![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
|
A 26-year-old woman comes to clinic complaining of a "bad cold." She woke up three days ago with sore throat and rhinorrhea. She complains of fatigue, and her nose is sore from frequently blowing it. She has a headache. She states that after 2 days of symptoms, phlegm turned from clear to yellow/green. The most likely cause of her infection is:
|
Rhinoviruses account for 30-50% of the "common cold", followed by coronaviruses (7-18%) and influenza (5-7%). Less common causes include respiratory syncytial virus, parainfluenza viruses, adenoviruses, and enteroviruses.
|
|
|
A 46-year-old business man comes in complaining of an upper respiratory tract infection, and you confirm the diagnosis. He is unhappy with being sick; it's the fourth cold he's had since last summer. Past history is notable for hypertension and tobacco use. He is sedentary. Physical examination is normal, except for findings consistent with an upper respiratory tract infection. The most effective means for prevention of future colds in this individual is:
|
Despite all the folklore, the single most effective means to reduce the risk of contracting an URI is to engage in frequent hand washing. Psychological stress is associated with increased risk of contracting an upper respiratory tract infection.
|
|
|
A 56 year-old woman with hypertension and a pack-a-day smoking history presents with 4 days of rhinitis, nasal congestion, sore throat, cough, and headaches. She requests antibiotics because she “developed a real bad pneumonia” after her last cold. Which of the following is correct regarding the risk of bacterial complications following URI?
a). Significant nasal discharge and "chest congestion" are predisposing factors for pneumonia leading to pneumonia in 5% of patients. b). Bacterial sinusitis is the most common bacterial complication of URTI, complicating <2% of cases. c). Lemierre’s syndrome is a common complication of URI and should be suspected in patients with persistently sore throats. d). Patient with viral upper respiratory tract infections do not develop bacterial complications. |
Bacterial complications from URTI and influenza are rare, but do occur. Bacterial sinusitis is the most common bacterial complication of URTI, yet occurs in <2% of cases. Bacterial pneumonia may complicate influenza, but is rare. This often occurs 4-10 days after symptomatic influenza is diagnosed, and may be due to S. pneumoniae, H, influenza, or S. aureus, including MRSA. Lemierre's syndrome is a rare complication of either viral or bacterial pharyngitis. Pharyngeal inflammation may lead to invasive infection by Fusobacterium necrophorum, followed by sepsis and internal jugular vein thrombosis. Classic symptoms are high fevers and rigors occurring as early as two days after the onset of sore throat.
|
|
|
A patient is distraught because in the past 2 days he developed cold symptoms just as he has an important upcoming business meeting to prepare for. He is desperate to reduce his symptoms and requests guidance on cold remedies. Which of the following advice is correct?
a). Diphenhydramine is superior to second generation antihistamines, such as fexofenadine or loratadine, for treating rhinorrhea. b). Echinacea is proven effective at reducing duration of symptoms of the common cold. c). Zinc is effective at shortening common cold symptoms if given within the first 48H of symptoms. d). Antibiotics are indicated if symptoms persist for more than 7 days. |
Since there is no cure for the common cold, treatment is focused on symptom management. First generation antihistamines are effective at reducing rhinorrhea and sneezing. Antibiotics are ineffective at treating URI, as are echinacea, zinc, and vitamin C.
|
|
|
Regarding influenza virus, which one of the following statements about antigenic drift and antigenic shift is true?
a). Antigenic drift causes more severe outbreaks in a population than does antigenic shift. b). Antigenic drift results from mutations in the HA and NA glycoprotein genes. c). Antigenic drift can happen with influenza A, but is not described with influenza B. d). Antigenic shift can happen with influenza B, but is not described with influenza A. |
Antigenic drift, which occurs with influenza A and influenza B, results from small changes in viral antigens due to mutations during the replication cycle of the virus. Antigenic shift, which occurs only with influenza A, is due to a major change in viral antigens due to gene re-assortment, which may result in severe pandemics of infection.
|
|
|
In early 2009 the novel H1N1 influenza virus was identified and, initially referred to as swine ‘flu. This virus emerged as a result of which of the following?
a). Antigenic shift of an H1N1 influenza A virus b). Antigenic shift of an H3N1 influenza A virus c). Antigenic drift of an H1N1 influenza A virus d). Antigenic drift of an H3N1 influenza A virus |
The 2009 pandemic novel H1N1 “swine flu” caused more severe illness because most individuals lacked partial immunity. Antigenic drift of seasonal influenza generally results in varying degrees of immunity from season to season.
|
|
|
You are evaluating a 32-year-old male who presents for a new patient physical. He describes an illness that he had three months ago, and was treated in an urgent care center. Blood work was drawn, but he does not recall the results. He describes having had a four-week illness, with daily fevers, swollen glands, headache and myalgias. He had no rash, but his girlfriend thought he looked "yellow" for a few days. He recalls the doctor at the urgent care center noted his spleen was enlarged. Which one of the following is likely to be among his lab results when you obtain his records?
a). Transaminase elevation; atypical lymphocytosis; influenza A viral culture positive b). Leukocytosis; normocytic anemia; influenza B viral culture positive c). Thrombocytopenia; atypical lymphocytosis; EBV IgM positive d). HIV antibody negative; HIV viral load positive |
Influenza, acute HIV seroconversion, and EBV infection have significant clinical overlap, and can be difficult to distinguish. However, acute EBV infection results in more severe liver inflammation and even jaundice, often with splenomegaly. Atypical lymphocytes are seen with acute HIV and EBV, but not with influenza. All three infections are associated with myalgias and arthralgias, and may also result in thrombocytopenia.
|
|
|
Influenza A is epidemic in your community. A patient calls with symptoms highly suggestive of influenza infection, which began 36 hours ago. Which treatment is most appropriate at this time?
a). Amantadine b). Rimantadine c). Oseltamivir d). Acetaminophen/fluids; it is too late for antivirals to be effective |
Treatment of otherwise healthy individuals for influenza with antivirals must be initiated within the first 48H of symptoms (the sooner the better). Amantadine and rimantadine treat influenza A infection, while oseltamivir and zanamivir treat both influenza A and B. Drug resistance to amantadine and rimantadine approaches 95% for H3N2 influenza A. Resistance to oseltamavir (but not zanamivir or peramivir) is common among seasonal H1N1 and some novel-H1N1 isolates. Thus selecting optimal antiviral agents depends on knowing local epidemiology.
|
|
|
A 25-year-old resident physician has severe egg allergy and asthma, and is about to rotate through the Emergency Department at the peak of influenza season. Prevention of influenza A and influenza B in this individual should be obtained by:
a). Administration of intranasal influenza vaccine b). Amantadine daily c). Oseltamivir daily d). Zanamivir daily |
The history of a severe reaction is a contraindication to repeating use of the influenza vaccine. Amantadine has multiple side effects and is ineffective against most H3N2 due to viral resistance. Zanamivir is contraindicated among individuals with lung disease (and is not approved for control of influenza outbreaks in nursing homes). Oseltamivir, despite high level seasonal H1N1 resistance, is the best choice for chemoprophylaxis.
|
|
|
A 43-year-old woman with diabetes presents for follow up. She was diagnosed with influenza three weeks ago, and was treated with supportive care. She improved, but three days ago, productive cough and dyspnea worsened, along with new fevers. You obtained a chest x-ray today, which shows a left lower lobe infiltrate. Of the causes listed, which is the most likely etiology of her pneumonia?
a). Influenza A virus b). Influenza B virus c). Staphylococcus aureus d). Pseudomonas aeruginosa |
Post-influenza pneumonia is relatively rare, but can lead to severe bacterial pneumonia, even in previously healthy young adults. The patterns of symptoms are typically worsening, or recurrence, of fever and development of new respiratory symptoms after an initial improvement. Over the past 5 – 6 years, severe post-influenza pneumonias caused by community associated MRSA have become more common and need prompt initiation of antibiotic management for optimal outcomes.
|
|
|
A 22-year-old woman presents with complaints of three days of sore throat and cough. On exam, she is febrile (T 38.3C), with tender anterior cervical adenopathy. Small white plaques are noted on her tonsils. Appropriate management at this point would be:
a). Empiric treatment with penicillin b). Empiric treatment with amoxicillin c). Rapid-strep antigen testing; antibiotics only if positive d). Throat culture; penicillin now until resistance patterns known |
Centor criteria are as follows:
T>38.0 Tonsillar exudates Tender cervical adenopathy No cough or rhinitis If 0-1 of these is present, no testing is indicated and treatment is symptomatic. If 2-3 criteria are present, rapid-strep testing is indicated, with treatment only if positive. If all 4 criteria are present, treatment with antibiotics is appropriate (as is rapid-strep testing with antibiotics if positive). |
|
|
A 32-year-old woman is diagnosed with streptococcal pharyngitis after a throat culture done at an urgent care center grows group A beta-hemolytic streptococci. She has no significant past medical history, is on no medications, and has no allergies. Among the treatment options listed, which is the best treatment?
a). Penicillin b). Doxycycline c). Azithromycin d). Ciprofloxacin |
Treatment of choice for group A beta-hemolytic streptococcal pharyngitis is penicillin for 10 days. Erythromycin or azithromycin is appropriate for the penicillin-allergic patient.
|
|
|
A 49-year-old woman with no significant past medical history comes to clinic complaining of mild nasal congestion and headache for the past four days. Symptoms began with a sore throat and, by her account, quickly settled in her sinuses. She blows her nose and shows you that the discharge is a yellowish-tan color. Which one of the following is true?
a). This patient should be provided symptomatic management with NSAIDS and first generation antihistamines. b). She should receive nasal saline lavage to relieve symptoms and prevent progression to bacterial sinusitis. c). Amoxicillin-clavulanate should be prescribed for this woman with acute bacterial sinusitis. d). If antibiotics are used and she has a history of previous rhinosinusitis, a 3rd generation fluoroquinolone that has activity against Pseudomonas aeruginosa should be used. |
Answer - A
Over-treatment with antibiotics is common with sinusitis, and sinus inflammation and congestion are common with viral URTI (as are purulent nasal discharge, headache, and maxillary tooth pain). The history and physical exam are not particularly useful in distinguishing viral from bacterial sinusitis (i.e. rhinosinusitis). Imaging of the sinuses is not indicated in the typical patient with sinusitis; air/fluid levels and edema are noted with both viral and bacterial infection. Features of the presentation that are of clinical use in distinguishing viral from bacterial sinusitis include: Presence of symptoms > 7 days Maxillary tooth pain Unilateral face pain Unilateral sinus tenderness Fever Purulent nasal discharge Symptoms worsening after initial improvement If antibiotics are indicated, appropriate therapy options include amoxicillin, doxycycline, or trimethoprim/sulfamethoxazole. |
|
|
A 37-year-old man presents with 10 days of acute bacterial rhinosinusitis. Past medical history is notable for type 1 diabetes, complicated by osteomyelitis of his left great toe, requiring antibiotics and amputation done just three weeks ago. On exam he is febrile, and has left maxillary sinusitis. Appropriate treatment at this point would be:
a). Amoxicillin b). Doxycycline c). Levofloxaxin d). Itraconazole |
Narrow spectrum antibiotics such as amoxicillin, doxycycline, and trimethoprim-sulfamethoxazole are most appropriate for treating uncomplicated bacterial rhinosinusitis in an individual without antibiotic exposure in the past 6 weeks. Individuals with recent antibiotics exposure are more likely to harbor resistant bacteria. For those patients, amoxicillin/clavulanic acid, moxifloxacin, and levofloxacin are reasonable choices.
|
|
|
A 19-year-old male smoker presents with a one-week history of cough productive of yellow/green sputum. He has mild dyspnea. Which ONE of the following statements is true?
a). Common causes of bronchitis include Streptococcus pneumoniae, Mycoplasma pneumoniae, and Chlamydophila pneumoniae. b). Because of his purulent sputum, he is likely to have a bacterial bronchitis. c). Normal vital signs and a normal chest exam make pneumonia an unlikely explanation of this patient's dyspnea. d). If wheezing is noted on physical exam, he likely also has asthma. |
c). Normal vital signs and a normal chest exam make pneumonia an unlikely explanation of this patient's dyspnea.
Infectious causes of bronchitis include viral and bacterial causes. The most common cause of bronchitis is rhinovirus, followed by other common causes of the "common cold". The most common bacterial causes are Mycoplasma pneumoniae and Chlamydophila pneumoniae. There is no clinical evidence to suggest that smokers are more likely to develop bacterial bronchitis relative to viral bronchitis. Pneumonia is the major disorder that must be differentiated from bronchitis. Although pneumonia is a rare complication of bronchitis, if fever, tachypnea, or dyspnea is present, or there is pulmonary consolidation on physical exam, a chest x-ray should be obtained to exclude pneumonia. Wheezing is a common finding in acute bronchitis, and should not prompt the diagnosis of asthma. |
|
|
What is the most consistently demonstrated risk for the development of URTIs?
|
psychological stress is the most consistently demonstrated risk for development of URTI
|
|
|
Smoking and URTIs
|
Smoking, a risk for lower respiratory infections, has not been demonstrated to increase the risk for upper respiratory infections. However, smoking does increase duration and severity of URTI.
|
|
|
What is the most common complications of URTIs?
|
The most common complication of URTI is asthma or COPD exacerbation in those at risk.
Very rarely (i.e. <2% of cases) do URTIs progress to bacterial infection in adults, usually bacterial sinusitis or otitis media. |
|
|
Management of URTIs
|
Although the understanding of URTI pathophysiology has advanced greatly, treatment has not changed significantly in the past decade. Indeed, trials of potential therapeutic agents have consistently demonstrated a lack of efficacy. Current therapy of URTI is based on symptomatic management. Oral decongestants such as phenylephrine (Neo-Synephrine and other brand names) and pseudoephedrine (Sudafed) and topical nasal decongestants such as ipratropium nasal spray (Atrovent Nasal) relieve rhinorrhea and nasal congestion. Oxymetazoline (Afrin) is another topical nasal decongestant, however use for as little as three days may lead to rebound nasal congestion (rhinitis medicamentosa), thus it should be recommended with caution. First-generation antihistamines (e.g., diphenhydramine) are more effective in reducing rhinorrhea and sneezing than second-generation antihistamines (e.g., loratadine), due to their greater anticholinergic properties. Non-steroidal anti-inflammatory drugs may help with sore throat, headache, and fever. Not surprisingly, trials of antibiotics have failed to demonstrate benefit. A variety of supplements and naturopathic products have been promoted for treatment of URTI. Those most studied have been vitamin C, zinc, and Echinacea, none of which have demonstrated efficacy in blinded studies.
|
|
|
Good hand hygeine reduces URTIs by what amount?
|
Washing hands and keeping them away from the eyes and mouth reduces frequency of URTI by approximately 20%
|
|
|
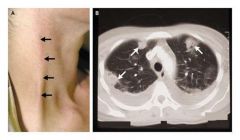
Lemierre's syndrome is a rare complication of either viral or bacterial pharyngitis (Figure 2). Pharyngeal inflammation may lead to invasive infection by Fusobacterium necrophorum, followed by sepsis and internal jugular vein thrombosis. Classic symptoms are high fevers and rigors occurring as early as two days after the onset of sore throat.40 On examination, tenderness is often detected over the sternocleidomastoid muscle. Septic jugular vein thrombosis can lead to septic emboli lodging in the lungs and the classic cannonball finding on computed tomography of the chest. Treatment is with antibiotics with good anaerobic activity, such as ampicillin-sulbactam or clindamycin.
|

