![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
240 Cards in this Set
- Front
- Back
|
What should the patient history include in examination of aneurysms?
|
The hx should focus on recognizing presenting symptoms and identifying risk factors
|
|
|
What symptoms do the majority of aortic aneurysms present with?
|
Most aneurysms are asymptomatic
|
|
|
What presenting symptoms CAN a pt w/ a aortic aneurysm present with?
|
1. Pain
2. Neurologic symptoms 3. Symptoms resulting from decreased blood flow to a organ, or compression of an organ |
|
|
What is the pain from Aortic aneurysms present with?
|
Abdominal, Back or Chest Pain depending on location. Pain is frequently poorly localized and may vary from poorly localized to sharp and tearing when a dissection is occurring.
|
|
|
What symptom will a patient present with if they have blood leaking from an aneurysm?
|
Diffuse pain throughout the abdomen that increases w/ movement
|
|
|
What symptom do pts with a dissecting thoracic aortic aneurysm present with?
|
Neurologic symptoms due to impaired cerebral blood flow
|
|
|
What are the risk factors for developing a aortic aneurysm?
|
1. atherosclerosis
2. family hx 3. HTN 4. Age 5. Male 6. Connective tissue dz |
|
|
What Vascular dz are pts with Marfan's syndrome or Ehler's Danlos syndrome at greater risk of developing?
|
Aortic Aneurysm due to connective tissue disorders
|
|
|
Where is the ascending arch and the aortic arch located? How long are they?
|
In the superior mediastinum and they are both ~5cm long
|
|
|
How wide is the aorta at is origin?
|
~3cm in diameter
|
|
|
Where is the descending thoracic aorta? How long is it? What is its diameter?
|
Located in the posterior mediastinum it is ~20cm long and 2.5 cm in diameter
|
|
|
Where does the abdominal aorta end? How long is it? What is its diameter?
|
The abdominal aorta ends at the 4th lumbar vertebra and bifurcates ~2cm below the umbilicus. It is about 15cm in length and is ~2cm in diameter
|
|
|
What is a aneurysm?
|
A pathologic dilation of a vessel due to weakness of the connective tissue w/in the media of the vessel wall
|
|
|
What is the natural hx/progression of a aneurysm?
|
Enlarges over time at a rate of ~.5 cm per year
|
|
|
What happens to the vessel wall as the radius of a vessel increases over time in a aneurysm?
|
The tension also increases, which causes the vessel to widen further as described by the law of LaPlace
|
|
|
How does the Law of Laplace apply to aneurysms?
|
As the radius of the vessel increases over time, the wall tension (T) also increases leading to further widening
Tension = Pressure x Radius |
|
|
What is a dissecting aneurysm?
|
When a tear in the arterial intima allows blood under arterial pressure to enter the arterial wall and dissect along the connective tissue of the media
|
|
|
Where are dissecting aneurysms more common?
|
They can occur anywhere but they are most common in the thoracic aorta
|
|
|
What is the most common aneurysm?
|
Abdominal Aortic Aneurysm (AAA)
|
|
|
Where do AAAs occur? What is their etiology?
|
Below the level of the renal arteries and are arteriosclerotic in etiology
|
|
|
What does rupture of a AAA lead to?
|
Shock and death
|
|
|
What increases the likelihood of a AAA rupture?
|
Likelihood increases w/ size
|
|
|
What are the probabilities of rupture in pts w/ a AAA > 7cm? >10cm?
|
80% of pts w/ a AAA > 7cm will rupture
95% of pts w/ a AAA > 10cm will die from rupture |
|
|
What are the presenting symptoms of pts w/ a AAA?
|
Often asymptomatic and cause no discomfort to the pt until they rupture.
SOME pts complain of lower back discomfort, abdominal pain or show signs of embolization to the lower extremities |
|
|
What is the risk of rupture in pts w/ a AAA of 5cm or less?
|
Risk of rupture is low enough that they can be followed over time for enlargement w/o the immediate need for surgical repair
|
|
|
How can you estimate the size of a AAA on physical exam?
|
Aneurysms >5cm are palpable on exam ~80% of the time and aneurysms <5cm are much more difficult to detect
|
|
|
How can a AAA be detected on physical exam?
|
The AAA is a expansible mass that pushes the examiners hands apart, the mass often lies to the left of the midline b/e the xiphoid and the umbilicus
|
|
|
What does the presence of an expansile mass indicate? what does the absence of an expansile mass indicate?
|
The presence of a expansile mass STRONGLY indicates the presence of a AAA but the absence of the mass means little b/c up to 78% of pts w/ AAAs lack a pulsatile mass
|
|
|
What does a midline pulsatile mass detected below the level of the umbilicus indicate?
|
Strongly indicates a AAA
|
|
|
What sound is associated w/ a AAA?
|
~1/3 of abdominal aortic aneurysms will be associated w/ a systolic bruit on auscultation
|
|
|
What pathologies are caused by a aneurysm of the ascending aorta?
|
Aortic regurgitation due to distortion of the aortic annulus and the separation of the aortic valve cusps
|
|
|
What are the presenting symptoms of a pt w/ a aneurysm of the aortic arch?
|
1. Dyspnea
2. Hoarseness 3. Cough 4. Hemoptysis 5. Anterior/Posterior Chest pain |
|
|
What is "tracheal tug"? What causes it? What pathology is this diagnositc of?
|
Tracheal tug is a palpable up and down movement of the trachea w/ each heart beat. It is caused by depression of the left mainstem bronchus by the aneurysm. It is diagnostic of a Aortic Arch Aneurysm
|
|
|
How can you detect tracheal tug?
|
By palpating the trachea in the suprasternal notch or by grasping the cricoid and applying slight upward pressure
|
|
|
What blood pressure readings are diagnostic (or at least suspcicious) of a aortic arch aneurysm?
|
Discrepant blood pressure readings or unequal pulses b/e the two arms
|
|
|
What is the most common aneurysm of the thoracic aorta?
|
Aneurysm of the Descending Thoracic Aorta
|
|
|
What presenting symptoms will a pt with a descending thoracic aortic aneurysm have?
|
1. Chest pain in the back b/e the scapula
2. Hemoptysis from leakage of the blood into the lung |
|
|
What kind of pain do dissecting aneurysms of the thoracic aorta cause? How will the pain vary?
|
EXCRUCIATING, tearing, anterior chest pain that may be referred to the back as the tear migrates.
Pts may describe an intensification of the pain w/ each heartbeat |
|
|
What pulse abnormalities may occur from a dissecting aneurysm of the thoracic aorta?
|
Loss of peripheral pulses may occur as the circulation to any major artery arising from the aorta is compromised
|
|
|
What aneurysm can cause ischemic neurologic symptoms? Why?
|
Dissecting Aneurysms of the Thoracic Aorta can cause neurologic symptoms from impaired cerebral blood flow due to invovlement of vessels leading to the head
|
|
|
What Head/Neck symptoms are caused by dissecting aneurysms of the thoracic aorta? why?
|
Pressure on the recurrent laryngeal nerve may lead to hoarseness while pressure on the superior cervical ganglion's preganglionic sympathetic nerves may lead to Horner's Syndrome
|
|
|
What cardiac pathologies can be caused by dissecting aneurysms of the thoracic aorta?
|
dissecting aneurysms of the thoracic aorta cause aortic regurgitation which may lead to SUDDEN onset of CHF and Cardiac Tamponade
|
|
|
How can Aortic dissections be classified?
|
By focusing on whether the ascending aorta is involved
|
|
|
How are ascending aortic dissections treated? How are descending thoracic aortic dissections treated?
|
Ascending are treated surgically while descending are treated medically
|
|
|
What causes sudden (acute) arterial occlusion?
|
Blood clots or atherosclerotic plaque dislodging from the vascular system and migrating downstream as an embolus to occlude a distal vessel w/in one of the lower extremities/ internal organs
|
|
|
Where do most emboli come from? where do the rest come from?
|
Most come from mural thrombi w/in the heart, the rest come from atherosclerotic plaque w/in a large artery (aorta)
|
|
|
What are the signs and symptoms of sudden arterial occlusion?
|
*the 5 P's*
1. Pain: due to ischemia of muscles/nerves 2. Pallor: and coldness of the involved limb 3. loss of Peripheral Pulses 4. Paresthesias: from sensory nerve ischemia 5. muscle weakness and Paralysis: from motor neuron/muscle ischemia |
|
|
What will result if blood flow is not restored after a sudden arterial occlusion?
|
Gangrene or organ infarction
|
|
|
What symptom do microemboli to the lower extremities cause?
|
"Blue toe syndrome"
|
|
|
What is "blue toe syndrome"?
|
Multiple recurrent microemboli occlude the smaller digital arteries in the toes, w/o affecting the larger pulses in the feet. Toes are blue/purple when the foot is in a dependent position (feet lower than body). Pain in toes also occurs.
|
|
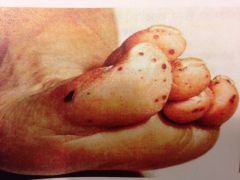
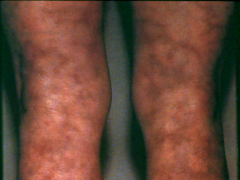
What's the dx? et?
|
"Blue toe syndrome" caused by microemboli to the lower extremities
|
|
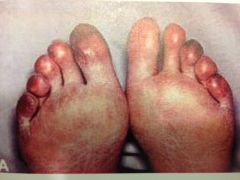
What's the dx? et?
|
"Blue toe syndrome" caused by microemboli to the lower extremities
|
|
|
What should the pt. hx. include in syndrome of chronic arterial occlusion?
|
The hx should explore both the type and location of the pain
|
|
|
What is the pain from chronic arterial occlusion typically described as?
|
Aching or cramping pain, sometimes pts may complain of fatigue of the lower limbs rather than pain when exercising
|
|
|
What part of the HPI is PARTICULARLY important for pts w/ chronic arterial occlusion?
|
The aggravating and alleviating factors
|
|
|
what are the aggravating and alleviating factors of syndrome of chronic arterial occlusion?
|
Exercise induces the pain, rest relieves the pain
|
|
|
What risk factors should be explored before definitively confirming a dx of syndrome of chronic arterial occlusion?
|
You should look for risk factors related to the condition and ask questions to rule out other causes for lower extremity leg pain => including trauma, tumors, venous blood clots infections etc
|
|
|
What is arteriosclerosis obliterans?
|
A dz where ischemia results when the arterial lumen is gradually and progressively occluded by the build-up of atherosclerotic plaque
|
|
|
What is the most common cause for syndrome of chronic arterial occlusion?
|
Arteriosclerosis obliterans
|
|
|
What region of the body is most commonly affected by arteriosclerosis obliterans?
|
The lower limbs
|
|
|
What vessel is most commonly affected by arteriosclerosis obliterans? What are the second most common sites that are affected?
|
Superficial femoral artery is the most commonly affected.
The distal aorta and its bifurcation are the second most common sites of involvement |
|
|
What is the term for the pain in pts w/ chronic arterial occlusion?
|
Intermittent claudication
|
|
|
What is intermittent claudication?
|
A crampy muscle pain that develops in a limb during exercise (walking) as a result of ischemia
|
|
|
What resolves intermittent claudication pain? What produces the pain?
|
The pain resolves w/in minutes if the exercise is discontinued
The amount of exercise necessary to produce the pain is usually constant for any given pt and decreases as the vascular obstruction worsens |
|
|
What is the most common presenting symptom of pts w/ chronic arterial occlusion?
|
B/c the superficial femoral artery is the vessel most commonly involved, calf muscle claudication is the most common symptom
|
|
|
What presenting symptom will occur in pts w/ obstruction of the aorta or iliac arteries?
|
Claudication in the buttocks and thigh
|
|
|
What is rest pain? What does this indicate?
|
Muscle pain that occurs at rest, it is an ominous sign that chronic arterial occlusion as almost totally occluded the artery
|
|
|
What is Leriche syndrome? What does it occur in?
|
Bilateral aorta-iliac occlusive dz that occurs in syndrome of chronic arterial occlusion
|
|
|
What dz will vasculogenic impotence occur in?
|
May occur in conjunction w/ claudication in syndrome of chronic arterial occlusion
|
|
|
What does the absence of both pedal pulses indicate?
|
Strongly indicates the presence of chronic arterial occlusion
|
|
|
Why should you be careful in interpreting findings related to the absence of peripheral pulses?
|
~12% of the pop. has a congenital absence of both dorsalis pedis pulses
~5% of African-Americans have the congenital absence of the posterior tibial pulse ~.5% of the gen. pop. has the congenital absence of both posterior tibial/dorsalis pedis pulses |
|
|
What does the presence of symmetrically strong peripheral pulses indicate?
|
It EXCLUDES the dx of peripheral arterial occlusive dz
|
|
|
What effect does gradual decrease in arterial supply to a tissue have?
|
Normal arterial supply has a trophic (nourishing) influence on tissues, so a gradual decrease in arterial supply may result in trophic changes to that organ
|
|
|
What trophic changes may result from diminished blood supply to a tissue?
|
1. thinning and increased shininess of the skin
2. loss of hair 3. thickening of toenails 4. cutaneous ulcerations w/ eventual gangrene |
|
|
What symptoms are not very specific or sensitive for chronic arterial occlusion?
|
1. thickened toe nails
2. loss of hair 3. thinning/ increased shininess of skin |
|
|
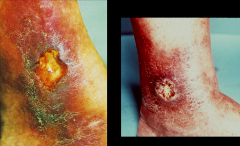
What trophic change from diminished blood supply to a tissue is HIGHLY specific (> 99%) for chronic arterial occlusion?
|

Cutaneous ulcerations and foot sores on the ankles at or below the level of the malleoli heels and tips of the toes
|
|
|
What can cause foot sores that develop from nerve damage?
|
Diabetes can cause neuropathic ulcers
|
|
|
Where do neuropathic ulcers typically occur? what Sy are they accompanied w/?
|
On the soles of the feet over the metatarsal heads and are accompanied by decreased cutaneous sensation in a stocking-glove distribution.
|
|
|
How can you tell whether foot sores are caused by diabetes (neuropathic ulcers) or chronic arterial occlusion (cutaneous ulcerations)?
|
The presence of normal cutaneous sensation in the feet excludes nerve damage as a cause for cutaneous ulceration. SO pts w/ diabetes will have lost sensation, pts w/ occlusion will still have sensation
|
|
|
Where do the ulcers from chronic venous dz occur?
|
Anywhere below the knee but are extremely rare on the soles of the feet! Most venous ulcers occur ABOVE the medial malleoli and are associated w/ edema, varicose veins and increased cutaneous pigmentation.
|
|
|
What is the dx if there is a limb bruit in the limb that has a ulcer?
|
Chronic arterial occlusion
|
|
|
What produces pallor and cyanosis in a limb?
|
When arterial flow is markedly reduced.
|
|
|
When does pallor occur? cyanosis?
|
Pallor occurs when the limb is elevated above heart level.
Cyanosis develops when hemoglobin oxygen saturation declines w/in the sluggish circulation of the limb when held in a dependent position. |
|
|
What is delayed capillary filling?
|
Delayed capillary filling greater than 5 seconds in the cutaneous vascular bed of the great toe develops w/ severe chronic arterial occlusion.
|
|
|
What can happen to the calf muscles in prolonged arterial dz?
|
They can atrophy
|
|
|
What can the occlusion of the arteries produce sound-wise?
|
Systolic bruits may be present.
|
|
|
What is the ankle-brachial index?
|
A good bedside screening test for the presence of chronic peripheral arterial dz.
|
|
|
How do you perform the ankle-brachial index?
|
Place a BP cuff around the calf, the systolic pressure is determined in the foot by listening w/ a hand-held Doppler device over the dorsalis pedis or posterior tibial arteries. Then use the doppler in the brachial artery.
The BPsys in the foot is divided by the BPsys in the brachial artery. Normally the ratio is greater than 1. |
|
|
What does a ankle-brachial index less than .97 mean?
|
Peripheral artery dz is probably present
|
|
|
What does a ankle-brachial index less than .5 mean?
|
consistent w/ limb-threatening ischemia.
|
|
|
What does a ankle-brachial index b/e .5 and .8 mean?
|
Consistent w/ dz severe enough to produce claudication. (cramps)
|
|
|
What does an ankle-brachial index greater than 1.3 mean?
|
Implies stiff, noncompliant vessels.
|
|
|
What is the end result of cerebrovascular dz?
|
Stroke.
|
|
|
What is a stroke?
|
An acute neurologic injury due to one of four main processes involving blood vessels in the brain.
|
|
|
What are the four processes that cause a stroke in the brain?
|
1. Hemorrhage
2. Embolization 3. Thrombosis 4. Vasospasm |
|
|
What is the most common cause of strokes?
|
Embolization
|
|
|
What is a hemorrhage?
|
A burst aneurysm in the brain.
|
|
|
What is a thrombosis?
|
A clot that formed w/in the vessel AT the location the stroke occurred.
|
|
|
What is a embolism?
|
A blockage (clot, bubble, etcetera) that traveled from its origin to block an artery in a different spot.
|
|
|
What is vasospasm?
|
Spasming vessels from drugs, especially cocaine, the spasms cause vessel occlusion.
|
|
|
When a cerebral emboli originated in the heart what disorder probably caused it?
|
1. ATRIAL FIBRILLATION
2. a mural thrombosis following a MI 3. MV prolapse 4. infective endocarditis |
|
|
What dz is present when cerebral emboli originated from the carotid arteries?
|
Atherosclerotic artery occlusive dz is present.
|
|
|
Where does atherosclerotic artery occlusive dz typically occur in pts that had a cerebral emboli?
|
Typically originate from the internal carotid artery, dz is less common in the common carotid artery.
|
|
|
What are the manifestations of carotid artery occlusive dz on exam?
|
Decreased carotid artery pulsations and carotid artery bruits.
|
|
|
What are the features of carotid artery bruits? what other sound must they be distinguished from?
|
Carotid bruits are loudest in the neck and decrease in intensity toward the chest. Transmitted murmurs are loudest in the chest and decrease in intensity toward the neck.
Carotid artery bruits must be distinguished from transmitted cardiac murmurs. |
|
|
What does the presence of an asymptomatic carotid bruit do in middle-aged adults? elderly adults?
|
Increases the risk of stroke by three times in middle-aged adults. In elderly adults they already have a near normal risk of stroke even when asymptomatic, so being asymptomatic when you're middle-aged simply brings you up to the level of the elderly.
|
|
|
What pathology combination indicates that the underlying stenosis is severe in the presence of a carotid artery bruit?
|
When the carotid artery bruit is located in a pt w/ carotid-territory cerebrovascular symptoms. But this is not a super-reliable test.
|
|
|
What physical exam should be performed in pts w/ carotid bruits?
|
Both the carotid arteries should be palpated w/ care in order to not dislodge atherosclerotic plaque.
|
|
|
Where does the carotid bifurcation lie?
|
At the level of the upper border of the thyroid cartilage.
*internal carotid artery itself is anatomically inaccessible to palpation. |
|
|
What is a transient-ischemic attack (TIA)?
|
A single episode of focal neurologic deficit that lasts less than 24 hours and then resolves. If the signs or symptoms persist for longer than 24 hours, an ischemic stroke w/ infarction has occurred.
|
|
|
What Sy do Pts w/ TIA or Stroke involving the carotid circulation present w/?
|
1. Weakness of contralateral face, arms and legs
2. Sensory impairment over same area. 3. Transient monocular blindness on the ipsilateral side due to involvement of the ophthalmic artery 4. Contralateral homonymous hemophilia. |
|
|
What Sys do Pts w/ TIA or Stroke involving the vertebral artery circulation present w/?
|
Dizziness, numbness of the ipsilateral face and contralateral limbs, dysarthria and diplopia.
|
|
|
What sound is vertebral artery occlusive dz associated w/ sometimes?
|
A audible bruit over the upper cervical spine.
|
|
|
What is homonymous hemianopsia?
|

Visual field loss on the left or right side of the vertical midline. Basically it is vision loss on the same side of both eyes. SO if you had a stroke/TIA on the right you would have vision loss on the left.
*above: Paris viewed in a pt w/ left homonymous hemianopsia. |
|
|
What do TIAs resulting from basilar artery insufficiency present w/?
|
Bilateral motor and sensory impairment in the limbs (long tract signs), cranial nerve dysfunction and cerebellar signs.
|
|
|
What causes Raynaud's phenomenon?
|
Vasospasm of arteriolar smooth muscle.
|
|
|
What dz'es cause Raynaud's phenomenon?
|
Underlying collagen vascular dz (SLE, scleroderma), occupational trauma, occlusive arterial dz and drugs.
|
|
|
What is Raynaud's dz?
|
An idiopathic cause of Raynaud's phenomenon.
|
|
|
What are the symptoms of Raynaud's phenomenon?
|
The fingers and/or toes become pale distal to the MCP/MCT joints as a result of spasm of the digital arteries.
|
|
|
What are the three phases of Raynaud's phenomenon in order? How long does the whole sequence of events take?
|
The phases are the white phase, the blue phase and the red phase. The whole sequence of events can last from minutes to hours.
|
|
|
What causes the pallor seen during the white phase of Raynaud's phenomenon? what precipitates the phenomenon?
|
Vasospasm and is usually precipitated by exposure to cold or emotional stress. The pt. may have feelings of cold and numbness in their digits.
|
|
|
What causes the cyanosis seen during the blue phase of Raynaud's disease?
|
Oxygen desaturation occurs from sluggish blood flow w/in the constricted arterioles.
|
|
|
What causes the red seen during the red phase of Raynaud's phenomenon? What symptom other than the redness do pts experience during this phase?
|
Vasodilation producing hyperemia during this final stage the pt complains of throbbing pain in the digits.
|
|
|
What can Raynaud's phenomenon lead to on rare occastions?
|
Digital ulceration and gangrene.
|
|
|
What is Livido Reticularis? Where does it occur?
|
A lacy bluish discoloration of the skin that outlines the areas of normal appearing skin. It occurs over the distal limbs in young men and women.
|
|
|
What may cause livido reticularis?
|
Constriction of arterioles followed by stasis and dilation of capillaries and venules that become filled w/ desaturated blood.
|
|
|
What causes the lacy/fishnet appearance of livido reticularis?
|
It reflects the anatomic arrangement of the vessels.
|
|
|
What part of the body is affected more often by livido reticularis?
|
The lower limbs.
|
|
|
What makes livido reticularis more prominent? less prominent/better?
|
The pattern becomes more prominent upon cold exposure and may resolve with warming.
|
|
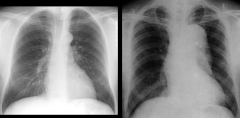
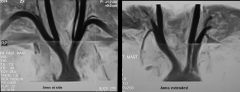
What's the dx?
*normal is on left |
Dissecting Aortic Aneurysm
|
|

This condition happened suddenly, the pt experienced severe pain and there is no pulse in the dorsalis pedis artery. The pt has sensory loss in the white area and paralysis of the toes on dorsiflexion. What's the dx?
|
Sudden arterial occlusion
|
|

What's the dx?
|
Occlusion of the internal carotid artery
|
|
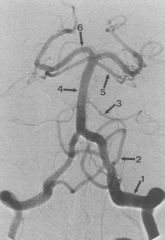
Who are we?
|
1. Vertebral Artery
4. Basilar Artery 6. Posterior Cerebral Artery |
|

What's the dx?
|
White phase of Raynaud's phenomenon
|
|

What's the dx?
|
Blue phase of Raynaud's phenomenon
|
|

What's the dx?
|
Red phase of Raynaud's phenomenon
|
|

What's the dx?
|
Digital ulceration and gangrene caused by Raynaud's phenomenon
|
|
What's the dx?
|
Livido Reticularis
|
|

What's the dx?
|
Livido Reticularis
|
|
|
What can other dz'es can livido reticularis be associated with on rare occasions?
|
Lupus and antiphospholipid syndrome
|
|
|
What is acrocyanosis?
|
A condition characterized by a persistent blue discoloration of the skin of the hands and sometimes feet.
|
|
|
What is acrocyanosis associated with?
|
Reduced skin temperature
|
|
|
What causes acrocyanosis?
|
Constriction of the precapillary arterioles leading to reduced skin temperature and dilation of the post-capillary venules leading to the blue color.
|
|

What's the dx?
|
Acrocyanosis
|
|
|
What symptoms do pts w/ acrocyanosis present with? what causes the symptoms to get worse?
|
Cyanosis of the distal limbs, cold skin and clammy palms. The blue color is intensified by exposure to cold.
|
|
|
What is thoracic outlet syndrome?
|
Syndromes of the upper extremity related to compression of the neural and vascular structures as they exit the thorax.
|
|
|
What symptoms do pts present with if they have thoracic outlet syndrome?
|
1. Pain in the shoulder/arm
2. Numbness and tingling in the arm, especially after activities that involve elevation of the arm above the head. (hair drying, hanging up clothes, sleep w/ arms overhead) 3. In the worst cases muscle atrophy of affected upper extremities. |
|
|
What causes thoracic outlet syndrome?
|
Compression of the subclavian artery and brachial plexus by any number of anatomical derangements.
|
|
|
What would hypertrophy or scarring of the anterior scalene cause? why?
|
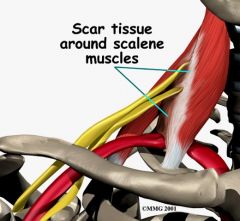
Thoracic outlet syndrome by compressing the subclavian artery and the brachial plexus as they exit b/e the anterior and middle scalenes
|
|
|
What is Adson's maneuver? how is it performed?
|
Tests for Anterior Scalene compression of the brachial plexus/subclavian artery by palpating the radial artery on the symptomatic side while having the pt. hold a deep inspiration after rotating the head (w/ chin raised) toward the involved side.
|
|
|
What is a positive Adson's maneuver?
|
Diminution or loss of the radial pulse.
|
|
|
What dz can the coracoid process of the scapula cause?
|
Thoracic outlet syndrome by compressing the subclavian artery.
|
|
|
How can you test to see if the coracoid process of the scapula is causing thoracic outlet syndrome?
|
By palpating the intensity of the radial pulse as the patients arm is elevated over their head.
|
|
|
What can the first rib and clavicle cause dz-wise?
|
The subclavian artery can be trapped b/e them and cause thoracic outlet syndrome.
|
|
|
How can you determine whether the first rib and clavicle are causing thoracic outlet syndrome?
|
By forcing the patient's shoulders back and downward, thereby decreasing the size of the thoracic outlet. Following this maneuver strength of the radial pulse is assessed w/ the patient's arm supported.
|
|
|
What does a cervical rib cause? What maneuver could help detect this?
|
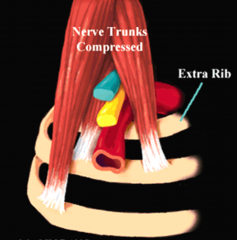
An extra rib that can impinge on the thoracic outlet by compressing the anterior scalene. Adson's test could help detect this.
|
|
What's the dx?
|
The coracoid process of the scapula compressing the subclavian artery.
|
|
|
What is subclavian steal syndrome?
|
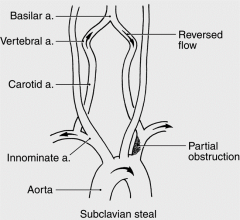
Narrowing of the subclavian artery proximal to the origin of the vertebral artery causes exercise in the upper limb to steal blood from the brain via the vertebral artery.
|
|
|
What symptoms do patients present with if they have subclavian steal syndrome?
|
Transient CNS ischemic symptoms result and resolve when the exercise is discontinued. ESPECIALLY signs of vertebral-basilar insufficiency.
|
|
|
A pt comes into your clinic and presents with the sudden onset of vertigo, ataxia, light-headedness, slurred speech, confusion and hemiparesis in response to heavy use of the extremity. What's the dx?
|
Subclavian-steal syndrome
|
|
|
What side of the body does subclavian-steal syndrome preferentially occur on?
|
The left side in > 85% of cases.
|
|
|
What physical exam findings point to subclavian steal syndrome?
|
BP and pulse are diminished in the affected arm and a systolic bruit is typically heard over the supraclavicular fossa.
|
|
|
What is the Allen test?
|
A test used to assess the patency of the radial artery, the ulnar artery and the palmar arch.
|
|
|
Why is the allen test important?
|
Important when using the radial artery for arterial puncture to obtain specimens of arterial blood. Unless the patient has an intact ulnar circulation and palmar arch, radial artery puncture may jeopardize blood supply to the patient's hand.
|
|
|
How is the allen test performed?
|

Both the radial and the ulnar arteries are compressed while the patient repeatedly clenches his fist until it blanches. Pressure is then released over the ulnar artery to see if the whole hand fills w/ blood.
|
|
|
What is a good outcome to the allen test? what is a bad outcome? what does a bad outcome mean?
|

A good outcome is when the whole hand fills with blood, this indicates an intact palmar arch and that the ulnar artery is present.
A bad outcome is when only the ulnar aspect of the hand fills w/ blood, this means the ulnar artery is present but the palmar arch is congenitally absent. Another bad outcome is the absence of either the ulnar artery or palmar arch. |
|
|
When is using the radial artery for arterial puncture contraindicated?
|
When either the palmar arch or ulnar artery is absent as proved w/ a positive allen test
|
|
|
What is the peripheral venous pressure in the supine position?
|
5-7mmHg higher than right atrial pressure
|
|
|
What is peripheral venous pressure in the standing position?
|
~90mmHg
|
|
|
What is peripheral venous pressure while walking?
|
Walking forces the veins of the lower extremity to empty as a result of muscular pumping so it reduces venous pressure to levels of ~25mmHg
|
|
|
What veins contain bicupsid valves?
|
Veins of the arms and legs
|
|
|
What do bicuspid valves do?
|
These valves direct the flow of blood to the heart and prevent reverse flow (venous insufficiency) that could raise venous pressure in the lower extremities to high levels.
|
|
|
What effect would any condition that affects the muscular pumping of venous blood or that damages venous valves have?
|
Will result in marked elevations of venous pressure.
|
|

What's the dx?
|
Absent palmar arch/ positive allen test.
|
|
|
What is the most common peripheral vascular dz affecting the lower extremity?
|
Varicose veins
|
|
|
What causes varicose veins?
|
hereditary weakness of the veins and their valves; occurs as a result of a deep venous thrombosis.
|
|
|
What is the distribution of varicose veins if they are hereditary?
|
Varicosities usually spread from the thigh to the lower leg.
|
|
|
What is the distribution of varicose veins if they are secondary to venous thrombosis?
|
Varicosities typically spread from the lower leg to the thigh.
|
|
|
What are the precipitating factors of varicose veins?
|
Obesity, pregnancy, cirrhosis of the liver w/ ascites and RV failure.
|
|
|
What do asymptomatic patients present with in varicose veins?
|
Concerns over the appearance of the dilated, tortuous superficial veins in the thighs and lower legs.
|
|
|
What do symptomatic pts present w/ in varicose veins?
|
1. Aching
2. A sensation of heaviness 3. Swelling in the lower extremity |
|
|
What causes the symptoms of varicose veins to be worse or better?
|
Worse: standing
Better: elevation of the legs |
|

What's the dx?
|
Varicose Veins
|
|

What's the dx?
|
Varicose Veins
|
|
|
What component of the venous system (superficial or deep) do venous thrombosis occur in?
|
Either component
|
|
|
What does venous thrombosis do?
|
Interferes w/ venous return by blocking the return of venous blood back to the heart. As a result, venous pressure in the peripheral venous system rises to extremely high levels.
|
|
|
When does thrombophlebitis occur?
|
When venous thrombosis is associated w/ inflammation of the adjacent vein wall.
|
|
|
What does Virchow's triad indicate?
|
Factors that contribute to the development of venous thrombosis
|
|
|
What are the members of Virchow's triad?
|
1. Venous stasis secondary to a sluggish venous circulation
2. Endothelial damage as a result of trauma 3. Hypercoagulability of blood |
|
|
What can cause venous stasis?
|
Sluggish venous circulation caused by:
1. RV failure 2. Cirrhosis w/ ascites 3. previous venous thrombosis 4. prolonged bed rest 5. pregnancy |
|
|
What can cause endothelial damage to the veins?
|
Trauma such as:
1. hip fracture 2. surgery |
|
|
What can cause hyper-coagulability of blood leading to venous thrombosis?
|
1. Malignancy
2. Surgery 3. Pregnancy |
|

What's the dx?
|
Unilateral Venous thrombosis
|
|
|
Where do the majority of deep venous thrombosis occur?
|
In the lower extremity
|
|
|
Where do most episodes of DVT begin? end?
|
Most episodes of DVT begin in the calf and propagate into the proximal venous system in the thigh.
|
|
|
What are the two major complications of deep venous thrombosis?
|
1. Pulmonary embolism
2. Chronic venous insufficiency |
|
|
When is the risk for pulmonary embolism highest? smaller?
|
In proximal vein thrombosis (popliteal or superficial femoral veins) and smaller for isolated calf vein thrombosis.
|
|
|
What is extremely common following an episode of DVT?
|
Postphlebotic syndrome or chronic venous insufficiency
|
|
|
What parts of the pt hx do drs spend extra time on when they suspect DVT?
|
Risk factors and Family Hx as well as timing of the symptoms
|
|
|
What do the risk factors for thrombosis relate to?
|
Virchow's triad (stasis, trauma, hypercoagulability)
|
|
|
What can indicate a hereditary abnormality in the clotting cascade?
|
A family hx of deep venous thrombosis
|
|
|
What are the common risk factors for DVT?
|
1. prolonged immobility
2. Recent trauma 3. known CA dx 4. dehydration 5. poor cardiac function. |
|
|
What should you do in a pt w/ DVT for whom no risk factors are identified?
|
These pts should undergo a thorough search for underlying malignancy.
|
|
|
What do asymptomatic pts w/ DVT present with?
|
complications from the thrombosis such as a pulmonary embolus.
|
|
|
Why should any pt w/ chest pain be questioned regarding risk factors for DVT?
|
B/c half of DVT pts are asymptomatic and only present w/ the complications of DVT such as a pulmonary embolus.
|
|
|
What do pts with symptomatic DVT present with?
|
Pain and/or swelling of the lower extremity (unilateral or bilateral)
|
|
|
Where is the swelling caused by DVT localized?
|
Localized to the calf or the entire leg.
|
|
|
What is the pain caused by DVT described as?
|
Aching, throbbing or pressure-like
|
|
|
What does the pt hx focus on for pts w/ DVT?
|
The timing of the symptoms, risk factors for thrombosis and alternative dx'es
|
|
|
What alternative dx'es should be considered in pts w/ DVT-like symptoms?
|
1. musculoskeletal injuries
2. Baker's (popliteal) cysts 3. cellulits 4. inguinal lymphadenopathy w/ impaired lymph drainage 5. poor cardiac or poor hepatic function 6. medication side effects |
|
|
Why can physical findings alone not be relied upon to dx DVT?
|
B/c of the range of presentations of pts w/ DVT. Some have no symptoms, some have all symptoms, some have all symptoms but when evaluated by venography do not have the dz.
|
|
|
How can you make the dx of DVT more reliable?
|
By combining specific findings from the hx and physical w/ the results of a noninvasive test (compression ultrasound).
|
|
|
What is a D-dimer test? what is it used for?
|
A test to stratify the pt w/ regards to DVT. D-dimer is a fibrin degeneration product which can be measured in the pts blood.
|
|
|
What is a positive D-dimer test?
|
Indicates recent or ongoing intravascular blood coagulation.
|
|
|
What can pts w/ a high/moderate pretest probability who also have a abnormal compression ultrasound study be reliably dx'ed with?
|
DVT (LR = 72)
|
|
|
What can pts w/ a low pretest probability and a normal compression ultrasound be dx'ed with?
|
They can be reliable excluded from DVT w/o need for a venography
|
|
|
What chance do pts w/ a high/moderate pretest probability and a normal compression ultrasound have of having DVT? What should you follow up the exam with?
|
~5%; they need a repeat compression ultrasound w/in one week or venography.
|
|
|
How can you avoid the compression ultrasound in the next visit in pts who had a high-moderate pretest probability of DVT but a normal compression ultrasound?
|
IF the d-dimer test is negative you can reliably avoid the compression ultrasound.
|
|
|
What vein typically causes superficial venous thrombosis?
|
Saphenous vein (or one of its tributaries)
|
|
|
What are the physical findings of superficial venous thrombosis?
|
The veins are superficial so physical exam findings are prominent including:
1. Erythema - redness of the skin 2. Warmth 3. Induration along the course of the vessel - hardness |
|
|
What other dz'es can be caused by superficial venous thrombosis?
|
Superifical venous thrombosis poses NO RISK for pulmonary embolism but it does contribute to varicose veins.
|
|

What's the dx?
|
Superficial venous thrombosis
|
|
|
What is chronic venous insufficiency?
|
refers to the reverse flow in veins due to incompetent valves.
|
|
|
What causes incompetent venous valves?
|
A result of involvement w/ venous thrombosis.
|
|
|
What do incompetent valves w/in the deep venous system cause?
|
Blood to flow back through the perforating veins into the superficial veins.
|
|
|
What effects on superficial veins do incompetent valves w/in the deep venous system have?
|
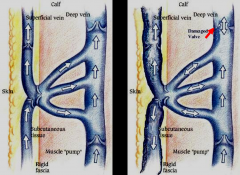
Venous HTN occurs w/in the superficial veins and varicosities result.
|
|
|
What can cause cutaneous edema and brawny induration?
|
They may occur as serum and blood extravasate into subcutaneous tissue.
|
|
What's the dx?
|
Chronic venous insufficiency
|
|
|
what causes the skin to have a brownish discoloration in venous insufficiency?
|
The breakdown of hemoglobin in the tissues leading to the formation and deposition of hemosiderin w/in the skin.
|
|
|
What are common side-effects of chronic venous insufficiency?
|
Pruritus (scratching/itching) and trauma from the scratching is a real problem.
|
|
|
What is stasis dermatitis?
|
The term given to ulceration, edema and brawny induration secondary to venous insufficiency.
|
|
|
What causes SVC obstruction?
|
Tumors w/in the mediastinum and lung cancer
|
|

What's the dx?
|
SVC obstruction
|
|
|
What are the physical findings of pts w/ SVC obstruction?
|
1. Cyanosis in the head, neck and arms;
2. Edema of the face, arms and upper third of the chest wall 3. elevation of the JVP 4. venous distention of the veins of the face, sublingual veins and conjunctiva (chemosis - swelling of the eyelids) |
|
|
What causes IVC obstruction?
|
Extrinsic compression from retroperitoneal lymphadenopathy, aortic aneurysm or massive hepatomegaly. ALSO intrinsic obstruction secondary to thrombosis.
|
|
|
What physical finding most likely points to IVC obstruction?
|
Dilated superficial veins w/ cephalad flow below the level of the umbilicus.
|
|
|
A pt has bilateral lower extremity edema w/ varicosities and brawny coloration. What's the dx?
|
IVC obstruction
|
|

What's the dx?
|
IVC obstruction
|
|

What's the dx?
|
SVC obstruction
|
|

What's the dx?
|
SVC obstruction
|

