![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
116 Cards in this Set
- Front
- Back
|
what are the indications for imaging in a trauma when there is concern for renal injury?
|
Absolute indications -
*Penetrating abdominal injury *Blunt injury with gross hematuria, most patients with upper tract injury present with gross hematuria (95%), *Microscopic hematuria with a period of hypotension or SBP <90mm Hg. *Also you have to be a doctor so think about the mechansim of injury like rib fractures, fall from height, flank injury, etc. as well as microscopic hematuria in the absence of hypotension. |
|
|
Could a patient have significant renal injury without hematuria?
|
Yes, you could have complete ureteral transection, avulsion of the vascular pedicle, renal artery thrombus.
|
|
|
How is this different in penetrating trauma?
|
In penetrating trauma if the patient is stable and can get imaged and there is any concern for upper tract injury there should be imaging studies done.
|
|
|
So let's say there is penetrating trauma and there is concern for a renal injury but no time for pre-op imaging studies, you are called into the OR because there is concern for renal injury, what should you do?
|
The reasons that you might get called in would include a retroperitoneal hematoma, but if it is non-expanding nor pulsatile then you don't have to explore it. But you can do a one-shot IVP on the OR table.
*These are the textbook stated indications for exploration but Carson was making fun of this at a tuesday case conference saying that in all of his years of practice he has never seen a pulsatile or expanding hematoma in the retroperitoneum. |
|
|
What is the goal of the one shot IVP at the time of operative exploration?
|
Really more than anything you are looking for contrast excretion in the contralateral kidney just in case you are considering doing a trauma nephrectomy.
|
|
|
How do you perform an intra-operative one shot IVP?
|
You give the patient iv contrast, you have to make sure that you know what kind that is, at 2cc/kg and then you wait 10 minutes after you have given it and you take a KUB.
|
|
|
Does the degree of hematuria correlate with degree of injury with penetrating injuries to the upper tract?
|
No, so you need to image and be concerned about even microscopic hematuria in a penetrating trauma patient.
|
|
|
Who are more likely to sustain injury from blunt trauma to the kidneys kids or adults?
|
Kids. The reason for that is relatively larger kidney size for patient size, less perirenal fat (think about doing an adult neprhectomy and a pediatric pyeloplasty), greater flexibility of the ribcage and spine.
|
|
|
So if a pediatric patient has a blunt trauma and there are no associated injuries and there is microscopic hematuria do you have to image that patient?
|
The answer is probably no, there was several studies looking at this and if a child has no other injuries with a relatively low degree of blunt impact and only microscopic hematuria then the likelihood of renal injury is very low. But there are other studies showing that these children may have injuries and we know that children don't get hypotensive until it is almost too late to save them, so the consensus by the WHO is that every child with gross hematuria and if a child has <50RBC/HPF with blunt trauma then they get imaged.
|
|
|
The AUA update on Trauma from 2006 talks about when they do and when they don't do delayed films for renal and ureteral injury, what is it?
|
Basically they state that if there is blunt trauma and the film is officially reviewed at the time of scan and the kidneys appear normal, there is no perinephric fluid, and there is no perivesical or retropreitoneal fluid.
However that being said I don't think anyone will ever fault you for getting delayed films and you may miss a small injury |
|
|
What is the role of angiography in trauma?
|
The role of angiography in the trauma setting these days is mostly therapeutic for patients that need embolization of acute or delayed hemorrhage.
|
|
|
When should the patient with blunt renal injury be re-imaged?
|
*Kind of controversial
*One Study - Patients with grade III-V blunt renal injury should be re-imaged in 2-4 days after initial injury. Hunter Wessells group questioned this because of the cost and contrast exposure and radiation exposure this would cause. *Hunter Wessells - author of the AUA update on imaging for GU trauma '06 - states that in their series that they only f/u image grade 4 & 5 blunt injuries with ultrasound as the only major complication that required intervention in their series of patients was urinoma, which would be seen. They don't image grade III. If CT scan is used they don't perform multiple phases and only use a late cortical phase where cortical abnormalities will still be evident and collection system issues will be seen. *They don't image any of the lesser injuries with the exception of those patients with persistant gross hematuria, patients with extensive extravasation of urine at the time of original injury, or drop in HCT, or patients with symptoms of possible AV fistula or pseudoaneurysm. *The other point is that for patients with grade IV and V injuries nuclear function studies are performed at 3 months after injury regardless of other management. |
|
|
What findings on CT scan might make you concerned for ureteral injury?
|
low density Fluid medial to the UPJ or adjacent to the ureter or concerning for ureteral injury.
|
|
|
What should you do if you suspect ureteral injury?
|
According to this AUA update you should directly inspect the ureter, but we don't really do that. The 2006 AUA update also states that instead you can do a RPG to help you diagnose and at that time can do a stent to bypass the leak and try ot heal it, this seems like a good option to me, can also do this in the delayed setting.
|
|
|
What kind of imaging should you do if you are worried about a bladder injury? How is it performed?
|
Either a CT cystogram or a cystogram. You should perform with contrast instilled under gravity and not by pressure. The AUA update says that you should have 300 to 400cc in the bladder as well as post-drainage films for conventional cystogram.
For a CT cystogram you have to retrograde instillation of contrast 300-400mls at 40mm Hg and you don't have to do delayed films or early filling flims. |
|
|
What percentage of pelvic fractures is actually associated with bladder injury?
|
about 10%
|
|
|
What associated injuries make you think of a urethral injury in a female?
|
Associated bladder injury or vaginal injury, especially anterior vaginal wall injuries.
|
|
|
What is the classic physical exam finding for urethral injury in a male?
|
Blood at the meatus.
|
|
|
What type of imaging should you consider doing in a urethral injury case? Should you knee jerk think of other imaging studies because of other injuries that are associated?
|
Well there is obviously a retrograde urethrogram or pericatheter urethrogram, you also have to consider CT cystogram because most of these injuries are associated with pelvic fractures and bladder injuries.
|
|
|
What if you are worried about a penile fracture or a tear in the tunica?
|
Then you do a circumcisiing incision and repair the injury primarily. If there is concern for an associated urethral injury then you do a RUG.
|
|
|
How should blunt scrotal trauma be evaluated?
|
Ultrasound.
|
|
|
In a patient with a renal injury in which on the delayed phase there is evidence of extravasation at the UPJ and you don't see any contrast distal in the ureter what should you do?
|
In that case you have to do something urgently to get something across that defect in the ureter. This may be a stent in a retrograde fashion or open operative intervention. This should probably be done within the first 72 hours.
Source - Dan & Adam |
|
|
Is hematuria a reliable marker of GU trauma in children?
|
No, some studies have found that up to 70% of children with grade 2 or higher renal injuries have no gross on microscopic hematuria on initial evaluation
|
|
|
What percentage of patients with grade 3 or 4 renal trauma managed in a nonoperative fashion will develop persistent or secondary (delayed) hemorrhage? When does delayed hemorrhage usually present? How can this typically be managed?
|
- 25%
-10-14 days, but usually within 1 month - selective angiographic embolization |
|
|
What is postembolization syndrome?
|
- a self-limiting condition manifested by pyrexia, flank pain, and adynamic ileus due to release of
pyogens from the necrosing kidney parenchyma. Usually resolves in 96 hours. -get blood and urine cultures to rule out bacterial seeding of necrotic tissue. |
|
|
When is follow-up renal imaging indicated after a renal injury?
|
*Again controversial
* Campbell's probably says Grade 3 injuries with devitalized fragments as well as grades 4 and 5 injuries should be reimaged 2 to 3 days after the injury. This serves to assess the extent of the hematoma/ urinoma and will serve as a baseline evaluation in case of secondary hemorrhage. *Again AUA Update '06 by Hunter Wessells group rarely images grade III and grade IV and V only with ultrasound usually. * Both sources agree that these patients should also receive a repeat scan at 3 months to verify resolution of any perinephric urinoma and to define the anatomic configuration of the residual functioning renal parenchyma |
|
|
How long after a renal injury should pass before a DMSA scan is performed? Who should get a DMSA scan?
|
*1 week: degree of renal recovery known by one week post-trauma, I guess this is from Campbell's
*patients with grade 3 injuries, all grades 4 and 5 injuries , and any patient with persistent hypertension following renal injury, those patients with renal hypertension that is persistant are usually patients with a poorly functioning kidney. *Again the above is from Campbell's the AUA update says 3 months from Hunter Wessell's group. |
|
|
If an injury to the main renal artery is identified, when should surgical repair be attempted?
|
- main renal artery reconstruction rarely successful
- it is only ever worth attempting in situations in which the patient is otherwise hemodynamically stable and the injury involves a solitary renal unit or is a bilateral renal artery injury -repair is seldom indicated with a normal contralateral kidney is identified |
|
|
What is the incidence of traumatically induced renovascular hypertension following grade 3 or greater renal injury? When does it typically occur?
|
- 5%
- it usually occurs within 36 months after the injury |
|
|
What studies are indicated in working up post-traumatic renovascular hypertension?
|
- DMSA to establish split renal function
- MRI or CT angiography to rule out an AV fistula |
|
|
What are the management options of trauma-induced renovascular hypertension?
|
- if an AV fistula is the cause, embolization may be effective
- if due to segmental renal ischemia, partial nephrectomy may be attempted - in most cases, the hypertension is due to a small, poorly function kidney (<20% function) associated with pan-nephric scarring---->Nephrectomy |
|
|
What are the classic CT findings associated with disruption of the UPJ?
|
-1. good renal contrast agent excretion with medial extravasation of contrast agent in the perirenal and upper ureteral area;
-2. absence of parenchymal lacerations -3. lack of visualization of the ipsilateral distal ureter |
|
|
In patients with pre-existing hydronephrosis or congenital UPJ obstruction, is there a higher likelihood of UPJ disruption?
|
-controversial, but authors say no. The vast majority with these conditions sustain renal contusions or Grade I injuries at best.
|
|
|
What complication rate do the authors site for management of ureteral injuries endoscopically with stenting versus with open surgical repair?
|
- 40% for endoscopic management (primarily strctures and fistulas) vs. 10% for open surgical repair
|
|
|
What time cut-off after ureteral trauma do the authors use to determine primary repair vs. drainage with delayed repair?
|
- if the injury is discovered within 5 days of its occurrence, the authors suggest primary surgical repair
- if later than 5 days, the authors opt for drainage with delayed repair |
|
|
What are the ABSOLUTE indications for bladder imaging after blunt abdominal trauma?
|
- 1. the presence of gross hematuria coexisting with a pelvic fracture and
-2. inability to void. Note: Neither gross hematuria alone nor pelvic fracture alone is an absolute indication for screening. |
|
|
What is one important difference to consider between bladder injuries in kids compared to adults?
|
- Traumatic bladder lacerations are approximately 2 times more likely to extend through the bladder neck in kids compared to adults.
-should be suspected any time extravasation of contrast agent is noted, and a competent bladder neck cannot be documented via radiographic studies. -if suspected, --->surgical exploration and intravesical repair |
|
|
Is management of a bladder neck laceration with an SPT and/or foley catheter adequate for full recovery? Why or why not?
|
-No.
-management of a BN laceration with a suprapubic tube alone or with foley drainage may result in the persistent extravasation of urine, the possible development of a pelvic urinoma/abscess or pelvic osteomyelitis, and urinary incontinence |
|
|
How much contrast should be instilled in into a child’s bladder for adequate imaging of an injury?
|
- one half of the estimated bladder capacity based on age (2 + age in years = ounces of bladder capacity).
or you could mutliply times 30 to eaqual mls. |
|
|
What are four differences between posterior urethral injuries in children compared to adults?
|
- a pelvic fracture is more likely to be unstable and associated with a severely and
permanently displaced prostatic urethra. - the severe displacement of the prostate off the pelvic floor makes a complete posterior urethral disruption more common in boys than men. - in children, concurrent bladder and urethral injuries may occur in up to 20% of the patients, with coexisting anterior longitudinal tears though the bladder neck and sphincteric complex being twofold more common in children compared with adults - in prepubertal girls, pelvic fractures are four times more likely to be associated with a urethral injury than in adult women |
|
|
What circumstances mandate radiographic or cystoscopic evaluation to rule out urethral injury in children?
|
- (1) when the patient presents with the classic triad of findings of a perineal/penile hematoma, blood at the meatus/vaginal introitus, and inability to void; 2) when one or more pubic rami are fractured or symphyseal diastases are present; and (3) when radiographic findings suggest a bladder neck injury
|
|
|
What should you do if a pediatric patient presents with evidence of urethral injury and a pelvic fracture?
|
-DRE: blood in the stool may signify occult rectal injury, which must be promptly treated with diverting colostomy to prevent the development of a pelvic abscess, pelvic osteomyelitis, and necrotizing fasciitis
|
|
|
What defines a penile fracture?
|
- disruption of the tunica albuginea with rupture of the corpus cavernosum
|
|
|
What are the most common mechanisms of penile fracture?
|
- traumatic sexual intercourse: rigid penis slips out of vagina and strikes the perineum or pubic bone- "faux pas du coit"
|
|
|
How are penile fractures usually diagnosed?
|
- HISTORY:
-patients will complain of a blow to the erect penis accompanied by a "cracking" or "popping"sound, pain, immediate detumescence and swelling. -PHYSICAL: -A corporal defect fracture line may be palpable. Extruded blood combined with swollen tissue creates a hugely deformed ecchymotic penis (“eggplant deformity”), a sign that is highly diagnostic. -If Buck’s fascia is ruptured, blood and urine extravasate around Colles’ fascia, giving a characteristic “butterfly sign” in the perineum. -the swollen,ecchymotic phallus will tend to deviate to side contralateral to site of injury (due to mass effect,hematoma) |
|
|
Where do most penile fractures occur?
|
-distal to the suspensory ligament
|
|
|
How are penile fractures managed?
|
- prompt surgical exploration and repair using a distal circumcising incision or some would advocate for a penoscrotal incision as most of these injuries are more proximal on the shaft and closure of the tunical defect with interrupted 2-0, 3-0, or 4-0 absorbable suture;
-debridement of the delicate underlying erectile tissue must be avoided |
|
|
What imaging study could be considered in cases where penile fracture is suspected but not obvious by history of physical exam?
|
- MRI
|
|
|
. How often is a urethral injury associated with penile fracture? What test should be performed when this is suspected?
|
- 38% of the time
- RUG |
|
|
How should gunshots to the penis be managed?
|
Immediate exploration, copious irrigation, excision of foreign matter, antibiotic prophylaxis, surgical closure
- Urethral injuries are common (15%-50%) in the setting of GSWs to the penis -RUG should be routinely performed especially with blood at the meatus, difficulty voiding, or close proximity of bullet's trajectory to the urethra |
|
|
How is penile amputation managed?
|
- if the amputated segment is available, transfer to a facility with microsurgical capabilities.
Then reconstruction of the urethra and reanastomosis of the corpora cavernosa with microsurgical repair of the penile vessels and nerves - if microsurgical capabilities are not available, macroscopic anastomosis of the urethra and corporal bodies can be performed with good erectile results albeit with less sensation - if the amputated segment is not available, the penile stump should be formalized by closing the corporal bodies and spatulating the urethral neomeatus similar to a partial penectomy. |
|
|
10. What is the most common etiology of testicular rupture?
|
- blunt scrotal trauma accounts for 75% (assault, sports injuries, and MVAs)
- penetrating scrotal injuries account for the rest of testicular injuries |
|
|
What is the typical presentation of testicular rupture?
Does the absence of a scrotal hematoma rule out injury? |
- Exquisite scrotal pain and nausea; swelling and ecchymosis are variable, and the degree of
hematoma does not correlate with the severity of testis injury. Absence of hematoma does not rule out fracture |
|
|
What imaging study may be useful in evaluating suspected testicular fracture? What findings on scrotal ultrasound indicate likely testicular injury?
|
-Ultrasound
-inhomogeneity of testicular parenchymal texture, disruption of the tunica albuginea |
|
|
T/F: In the presence of a normal ultrasound, it is not necessary to surgically explore the site of injury?
|
-False: ultrasound is highly operator-dependent, resulting in high percentage of false-negative rates.
|
|
|
How should testicular rupture be managed? What is the benefit of doing it the right way?
|
- Early exploration and repair as this is associated with increased testis salvage, reduced convalescence and disability, faster return to normal activities, and preservation of fertility and hormonal function.
|
|
|
How do you repair testicular rupture?
|
-After removal of the scrotal hematoma, complete exposure of the testicle, epididymis, and
spermatic cord provides the opportunity to detect all injuries. The testicular parenchyma is typically seen extruding through a transverse laceration in the tunica. This portion of the parenchyma is often devitalized and should be completely excised. No attempt should be made to force the extruded parenchyma back into the tunica albuginea because high-pressure parenchymal necrosis might ensue after closure. The fracture margins of the tunica should be approximated with fine absorbable suture, usually placed in a continuous locking method. The area is liberally drained with a Penrose or closed-suction technique. |
|
|
Are bladder injuries common in external trauma? Why or why not?
|
-No; the bladder is relatively protected from injury by the boney pelvis
|
|
|
What are bladder injuries commonly associated with? What percentage of pelvic fractures are associated with a bladder injury?
|
- pelvic fracture; 6-10% of pelvic fractures will have an associated bladder rupture; conversely
80-100% of bladder ruptures have a concomitant pelvis fracture |
|
|
What are some signs/symptoms associated with bladder injury?
|
- gross hematuria: present in 95-100% of bladder injury patients and associated with more significant injuries (bladder rupture), whereas microhematuria has been more commonly seen in patients with bladder contusion.
-abdominal tenderness/distension, inability to void, bruising over suprapubic region, perineal/scrotal swelling,clots in urine, preexisting bladder disease/surgery |
|
|
What imaging modalities can be used to dx bladder rupture? What are the sensitivites and specifities of the different studies?
|
- retrograde cystography with post-drainage films (13% of ruptures will only be dx by the post drainage film: lesser used modality
- CT cystography: most often used since most of these patients already require CT evaluation. Modality has sensitivity/specificity of 100%/99% for EPR and 92%/100% for IPR |
|
|
What is the technique used for CT cystography
|
- retrograde placement of 350 mL of 30% contrast material diluted 6:1 with saline prior to CT
|
|
|
Is clamping of the urethral catheter during a contrasted CT abdomen/pelvis to allow antegrade filling of the bladder adequate to rule out bladder injuries?
|
- NO!
|
|
|
What is the most common class of bladder rupture and what is the likely causative factor?
|
- Extraperitoneal rupture-found alone in 62% and in combination with intraperitoneal ruptures
in another 12%. -result from direct laceration, usually by boney spicules from the fractured pelvis. |
|
|
How should extraperitoneal ruptures be managed? When is surgical correction indicated?
|
-usually managed conservatively with foley catheter (authors recommend 22 French) drainage, followed by cystogram in 10-14 days
-Prophylactic abx are given from the time of injury until three days after the catheter comes out. - Relative indications for surgical correction are bone fragment projecting into the bladder (which is unlikely to heal), open pelvic fracture, and rectal perforation (high risk of infection). -Another relative indication for repair of extraperitoneal rupture is found in patients undergoing laparotomy for other reasons (such as open exploration by the general surgery team for intra-abdominal injuries). There is evidence that operatively managed patients with extraperitoneal ruptures do better long-term. -Patients should also undergo repair any time Ortho is taking them to OR for reduction of pelvic fracture (some say decreases infection risk of their hardware). -Also if the injury is at the urinary trigone or bladder neck as this will not heal and the patient is likely to end up with a large urinoma and abscess, if you can't see a competent bladder neck on imaging then should consider this option. |
|
|
What percentage of bladder ruptures do intraperitoneal ruptures constitute? What is the mechanism of injury? Where do intraperitoneal ruptures typically occur, i.e. what part of the bladder?
|
- they constitute 25% of all bladder ruptures by themselves and another 12% in combination with extraperitoneal ruptures
- Intraperitoneal ruptures occur after blunt trauma in which rapidly rising intraperitoneal pressure causes the bladder to burst , usually at its weakest spot (dome) Dr. Teigland gave the historical anecdote of new soldiers versus vetaran soldiers and the modern day example of a drunk and how the full bladder and once they get a rupture they get a burst of urine into the intraperitoneal cavity. |
|
|
What findings on CT cystography indicate IPR?
|
-extravasation of urine around bowel loops, between mesenteric folds, or in paracolic gutters
|
|
|
How should intraperitoneal ruptures be managed?
|
- open operative repair with two-layer closure using absorbable suture and perivesical drain placement;
- SP tube in conjunction with urethral catheterization is traditional but may not be necessary -abx until three days after catheter is removed. - cystogram on POD 7-10 |
|
|
What are urethral distraction injuries associated with?
|
-Urethral distraction injuries are a common sequela of pelvic fracture, occurring in 10% of males and 6% of females sustaining pelvic fractures.
-associated with bilateral pubic rami fractures (so-called straddle fractures), especially when this pattern is seen with diastasis of the sacroiliac joint. Much more common in males, but girls younger than 17 years have a significantly increased risk of urethral injury compared with women, perhaps owing to greater compressibility of the pelvic bones |
|
|
What is the clinical triad associated with urethral injury?
|
-blood at the urethral meatus, inability to urinate, and palpably full bladder.
-High riding prostate is a very unreliable marker (only found in 30%) |
|
|
How is the diagnosis of urethral disruption confirmed? How is it initially managed?
|
- In males, RUG. Females get cystourethroscopy in lieu of RUG.
-if a urethral injury is demonstrated, one attempt at placement of a 16-Fr silicone urethral Catheter may be attempted by a urologist - if this fails, the patient is brought to the operating room for placement of a formal suprapubic urinary catheter, bladder exploration, and repair of bladder injuries if present. |
|
|
Today, what is meant by “primary realignment” and when should it be done for urethral disruption?
|
- endoscopically assisted stenting of the distraction with a urethral catheter, without any pelvic dissection or sutures.
-When indicated, authors favor realignment as soon as practical (usually within 72 hours); -The polytrauma patient with life-threatening associated injuries and severe pelvic fracture should not undergo an attempt at primary realignment. |
|
|
If indirect primary urethral realignment is accomplished, how long does the catheter stay in?
|
-6 weeks (some people would call this excessive), then get a pericatheter RUG. The suprapubic catheter is left after the urethral catheter is removed because many of these patients go on to develop symptomatic urethral stricture. If the patient voids satisfactorily via the urethra, the suprapubic catheter can be removed 7 to 14 days later
|
|
|
What if primary realignment of the urethra is not possible?
|
- SP tube alone and then delayed reconstruction is attempted after 3 months. At that point,the disruption site should be stable enough for surgery
|
|
|
What are the complications associated with repairing urethral disruption?
|
- impotence: 30-60% of patients with pelvic fracture and urethral distraction injury will
suffer some degree of impotence - incontinence: presumably due to injury to the external striated sphincter - stricture: 12-15% after urethral reconstruction |
|
|
What are the causes of anterior urethral injuries?
|
- Straddle injuries, direct penile trauma, GSWs
|
|
|
How are anterior urethral transactions usually managed?
|
- primary repair if possible with SP tube drainage
- if primary repair not possible, SP drainage for 6 weeks to 3 months followed by delayed reconstruction consisting of excision of the scar and anastomotic urethroplasty |
|
|
Which component of the GU system is most often injured by external trauma?
|
- Kidneys.
|
|
|
What is a key piece of information regarding the history of blunt trauma to the kidneys? And for penetrating trauma?
|
- blunt: the extent of the deceleration involved; rapid decels à vascular injury (ie, renal artery
thrombosis, renal vein disruption, or renal pedicle avulsion) - penetrating: bullet velocity; higher velocity projectiles impart exponentially greater kinetic energy and therefore create a larger temporary cavity on impact |
|
|
What findings on physical exam may raise suspicion of renal injury?
|
flank pain/ecchymoses/abrasions, abdominal mass/tenderness, evidence of rib fracture
|
|
|
What is the best indicator of injury to the urinary system from trauma?
|
- Hematuria [gross or microscopic ( > 5 RBCs per hpf)]
|
|
|
Does the degree of hematuria sustained after GU trauma consistently correlate with severity of injury?
|
-No, in up to 40% of injuries one can have an absence of hematuria with renal vascular injury. Notably, however, in cases of shock (i.e. SBP < 90 mmHg) in the presence of microhematuria, the severity of renal injuries is noted to increase.
|
|
|
What are the indications for renal imaging after trauma?
|
-All blunt trauma patients with gross hematuria or those with microscopic hematuria and shock (SBP < 90 mm Hg)
- Patients with a mechanism for vascular injury (rapid deceleration) since renal vascular injury can occur in the absence of hematuria - Penetrating injuries with any degree of hematuria: - Pediatric patients: more susceptible to renal injury from blunt trauma but may not manifest signs/symptoms of shock as readily as adults (secondary to release of catecholamines) |
|
|
What is the imaging modality of choice to evaluate renal trauma? What findings indicate major injury?
|
- Contrast-enhanced CT
- Major injury indicated by: 1) medial hematoma (suggests vascular injury particularly venous), 2) medial urinary extravasation (renal pelvis or UPJ injury), 3) lack of parenchymal contrast enhancement (arterial injury) |
|
|
How is single shot IVP performed? In what situation of renal trauma is it useful?
|
-a single abdominal plain film is taken 10 mins after IV injection of 2ml/kg of contrast
-can be used intraoperatively during abdominal exploration when a unexpected retroperitoneal hematoma is discovered to eval possible renal injury. Prevents need for renal exploration in 32% of cases. |
|
|
What percentage of renal injuries are significant (Grades II-V)? How are most renal injuries best managed?
|
significant renal injuries (Grades II-V) represent on 5.4% of renal trauma cases
-most significant renal injuries are best managed NONOPERATIVELY |
|
|
What is the nonoperative management after renal injury? Are any tests recommended to evaluate renal function after the acute injury resolves?
|
- Bed rest until gross hematuria clears, serial HCTs, vital sign monitoring, and hydration. May usually discharge patient if ambulation does not cause hematuria.
Recurrence of hematuria may occur w/in 21 days. If occurs, place patient back on bed rest. If hematuria persists, selective vascular embolization may be attempted before surgery as last option. - DMSA renal scan may be used as a prognostic tool for recovery of renal function |
|
|
What are the indications for operative management/exploration of a renal laceration?
|
-Absolute: persistent renal bleeding, expanding perirenal hematoma, pulsatile perirenal hematoma
Relative: urinary extravasation, nonviable tissue, delayed diagnosis of arterial injury, segmental arterial injury, and incomplete staging (often a combination of relative indications necessitates renal exploration |
|
|
What approach is best used for renal exploration? Why?
|
- transabdominal because it allows for exploration and stabilization of other abdominal viscera and vessels prior to renal exploration.
|
|
|
In exploring renal injuries, in which substantial bleeding is suspected, what is an important first step before entering Gerota's fascia and why?
|
-early vascular control
-control of the renal vessels may prevent bleeding and mitigate need for nephrectomy (controversial) |
|
|
When can renal reconstruction be attempted vs. trauma nephrectomy?
|
- reconstruction should only be attempted if the patient is stable enough to tolerate extending the
surgery. Nephrectomy is immediately indicated in extensive renal injuries when the pt’s life would be threatened by attempted repair. |
|
|
What are the main principles involved in renal reconstruction?
|
- Complete renal exposure, débridement of nonviable tissue, hemostasis by individual suture ligation of bleeding vessels (4-0 chromic sutures),
watertight closure of the collecting system (3-0 absorbable sutures), and coverage or approximation of the parenchymal defect. |
|
|
What structures may be used for coverage of a parenchymal defect?
|
pedicle flap of omentum (rich vascular/lymphatic supply), retroperitoneal fat, absorbable mesh
|
|
|
What is the cause of main renal artery thrombosis? How quickly must repair be attempted? What
techniques may be used to correct the injury? What is the main complication of repair? |
- main renal artery thrombosis usually occurs from blunt trauma caused by rapid deceleration
- repair must be attempted within 8 hours before viability of tissue is lost - interposition graft with hypogastric or splenic arteries; possibly endovascular stenting - hypertension |
|
|
When should segmental renal artery injuries be surgically addressed?
|
- when they are associated with parenchymal laceration with infarction of > 20% of the kidney
|
|
|
How should main renal vein injuries be managed? Segmental venous injuries?
|
- main renal venous injuries require surgical repair with fine 5-0 vascular sutures
- segmental renal venous injuries can be managed by ligating the vessel due to collateralization of the renal venous system |
|
|
What are the main complications associated with renal trauma? How may they usually be managed?
|
persistent urinary extravasation, leading to urinoma formation and perinephric infection: systemic antibiotics, spontaneous resolution
-delayed renal bleeding: initial management with bed rest, hydration. if persists, consider angiography and embolization -perinephric abscess: percutaneous drainage - hypertension: caused by stenosis/occlusion of renal artery or major branches, compression of renal parenchyma with extravasated urine/blood, and/or renal ischemia (stimulation of renin-angiotensin axis) |
|
|
Is ureteral injury commonly caused by external trauma? What percentage of penetrating trauma involves the ureter? Blunt trauma?
|
- No
- 4% - 1% |
|
|
What types of injuries in the blunt trauma patient should raise suspicion for ureteral injury?
|
-fractured lumbar processes
-thoracolumbar spinal dislocation |
|
|
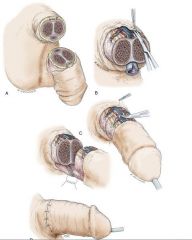
What is the scale for renal trauma?
|
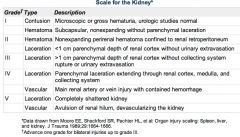
|
|
|
List the more common iatrogenic modes of ureteral injury?
|
1) Open surgical procedures especially hysterectomy (54%) , colorectal surgery (14%) , pelvic surgery (i.e. ovarian tumor removal) and abdominal vascular surgery (aorto-iliac/femoral bypass surgery-6%)
2) Laparoscopic surgery especially gynecologic surgeries such as lysis of endometriosis 3) Ureteroscopic injury |
|
|
What are current recommendations for preventing ureteral injury during ureteroscopy?
|
- when a ureteral tear is recognized during USE, stop and place a stent
- perform ureteroscopy alongside a wire placed up into the renal pelvis - use smaller, flexible ureteroscopes; avoid ureteroscopy in previously irradiated tissue |
|
|
What are the common ways in which ureteral injuries due to external trauma may be diagnosed?
|
- intraoperative recognition: since laparotomy is often required in the population of trauma pt’s most at risk for ureteral injury. (assisted by 1-2cc injection of methylene blue into renal pelvis)
- excretory urography: one shot IVP intra-operatively - retrograde ureterography |
|
|
What are some limitations to these diagnostic tools?
|
- excretory urography: findings subtle, non-specific (delayed function, ureteral dilation, and ureteral deviation)
- Contrasted CT: must have delayed images to be diagnositic - Retrograde ureterography: not useful in the acute trauma setting, but may be helpful if ureteral stent to be placed. |
|
|
What are the clinical manifestations of missed ureteral injury?
|
fever, leukocytosis, and local peritoneal irritation (constellation should prompt CT evaluation)
|
|
|
What are the principles of surgical ureteral repair?
|
Mobilize the injured ureter carefully, sparing the adventitia widely to prevent devascularization.
Débride the ureter liberally until the edges bleed Repair ureters under magnification with spatulated, tension-free, stented , watertight anastomosis (absorbable suture) placing retroperitoneal drains afterward. Consider omental interposition to isolate the repair when possible |
|
|
If a patient is too unstable to undergo immediate repair of ureteral injury, what are some management options?
|
- planned staged repair: the damaged ureter is tied off using long silk ties to aid the dissection of the ureteral stump during the second stage. Then perc. neph tubes may be placed to drain the kidney
- nephrectomy: usually in the setting of severe associated visceral injury or injury to the ipsilateral kidney |
|
|
What are the options for surgical management of UPPER ureteral injury?
|
- Ureteroureterostomy
-ureterocalycostomy-when profound damage to renal pelvis or UPJ -autotransplantation (for profound ureteral loss or multiple failed attempts at ureteral repair) of kidney -bowel interposition: use of ileum, large bowel to form a ureter. |
|
|
What are the options for midureteral injury?
|
- UU or transureterostomy (often perfomed as a secondary or delayed procedure, great care should be exercised
with TU-? iatrogenic injury to uninvolved ureter. If available, probe PMH for urothelial cancer, stone disease) *Also could de an ileal ureter |
|
|
What are the options for distal ureteral injury?
|
- Ureteroneocystostomy: submucosal tunnel that is three times longer than the width of the ureter. The authors recommend post-operative stenting.
- Psoas hitch: preferable to UU since the blood supply to the distal ureter is tenuous and might not survive transaction - Boari flap: for long gap distal ureter injuries; not useful in the acute setting |
|
|
How due the authors recommend handling initially missed ureteral injuries?
|
-attempt retrograde stenting (successful only 20-50% of time)
-if that fails, nephrostomy tube with gentle attempt at antegrade stenting - if that fails, wait 7-14 days and attempt antegrade stenting again - finally, leave nephrostomy tube for several months for complete wound healing before attempting open surgical repair |
|
|
A 20 year old man sustains a circumferential avulsion of the skin of the mid-shaft of the penis. There is intact skin on both the proximal and distal aspects of the penile shaft, with a denuded area 4 cm in length. The most appropriate treatment is what?
|
*Split thickness skin graft and removal of the distal penile skin as a 4cm gap if covered by simple re-approximation will be cosmetically displeasing. Therefore a split thickness skin graft should be used. The distal skin should be removed if it is not removed then interposed split thickness skin graft will cause obstruction of the normal lymphatic drainage of the distal skin and lymphedeme will result.
|
|
|
Massive extravasation of urine into the pelvis and resultant absorption of urine would cause what kind of electrolyte abnormalities?
|
*Hyperchloremic, hyperkalemic metabolic acidosis would result.
|
|
|
What is silicone injection into the penis and what will it do how can it be corrected?
|
Silicone injections are exactly what they sound like — injections of silicone into the body, and in this context generally (but not exclusively) to the male genitalia. The potential changes are, for lack of a better word, "monstrous." As far as male genital injections, circumference increases of as much as three hundred percent are definitely not unheard of. Done slowly, the level of sculpting that can be achieved is almost limitless.
In general, this procedure is not reversible, at least without extensive invasive and damaging surgery. The only way to reverse the changes is to remove the skin completely and perform penile skin graft surgery. |
|

|

|
|
|
If a patient has a penile amputation and there isn't a microsurgeon at your hospital and the patient can be transferred to one, how should you prepare the amputated penile segment and how long do you have as far as time before its too late?
|
The amputated portion of the penis should be cleaned, wrapped in a sponge soaked in sterile saline, and placed in a sterile zipper-sealed plastic bag. This is kept in ice slush, and replantation can be accomplished as long as 18 hours after amputation.
|

