rheumatica (pain and morning stiffness in the neck, shoulders and hips) - Fever, malaise |
|
|
How is Giant Cell Arteritis Diagnosed and Treated?
|
Dx: Temporal Artery Biopsy
Tx: Anti-inflammatory drugs (corticosteroids) Prognosis is good: subsides in 6-12 months. Blindness if left untreated |
|
|
What is the epidemiology of Takayasu Arteritis?
|
F>M (F ~90%)
>40 (30) yrs of age - Asians Immune mechanism?? AKA: Pulseless Disease |
|
|
What is the histological feature of Takayasu Arteritis?
|
GRANULOMATOUS INFLAMMATION WITH INTIMAL FIBROSIS
- GIANT CELL GRANULOMAS - Transmural mononuclear inflammation - Later changes: Fibrosis and intimal proliferation |
|
|
What arteries are affected in Takayasu Arteritis and what is their appearance?
|
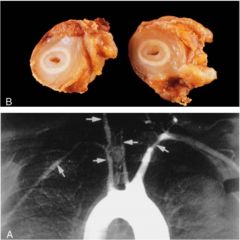
* NARROWING OF AORTIC ARCH AND MAJOR BRANCHES (Subclavian, Carotid)
- Irregular thickening (intimal fibrosis) of the vascular wall - Intimal wrinkling |
|
|
What are the clinical manifestations of Takaysu Arteritis?
|
* Decreased blood flow through carotids and subclavians (pulseless disease)
Tx: Corticosteroids *Prognosis is usually good but is worse with stroke or aortic dissection |
|
|
Henoch - Schönlein Purpura
|
* IgA ASSOCIATED VASCULITIS
* Most common Vasculitis in kids * Follows infection (Viral, Strep A) *IgA & COMPLEMENT IMMUNE DEPOSITS *Involves skin, GI, Renal, Joints *Self - Limited |
|
|
Raynaud Disease
|
*COLD INDUCED VASOSPASM
* Fingers and toes * Part of CREST syndrome * Not really a Vasculitis |
|
|
Thromboangiitis Obliterans (Buerger Disease)
|
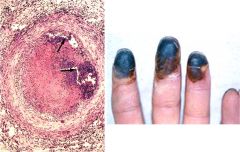
* SMOKERS
* Vasculitis with thrombosis * Involves extremities (Gangrene) * Tx = stop smoking |

