![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
Which sex has the longer urethral sphincter mechanism?
|
Females
|
|
|
the 2 phases of the micturition cycle are?
|
Storage
Voiding |
|
|
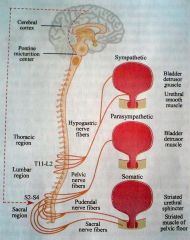
Neurophysiology of micturition
|
|
|
|
Afferents and Efferents to the Bladder
|
Afferents
1. Parasympathetic desire to void pain/temperature 2. Sympathetic sensation of fullness pain/temperature Efferents ( Motor ) 1. Parasympathetic ( S2,3,4 ) Detrusor motor nucleus 2. Sympathetic ( T10 - L2 ) Bladder neck - alpha1 detrusor relaxation - beta3 |
|
|
Difference between "desire to void" and "sensation of fullness"?
|
sensation of fullness in SNS and can be supressed (eg watching a movie till you get a desire to void)
|
|
|
Urethra & Pelvic Floor Neurophysiology
|
1. Smooth Muscle Sphincter
( internal sphincter ) : alpha-adrenergic ( T10 - L2 ) 2.Striated Muscle Sphincter ( rhabdosphincter / external sphincter ) & Pelvic Floor : somatic ( S2,3,4 ) |
|
|
Higher Centres in Micturition
|
Pontine Micturition Center (PMC)
Receives afferents from bladder stretch receptors & send efferents to detrusor motor nucleus to initiate micturition reflex Receives input from cortex and CO-ORDINATE micturition Cerebral Cortex Frontal lobe Insula |
|
|
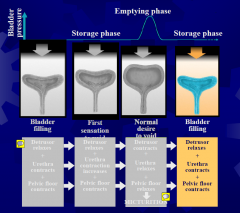
The Storage & Micturition Reflexes & Their Relationship to the Normal Micturition Cycle
|
|
|
|
Micturition (Voiding) Reflex
|
Central inhibition of this reflex learned in toilet-training
1.Central inhibition lifted ( voluntary – frontal lobe ) 2.Rhabdoshpincter ( urethral ) relaxation 3.Urethral pressure drop ( 3-5 sec ) 4.Detrusor contraction 5.Voiding begun & maintained till bladder empty 6.Detrusor Relaxation and Restoration of Rhabdosphincter tone 7.Cycle starts again next time desire to void is reached |
|
|
spinal cord Injury at level S1
- effect on mictruition? |
sospinal cord injury just at S1 will fill and void by itself ( no sensation)
-OMC and Cortex still working |
|
|
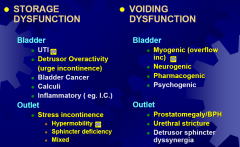
Storage Sx
|
Frequency
Urgency Urgency incontinence Nocturia The Overactive Bladder Syndrome ( OAB ) Suggest storage disorder |
|
|
Definition of Nocturia
|
waking up more than once in the night time to void
|
|
|
Voiding Sx
|
Hesitancy
Intermittency Slow flow Terminal dribbling Incomplete emptying Suggest voiding disorder |
|
|
Incontinence occurs only when?
|
Occur ONLY when intravesical pressure > urethral closure pressure ( resting urethral tone )
it is both a sign and a Sx |
|
|
# main types of Incontinence
|
3 main types : stress, urge, overflow
|
|
|
Classification of Bladder Dysfunction (common ones in yellow)
|
|
|
|
Hypermobility
|
the urethra due to poor pelvic support
|
|
|
Overactive Bladder (OAB)
|
Is a symptom complex that includes urgency, with or without urge incontinence, usually accompanied by frequency and nocturia1
Occurring in the absence of pathologic or metabolic factors that would explain the symptoms2 OAB-dry OAB-wet |
|
|
Prevalence of OAB
|
Estimated prevalence:
15 % of people aged 18 years and over2 OAB is likely to affect an estimated 1.5 million Australians aged over 40 years* |
|
|
Causes of OAB
|
1. Non-neurogenic OAB
Idiopathic From outflow obstruction ( eg. BPH, CaP, Stricture ) Bladder cancer 2. Neurogenic Detrusor Overactivity Dementia, Stroke, Parkinson‟s Disease Spina bifida Suprasacral spinal cord injury |
|
|
Careful History
|
Careful History
Symptomatology Storage, voiding or mixed symptoms Motor vs Sensory urgency „I know where all toilets are when I go out‟ Severity pad usage bothersomeness ( QoL ) associated haematuria „Think Outside the Bladder‟ Caffeinated beverages, EtOH Past Hx : gynae/pelvic surgery, neurological Social Hx : smoking, occupation |
|
|
Focussed Physical Examination
|
Focussed Physical Examination
Focussed examination Bladder Palpation Bedside ultrasound “Outside the Bladder” Vagina - pelvic organ prolapse, atrophic vaginitis Penis - meatus stenosis Prostate – rectal exam S2-S4 - Neurological exam |
|
|
Ix
|
MSU, PVR, voiding diary
Gold standard is URODYNAMICS |
|
|
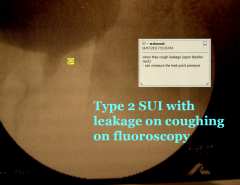
Urodynamics
|
Simulates the 2 phases of the Micturition Cycle
1. Storage phase Bladder slowly filled with diluted contrast medium Pt reports sensations of filling, fullness, & urgency Look for detrusor instability or poor compliance Coughing/Valsalva to detect stress incontinence Assisted by Fluoroscopy or U/S 2. Voiding phase Simultaneous recording of flow rate and detrusor pressure during voiding to type of voiding disorder (eg. Obstruction vs Hypocontractile bladder ) Assisted by Fluoroscopy or U/S |
|
|
Truw Detrussor Pressure in Urodynamics
|
true detrussor pressure with a needle in the bladder neck
but we do red minus green (bladder pressure minus rectal pressure) |
|
|
General Schema of OAB Treatment
|
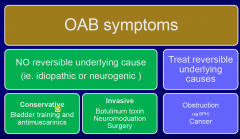
Conservative
Bladder training and Pelvic Floor exercises ( 3 months ) Behavioural modification ( reduced fluids, postponement ) Anticholinergics with bladder training – the BEST Minimally Invasive Intravesical agents ( eg. Botulinum toxin A ) Sacral neuromodulation Permanent IDC or SPC Invasive Clam ileocystoplasty ( bladder augmentation ) Diversion with ileal conduit |
|
|
Antimuscarinics ( also known as anticholinergics
|
Less uro-selective
Oxybutynin ( Ditropan R ) Propantheline ( Probanthine R ) Tolterodine ( Detrusitol R ) More uro-selective Solifenacin ( Vesicare R ) Darifenacin ( Enablex R ) |
|
|
Anticholinergic side effects
|
Salivary : dry mouth
GIT: constipation Eyes: blurred vision, exacerbate glaucoma CNS: drowsiness CVS: palpitations, ankle oedema |
|
|
Comparing Anticholinergics
|
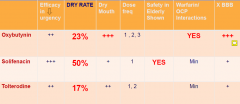
|
|
|
Botulinum Toxin -A
|
Botulinum Toxin -A
Inhibits pre-synaptic release of acetylcholine, ie blocks neuromuscular transmission Non-neuropathic : 100-150 U Neuropaths : 300 U Can top –up after 6-9 months Side-effects: Slight hematuria Retention ( approx. 10% ) Potentiated by gentamicin Case reports of systemic toxicity |
|
|
Take Home Messages for Bladder Overactivity
|
1.MSU, PVR, voiding diary are essential
2.Bladder Cancer is a great mimicker (short term 2-3months) 3.Urodynamics indicated if empirical drugs fail 4.Anticholinergics and BT are cornerstone of therapy |
|
|
Female Stress Urinary Incontinence
|
Worldwide problem
Account for 30% of female incontinence cases age, parity, prolonged 2nd stage labour, pelvic floor prolapse Stress incontinence both a SYMPTOM and a SIGN, but NOT A DIAGNOSIS. „Urodynamic stress incontinence (USUI)‟ is a DIAGNOSIS, based on videourodynamics : defined by urethral leakage when intravesical pressure exceeds urethral closure pressure, in the absence of a bladder contraction. |
|
|
Two Types of USUI
|
1. Urethral Hypermobility ( Type 2 )
From laxity/weakness of pelvic support structures Rotational descent of bladder base with distraction of bladder neck and urethra Characterised by HIGH leak-point pressure CAUSES - age, parity, pelvic prolapse 2. Intrinsic Sphincter Deficiency ( Type 3 ) Reduction in external sphincter muscle mass AGEING : gradual reduction in sphincter mass Characterised by LOW leak-point pressure CAUSES - age, previous incontinence ops, pelvic irradiation or surgery, infrasacral cord injury |
|
|
Type 2 Stress Incontinence
|
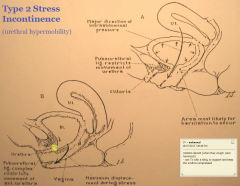
the rotation allows the urthera to open (thus leakage)
Tx can be in the form of a surgical sling to properly support the bladder and avoid this rotational decent |
|
|
History and Examination SUI
|
Typically leaks on coughing, laughing, picking up children, sporting activities
Gauge severity by number of pads used or degree of restriction with daily activities Abdomen Vagina : leak on coughing with urethral descent visible +/- atrophic vaginitis +/- prolapse Lower limb neuro exam - exclude neurogenic bladder |
|
|
Initial Investigations for SUI
|
MSU
PVR Videourodynamics warranted if symptoms bad / surgery is planned in complex cases differentiate between hypermobility and ISD, exclude DO |
|
|
Treatment for Type 2 SUI
|
Treatment for Type 2 SUI
1. Conservative Pelvic Floor Exercises Cure and improved in up to 75% in 6 months Nurse continence advisor Brochures from Continence Foundation of Australia Reduce abdominal strain Weight loss Chronic cough 2. Surgical A) Synthetic Slings At mid-urethra ( Eg. TVT ) Minimally invasive Day-only B) Pubovaginal Sling At Proximal urethra and bl. neck C) Injectables D) Artificial urinary sphincter |
|
|
Take Home Messages SUI
|
SUI is not „normal‟. Treatment is available to those who are significantly bothered
Conservative Rx first Pelvic Floor exercises Weight Loss Referral to urologist for surgery if conservative fails Good and durable outcome from currently available synthetic midurethral and fascial pubovaginal slings In general, > 85% improved still at 8 years post-op |
|
|
Case Scenario - Nocturia
62 yo Nocturia 5-6 x – at least 300-400ml each “does not pass that much during daytime” Losing sleep O/E : ankle oedema, PR : prostate smooth 30g ISSUES? |
Passes more at night than day ( polyuria, not frequency )
Fluid consumption in evening ( esp. caffeinated ) ?insomnia ? CCF |
|
|
NOCTURIA
2 types |
1.Nocturnal frequency
Often due to ageing Other causes : BPH, OAB, insomnia 2.Nocturnal polyuria > 50% urine output during sleep than when awake Idiopathic - ? Decreased renal sensitivity to ADH Secondary – CCF, diabetes mellitus or insipidus |
|
|
Common Voiding Disorders
|
1. Bladder
Bladder underactivity (hypocontractile bladder) 2. Outlet Outflow obstruction BPH, Prostate cancer Urethral stricture |
|
|
Case Scenario
70 yo 2 yrs of poor flow, abdominal straining to void, frequency, urgency, nocturia 5-6x, nocturnal incontinence O/E : not distressed; bladder almost at umbilicus; PR : moderately enlarged P Cr, MSU, PSA normal US – 1000cc with 500 cc post-void residual |
Bladder Hypocontractility
|
|
|
Detrusor Hypocontractility
|
Detrusor Hypocontractility
Predominately a Geriatric voiding dysfunction Often present as overflow incontinence or nocturnal enuresis Often secondary to chronic silent outlet obstruction, but can be idiopathic Characterised by : mixed S and V symptoms and esp. nocturnal incontinence Hypo- or acontractile bladder with low flow on urodynamics Treatment : Cholinergics + a-blocker : worth a try Double-voiding technique if still has contractility – monitor PVR regularly Clean Intermittent self-catherisation ( CISC ) ! SPC or IDC if can‟t CISC |
|
|
Case Studies At the end of the lecture
|
...
|

