![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
63 Cards in this Set
- Front
- Back
|
Name major pancreatic enzymes
|
Alpha-amylase—starch digestion, secreted in active form.
enzymes Lipase, phospholipase A, colipase—fat digestion. Proteases (trypsin, chymotrypsin, elastase, carboxypeptidases)—protein digestion, secreted as proenzymes also known as “zymogens.” Trypsinogen—converted to active enzyme trypsin by enterokinase/enteropeptidase, an enzyme secreted from duodenal mucosa. Trypsin activates other proenzymes and more trypsinogen (positive feedback loop). |
|
|
Achalasia
|
Failure of relaxation of lower esophageal sphincter (LES) due to loss of myenteric (Auerbach’s) plexus. High LES opening pressure and uncoordinated peristalsis lead to progressive dysphagia. Barium swallow shows dilated esophagus with an area of distal stenosis (bird's bick appearance)
|
|
|
What risk is achalasia associated with?
|
Increased risk of esophageal carcinoma
|
|
|
Name two otther conditions, outside of Aerbach's Plexus absence that will lead to achalasia
|
1. Chagas Disease - caused by Trypanosoma cruzi (Kissing bag)
2. Schleroderma (CREST Syndrome - five main features: Calcinosis, Raynaud's syndrome, Esophageal dysmotility, Sclerodactyly Telangiectasia) |
|

|
Cleft palate:Due to failure of fusion of the facial processes in the embryonic period. (Gi200)
|
|

|
Herpes simplex
Note the vesicular lesions above the vermilion border of the lip. The virus remains dormant in the cranial sensory ganglia. (Gi201) |
|

|
Reflux Esophagitis:
This is the most common type of esophagitis. There is acid chemical damage to the mucosa of the esophagus, owing to relaxation of the LES. Barrett's esophagus is a complication of GERD and predisposes to distal adenocarcinoma. (Gi017) |
|
|
Patient: executive under great stress, severe epigastric pain, shooting down the left shoulder: workup?
|
Flat Plate of the abdomen: an X-ray of the abdomen, without use of contrast media and obtained while the patient is recumbent.
The ulcer perforates, acid irritates diaphragm becomes irritated (phrenic nerve)--> referred pain to the shoulder because this is the same dermatome. |
|
|
Name the main causes of panctreatic insufficiency
|
Chronic pancreatitis: usually due to alcoholism in adults and cystic fibrosis in children. Leads to maldigestion of fats, fat-soluble minerals, carbs and proteins
|
|
|
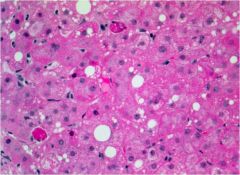
Councilman hyaline body is an eosinophilic globule often found in the liver in viral hepatitis, yellow fever, or other viral syndrome. It represents a hepatocyte that is undergoing apoptosis.
|
|

|
Duodenal Atresia: radiograph of the abdomen demonstrates the double bubble sign: an enlarged stomach (S) and proximal duodenum (D) in a neonate with duodenal atresia. Note the absence of distal gas.
Symptoms: obstruction - vomiting and abdominal distension, biliary vomit. |
|

3 week old male infant with recurrent projectile, nonbilious vomiting. No signs of illness (fever, diarrhea etc). Physical exam shows an olive shaped mass in the epigastric region
|
Pyloric sphincter stenosis
|
|
|
Name three main congenital mechanical disorders of the esophagus
|
1. Tracheoesophageal fistula
2. Esophageal webs 3. Achalasia |
|

Esophageal webs/rings
Associated sydromes |

Weblike protrusions of the esophageal mucosa into the lumen.
Presentation: dysphasia Epidemiology: women in 40s Risk factors: GERD Consequences: Fe deff anemia, increased risk of carcinoma Seen in Plummer-Vilson Syndrome Think of middle aged unmarried women purposely putting webs in their pipes esophagus) to lure in a cute plummer. Esophageal rings (Chatzki rings for Polish housewives) are very similar, but circumferential and thicker. They include mucosa, submucosa and muscularis propria |
|

Achalasia
|

Failure of the LES to relax with swallowing
Etiology: mostly unknown - loss of distal esophageal inhibitory neurons that release NO and VIP. In South America - Chagas disease that causes destruction of myenteric plexus. Presentation: progressive dysphagia Gross: esophageal dilation proximal to the LES Barium swallow: "Bird's Beak sign" Micro: loss of ganglion cells in myenteric plexus. Treatment: LES balloon dilation or myotomy. Increased |
|
|
Describe treatments for achalasia
|
- Laparascopic myotomy
- Balloon dilation - Botulinum toxin (botox) injection to inhibit LES cholinergic neurons |
|
|
What is achalasia putting one at an increased risk for?
|

Esophgeal carcinoma because food is roating in the dilated portion of the esophagus above strictured LES.
|
|
|
Mallory - Weiss Tears
|

- Longitudinal linear tears in the esophagus near gastroesophageal junction.
- Associated with severe retching or vomiting secondary to acute alcohol intoxication. Mechanism: relaxation of LES fails with prolonged vomiting - refluxing gastric contnents overwhelm and stretch and tear esophageal wall. 10% of upper esophageal bleeds are due to esophageal lacerations. Treatment: generally heal by themselves. |
|
Name the condition and its etiology
|
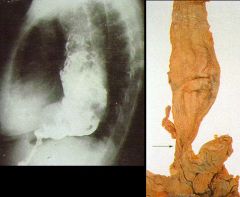
Esophageal achalasia - hypertonia of the lower esophageal sphincter produces the characteristic "birds beak" deformity.
Etiology: 1ry achalasia - caused by failure of distal esophageal inhibitory neurons. 2ry: Chagas disease, diabetic autonomic neuropathy |
|

Name the condition and describe its possible etiology
|
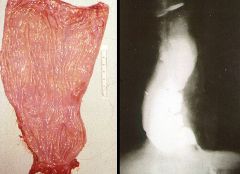
Esophageal stricture - concentric fibrosis of the submucosa produces
a long narrowed esophagus. This could be caused by chronic GERD, scarring or irradiation. The dysphagia associated with stenosis is usually progressive. |
|

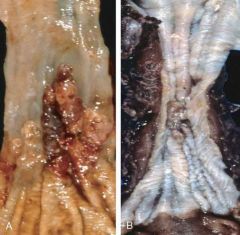
What pathology is seen on this gross image?
|
At the lower end of the esophagus (which has been turned inside out at autopsy) are linear dark blue submucosal dilated veins known as varices. In patients with portal hypertension (usually micronodular cirrhosis from chronic alcoholism), the submucosal esophageal veins become dilated (form varices). These varices are prone to bleed.
Esophageal varices DEVELOP IN 90% OF CIRRHOTIC PATIENTS, most commonly in association with alcoholic liver disease. Presentation: asymptomatic, with massive hematemesis when ruptured --> potentially fatal hemorrhage. TreatmentL surgical: band ligation |
|
|
Pathophysiology of GERD
|

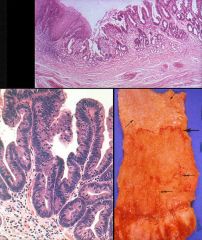
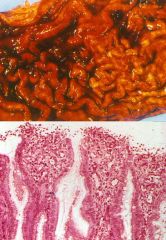
GERD is most common in adults over 40.<BR>Clinical symptoms: heartburn, dysphagia, sometimes regurgitation of sour-tasting gastric contents.<BR>Reflux of gastric juices leads to the development of mucosal injury in GERD.<BR>Barrett's Esophagus is a common complication of GERD characterized by intestinal metaplasia within the esophageal squamous mucosa. On the image we see patches of red, velvety columnar gastric mucosa rwith intestinal goblet cells eplacing pale, smooth esophageal squamous mucosa.<BR>Diagnosis requires histologic presence of gastric columnar mucosa with goblet cells above esophageal junction.<BR>Complications of GERD: bleeding, stricture formation, Barrett's esophagus
|
|
|
Describe two most common complications of Barretts esophagus
|
1. Ulceration with stricture formation (most common)
2. Glandular dysphasia with increased risk for distal adenocarcinoma (seen on image) |
|
|
Barrett's Esophagus
|
Metaplasia of the squamous esophageal mucosa to a more protective columnar type because of chronic exposure to gastric secretions.
Incidence is increasing. Gross: iregular GE junction with tongues of red granular mucosa extending up into the esophagus. Increased risk of dysphasia and esophageal carcinoma. |
|

Squamous Cell Carcinoma
("Second Class Citizen" carcinoma) |
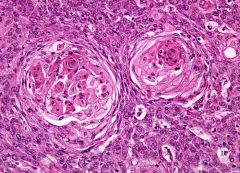
Squamous Cell Carcinoma
- arises most commonly in the upper and middle esophagus. Epidemiology: most common esophageal cancer in the world. Males>females, African Americans x 6>Caucasians. Risk factors: - Smoking - Alcohol - POVERTY - Plummer-Vinson syndrome - Achalasia Presentation: often asymptomatic until late in the course. Progressive dysphasia. Weight loss and anorexia. Bleeding. Histo: Squamous cell carcinoma is composed of nests of malignant cells that partially recapitulate the organization of squamous epithelium. Treatment: Surgery Prognosis: poor |
|
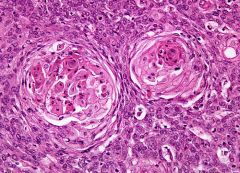
What type of esophgeal carcinoma this is more likely to be? Why? Describe pathophysiology
|
Squamous cell carcinoma is composed of nests of malignant cells that partially recapitulate the organization of squamous epithelium.
|
|

Adenocarcinoma of the esophagus
|
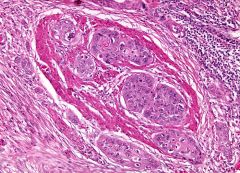
Adenocarcinoma arising in Barrett's Metaplasia -
the presence of a nodular mass in a field of Barrett's metaplasia is highly suspicious for adenocarcinoma. Adenocarcinoma of esophagus is the most common in Western countries and US. Caucasians>Africans Arises in DISTAL esophagus. Associated with Barrett's esophagus and dysphasia - presumably due to accumulationof mutations during progression to dysphasia and ivasive carcinoma. Histo: esophageal adenocarcinoma is organized into back-to-back glands. |
|
Esophageal cancer: how to distinguish between adenocarcinoma and squamous cell carcinoma?
|
- Adenocarcinoma usually occurs distally and often involves gastric cardia. Initially appears as flat or raised pathes in otherwise intact mucosa. Adenocarcinomas frequently produce musin and form glands.
Squamous cell carcinoma - are most frequently found in mid esophagus, where it is commonly causes strictures. |
|
|
Pyloric stenosis
|
Congential form is due to hyperthrophy of pyloric sphincter resulting in gastric outlet obstruction.
Males>females Associated with Turner and Edwards syndrome. Presentation: onset of regurgitation and vomiting in the second week of life. Waves of peristalsis are visible in the abdomen plus a firm, ovoid abdominal mass. Acquired pyloric stenosis: in adults as a result of antral gastritis or peptic ulcers close to pylorus. |
|
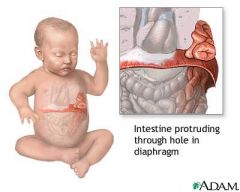
Diaphragmatic hernia
|
Congenital defect in the diaphragm resulting in hurniation of the abdominal organs into the thoracic cavity.
The stomach is the most common hurniated organ. Often associated with intestinal malrotation Complications: respiratory compromise - underdeveloped lungs |
|
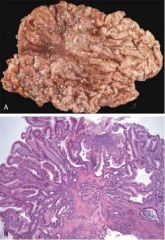
What is the pathology?
|
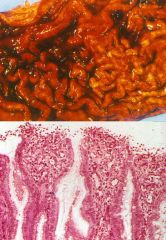
Menetrier disease Think of a Man becoming Tree-Like.
Menetrier disease is a disorder characterized by increased secretion of Transforming Growth Factor (TGF-alpha). As a result: diffuse hyperplasia of the foveolar mucous-secreting epithelium of the body and fundus and hypoprotenemia. Replacement of parietal and chief cells-> decreases HCl production Increased risk of gastric adenocarcinoma. Treatment: supportive Histo: can see elongated cork-screw like foveolar glands. |
|
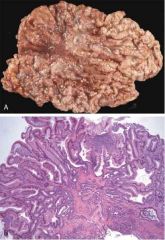
What is the pathology?
|
Menetrier disease Think of a Man becoming Tree-Like.
Menetrier disease is a disorder characterized by increased secretion of Transforming Growth Factor (TGF-alpha). As a result: diffuse hyperplasia of the foveolar mucous-secreting epithelium of the body and fundus and hypoptotenemia. Replacement of parietal and chief cells-> decreases HCl production Increased risk of gastric adenocarcinoma. Treatment: supportive Histo: can see elongated cork-screw like foveolar glands. |
|
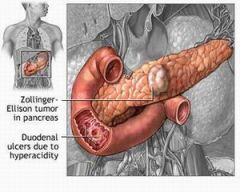
Describe the pathophysiology of Zollinger-Ellison Syndrome
|
Caused by gastrin secreting tumors, gastrinomas, usually found in the pancreas or small intestine.
Gross: enlarged rugal folds because Gastrin induces hyperplasia of parietal cells (5X increase) and mucous producing cells-> Increased acid secretion. Presentation: multiple intractable peptic ulcers. Treatment: goal 1: blockage of acid hypersecretion by PPI or high dose H2 histamine receptor agonists. goal 2: identification and resection of gastrinomas. Most are solitary tumors and are easily resected. 25% have multiple neoplasia type I. |
|
36 yo male patient presents with burning epigastric pain accompanied by nausea and vomiting. Melena is present in his stool. Patient is a chronic NSAIDs user and smoker of 15 years. The physical examination findings are often normal with occasional mild epigastric tenderness. What is the most likely diagnosis?
|
Acute Hemorrhagic Gastritis
Definition: acute inflammation, erosion, hemorrhage of gastric mucosa due to a breakdown of mucosal barrier and acid-induced injury. Etiology: - Chronic aspirin/NSAID use - Alcohol use - Smoking - Postsurgery - Burns - Ischemia - Stress Presentation: epigatstric abdominal pain. Gastric hemorrhage, hematomesis, melena. |
|
36 yo male patient presents with burning epigastric pain accompanied by nausea and vomiting. Melena is present in his stool. Patient is a chronic NSAIDs user and smoker of 15 years. The physical examination findings are often normal with occasional mild epigastric tenderness. What is the most likely diagnosis?
|
Acute Hemorrhagic Gastritis
Definition: acute inflammation, erosion, hemorrhage of gastric mucosa due to a breakdown of mucosal barrier and acid-induced injury. Etiology: - Chronic aspirin/NSAID use - Alcohol use - Smoking - Postsurgery - Burns - Ischemia - Stress Presentation: epigatstric abdominal pain. Gastric hemorrhage, hematomesis, melena. |
|

Describe the pathophysiology of gastric stress ulcers
|
Gross: multiple, small, round, superficial ulcers of the stomach and duodenum.
Etiology: NSAIDs use, severe stress, sepsis, shock, severe burns or trauma (Curling ulcers), elevated intracranial pressure (Cushing ulcers) HIGH INCIDENCE AMONG ICU PATIENTS Complication: bleeding. |
|

Describe the pathophysiology of chronic gastritis
|
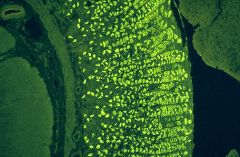
Chronic inflammation of the gastric mucosa eventually leading to athrophy.
Two main types: - Fundic/Body type - Autoimmune gastritis (Abs are produced to parietal cells and intrinsic factor) - Antral type - medicated by Helicobactor Pylori. Most common in the US. Associated with duodenal and gastric ulcers. Foci of acute inflammation. chronic inflammation with lymphoid follicles. |
|
Describe the pathophysiology of autoimmune gastritis
|
- Fundic/Body type of gastritis
- Abs are produced to parietal cells and intrinsic factor - Loss of patietal cells - Decreased acid secretion - Increased serum gastrin (G cell hyperplasia) - Pernicious anemia Gross: loss of rugal folds Histo: mucosal athrophy with loss of glands and patietal cells Increased risk of gastric carcinoma |
|
|
In a newborn, projectile vomiting after feeding and an olive-shaped mass palpable within the andomen is indicative of what congenital abnormality of the GI tract?
|
Pyloric stenosis - when the muscle of the pyloric sphincter is too hyperthropied to allow adequate passage of chyme from the stomach into duadenum.
|
|
|
Describe pathogenesis of Hepatic adenoma
|
See slides
|
|
|
What are the main risk factors for the development of malignancy from hepatic adenoma?
|
Beta – Catenin mutation
Glycogen storage disease |
|
|
Describe the pathogenesis of Focal Nodular Hyperplasia
|
Regenerative nodule formation due to abnormal vascular supply
|
|
|
Name four main types of primary hepatic tumors
|
Hepatocellular carcinoma
Angiosarcoma Hepatoblastoma Cholangiocarcinoma |
|
|
Name four major etiologic factors associated with hepatocellular carcinoma
|
- Chronic viral infections (HBV, HCV)
- chronic alcoholism - non-alcoholic steatohepatitis (NASH) - food contominanst (mainly afilatoxin - binds to DNA and messes with p53) Plus some others (glycogen storage disease, hereditary hemochromatosis, alpha-1 antitrypsin deficiency) |
|
|
Is there a difference in etiologic factors between Asia and Western countries?
|
Asia: mainly due to HBV, aflatoxin, in young patients, cirrhosis uncommon
In Western countries: HCV, alcohol, NASH are main factors Causes cirrhosis |
|
|
Describe the pathogenesis of Hepatocellular Carcinoma
|
Repeated cycles of cell death and regeneration --> accumulation of mutations --> hepatocellular transformation plus chronic inflammation
In western world: often due to random mutations in Wnt or AKT pathways, KRAS, p53, c-MYC etc In Asia: due to HBV integration plus aflatoxin's effects |
|
|
Describe clinical presentations of HCC
|
Ill-defined upper abdominal pain
Malaise Fatigue weight loss Sometimes can palpate irregular nodular liver shape |
|
|
Describe the course of clinical progression of HCC
|
Progressive enlargement of the tumor till it seriously disturbs hepatic function or metastasizes, generally to the lungs and then to other sites. Death occurs from either:
a. calcexia b. GI or esophageal bleeding c. liver failure with hepatic coma d. rapture of the tumor with hepatic hemorrhage |
|
|
Is HCC see mainly in males/females or equal in both sexes?
|
3rd most common cause of cancer deaths
Clear predominance of men: 2.4:1 |
|
|
Describe the pathogenesis of fibrolamellar carcinoma
|
The etiology unknown. Typically occurs in the absence of underlying liver inflammation or fibrosis. Presents with single large, hard scirrhous tumor with fibrous bands coursing through it.
5% of HCCs, equal in males and females. |
|
|
Comment of Angiosarcoma
|
Rare, aggressive (survival less than 5 months). Uncommon malignant neoplasms characterized by rapidly proliferating, extensively infiltrating anaplastic cells derived from blood vessels and lining irregular blood-filled spaces.
Risk factors: - vinyl chloride - arsenic - thorotrast |
|
|
Comment on main features of Hepatoblastoma
|
The most common liver tumor of young childhood (neonates and infants)
Agrressive Hepatomegaly, failure to thrive, vomiting Elevated apha-fetoprotein |
|
|
What is the most common malignant liver tumor?
|
METASTASIS
|
|
|
What are the main origination sites of liver metastases?
|
Breast, lung, colon, upper GI, Pancreas, melanoma
|
|
|
How do metastatic liver cancers present?
|
Can be asymptomatic despite massive liver involvement.
Liver failure, jaundice, hepatomegaly |
|
|
Define acute cholecystitis
|
Acute inflammation of the gallbladder, precipitated 90% of the time by obstruction of the neck or cystic duct
|
|
|
Describe pathogenesis of acute cholecystitis
|
Results from chemical irritation and inflammation of the obstructed gallbladder (mucosal epithelium becomes disrupted by the action of bile salts). Bacterial contamination may also develop.
Acute acalculous cholecystitis is thought to develop from ischemia. |
|
|
Define empyema of the gallbladder
|
Condition where the contents of the gallbladder are almots entirely puss
|
|
|
Describe clinical features of acute cholecystitis
|
Progressive RUQ or epigastric pain, frequently associated with mild fever, anorexia, sweating, nausea and vomiting
|
|
|
Describe pathogenesis of chronic cholecystitis
|
Typically develop following long-term co-existance of gallstones and low grade inflammation.
|
|
|
What are Rokitansky-Aschoff sinuses and in what disease do we see them?
|
In chronic cholecystitis we often see reactive proliferation of mucosa and fusion of the mucosal folds that gives rise to buried crypts of epithelium within the gallbladder wall. These outpouchings are called Rokitansky-Aschoff sinuses (Robbins p.886)
|
|
|
What is porcelain gallbladder?
|
Extensive dystrophic calcifications within gallbladder
|
|
|
After an extraction of an absessed tooth - sulfur granules in pus, contain gram+ brabching filamentsm anaerone
|
actomyces israeli
|

