![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
118 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
calcium total
|
decreased: malabsorption, renal failure, acute pancreatitis
|
9-10.5 values decrease in elderly
|
|
|
potassium
|
decreased: vomiting, gastric suction, diarrhea, drainage from interstitial fistulas
|
3.5-5
|
|
|
albumin
|
decreased: hepatic disease
|
3.5-5
|
|
|
ALT
|
increased: liver disease, hepatitis, cirrhosis
|
8-20 units
|
|
|
AST
|
increased: liver disease, hepatitis, cirrhosis
|
5-40 units
|
|
|
alkaline phosphatase
|
increased: hepatic disease, biliary obstruction
|
42-128 units
|
|
|
Bilirubin
|
increased: hemolysis, biliary obstruction, hepatic damage
|
0.1-1.0
|
|
|
conjugated bilirubin
|
increased: biliary obstruction
|
0.1-0.3
|
|
|
unconjugated bilirubin
|
increased: hemolysis, hepatic damage
|
0.2-0.8
|
|
|
ammonia
|
increased: hepatic disease like cirrhosis
|
15-110
|
|
|
Xylose absorption
|
decreased values in blood and urine indicate possible malabsorption in small intestine
|
5g dose in 2h=> 20
25g dose in 2h=> 25 |
|
|
serum amylase
|
increased: acute pancreatitis
|
25-125 units
|
|
|
serum lipase
|
increased: acute pancreatitis
|
0-110
|
|
|
cholesterol
|
increased: pancreatitis, biliary obstruction.
decreased: liver cell damage |
<200
|
|
|
carbohydrate antigen 19-9 (CA19-9)
|
increased: cancer of pancreas, stomach, colon. acute pancreatitis, inflammatory bowel disease
|
<37
|
|
|
carcinoembryonic antigen (CEA)
|
increased: colorectal, stomach, pancreatic cancer. ulcerative colitis, crohns disease, hepatitis, cirrhosis
|
nonsmoker: <2.5
smoker: up to 5 |
|
|
digestion is the process of breaking down complex food into nutrients the body can absorb and convert into energy
|
once absorption has taken place the GI system excretes any unabsorbed materials
|
|
|
|
GI system changes with aging
|
stomach: <HCL acid levels, encourage bland foods high in vitamins and iron which help prevent gastritis, assess for epigas pain helps detect gastritis
Intestines: <peristalsis leads to constipation and impaction, encourage high fiber diet and 1500mL fluid daily and encourage activity. pancreas:<lipase production which leads to steatorrhea, encourage small meals and assess for diarrhea which can lead to dehydration liver:<protein synthesis and enzyme activity, decreased drug metabolism which leads to toxic levels, assess for adverse effects of drugs. |
|
|
|
mucosa
|
innermost layer includes a thin layer of smooth muscle and exocrine gland cells
|
|
|
|
submucosa
|
layer surrounded by the muscularis and the muscularis is composed of both circular and longitudinal smooth muscles which work to keep contents moving through GI tract.
|
|
|
|
USE
|
upper esophageal sphincter when at rest is closed to prevent air into thr esophagus during respiration
|
|
|
|
LES
|
lower esophageal sphincter when at rest is normally closed to prevent refluc of gastric contents into the esophagus. if the LES doesn't work properly rrfluc disease or GERD can develop.
|
|
|
|
the atrium(pylorus)
|
or distal part of the stomach is seperated from the duodenum by the pyloric sphincter.
|
|
|
|
parietal cells
|
line the wall of the stomach and secret HCL acid and intrinsic factor which is a substance that aids in the absorption of vitamin B12(absence of I.F. causes pernicious anemia.
|
|
|
|
the liver is the largest organ in the body
|
in thr URQ, transports bile, recieves blood from thr hepatic artery and portal vein and stores fat soluble vitamins ADEK, iron and magnesium.
|
|
|
|
kupffer cells
|
the protective function of liver in which they engulf harmful bacteria and enemic red blood cells and detocifies harmful compounds.
|
|
|
|
the metabolism of the liver
|
breaks down amino acids to remove ammonia which is turned into urea and excreted through the kidneys.
stores and releases glycogen as the bodys energy requirements change. also temp stores and breaks down fatty acids and triglycerides. forms and cont secretes bile which is essential for fatt breakdown and secreted into the duodenum or SOO if the sphincter is closed it goes into the gallbladder for storage. |
|
|
|
the gallbladder is
|
underneath thr liver and releases stored bile via the common bile duct.
|
|
|
|
Assessment History of GI system
|
PT hx: older adults are more likely to get stomach cancer whereas younger are to get IBD. Large amounts of NSAIDS can lead to peptic ulcer disease n GI bleeding. smoking is a major risk for GI cancers.
nutritional hx: anorexia which is loss of appetite assess for nv or dyspepsia abd pain associated with esophageal disorders. socioeconomic status: limited budget like older adults or unemployment may not be able to purchase required food for a balanced diet. family hx: FAP is an enherited autosomal dominant disorder thst predisoses a pt to colon cancer. current health problems: ask about patterb color consistency of bowels if pt has diarrhea or constipation and any measures to fix this, if blood or tarry stools and if any abd distention or gas. |
|
|
|
URQ organs
|
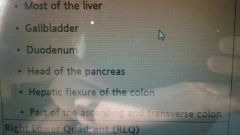
|
|
|
|
RLQ organs
|
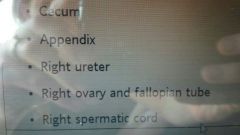
|
|
|
|
LUQ organs
|
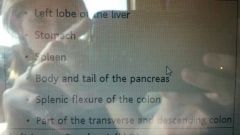
|
|
|
|
LLQ organs
|
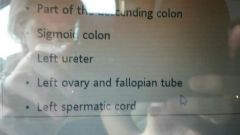
|
|
|
|
nursing action
|
|
|
|
bowel sounds after surgery
|
ask it pt has passed flatus within the past 8 hrs or a stool within the past 12-24 hrs.
|
|
|
|
blumbergs sign
|
rebound tenderness..pain felt on release.
|
|
|
|
Stool Tests
|
FOBT: avoid raw fruits and veggies and red meat Vitamin C rich foods juices and tablets, coumadin and NSAIDs DC 7days before.
ova and parasites test: tested for parasitic infec and steatorrhea. C.Diff: stool cyctocix assay and stool |
|
|
|
Diagnostic Upper GI studies
|
fluoroscopy exam: trace the barium through the esophagus and stomach pt stands against xray table then table changes position to coat the mucosa supply pillow or blanket for warmth...if small bowel radiographic series is included the patient drinks additional barium and more xrays r taken...chalky white for 24-72hrs.
NPO overnight. post procedure: may need laxative, drink 6-8 glasses water for 2 days. monitor stools. |
|
|
|
Barium Enema lower GI study
|
fluoroscopic and radiographic exam of large intestine after barium instilled rectally.
prep: laxatives clear liquid diet snd enema. post: increase fluids 24-48hrs. mild laxative to pass barium, monitor for stool barium notify MD if no BM in 2 days. |
|
|
|
PTC
|
xray of the biliary duct system using an iodinated dye instilled via a percutaneous needle inserted through the liver.
ERCP is better for information about dilated biliary ducts. |
|
|
|
MRCP
|
patients with abdominal symptoms usually first test requested by HCP.
|
|
|
|
Endocopic Exams
EGD, ERCP(farther than EGD into duodenum into biliary tract) |
pre: NPO 6-8 hrs before test, obtain informed consent, remove dentures, administer sedative as ordered, obtain baseline vitals. avoid anticoagulants aspirin and NSAID.
intra: fentanyl for seditation, atropine for dry secretions, left side decubitus sims position. post: monitor vs resp caridac and neuro status, gag reflex, s/s of bleeding: hypotension, pallor, tachycardia. s/s of perforation: pain tachypnea crackles. |
direct visualization of GI with flexible endoscope through the esophagus stomach and duodenum.
DO NOT GIVE ANYTHING BY MOUTH UNTIL GAG REFLEX IS INTACT. |
|
|
Endocopic Exam: Colonoscopy
|
endoscopy to visualize lining of large intestine.
pre: obtain informed consent, clear liquid diet 48 hrs before, NPO 6-8h before, bowel prep laxatives evening before enema day of test. post: monitor vs, monitor for side effects, resume normal activity n diet, monitor s/s of colon perforation: abdominal pain or distention malaise fever purulent rectal drainage or lower gi bleeding. |
|
|
|
Lower Endocopic Exam: Sigmoidoscopy
|
exam of rectum n sigmoid using flexible scope. test for cancer colon, GI bleeding n IBD.
pre: clear liquids 24b4 cleansing enema morning of. post: mild gas pain n flatulence from air instilled. |
|
|
|
stomatitis:
primary: aphthous, herpes. secondary: infection, fungi, candidiasis, chemotherapy. |
Clinical Manifestation: dry red painful mouth, oral ulceration,
if candidiasis possibility from dentures: white plaque-like leasions on the tongue when wiped away, red sore tissue appears. oral hygiene: soft toothbrushor disposable foam swabs, rinse mouth with alcohol free mouthwash, perform after each meal and at bedtime. drug therapy: antibiotics(swish and swallow) antifungal(swish n swallow) IV acyclovir for herpes simplex stomatitis symptomatic topical agents. |
risks for aphthous ulcers: coffee, potatoes, cheese, nuts, citrus fruits, gluten, deficiency in B vitamins, folate zinc iron.
|
|
|
Leukoplakia
|
thickened white firmly attached patches, slightly raised and sharply circumscribed, oral hairy leukoplakia found in HIV patients.
|
smokers patch. risk: smoked dipped chewed tobacco male older than 40.
|
|
|
oral malignant tumors
|
squamous cell carcinoma: most common oral malignancy, risk fx are age tobacco and alcohol use, tumor node metastasis TNM.
Basal cell carcinoma: occurs primarily on lip, asymptomatic resembles raised scab, aggressively involves the skin of the face but does not metastasize, risks are exposure to sun. kaposi sarcoma: usually painless raised purple nodule or plaque, found on the hard palate gums tongue or tonsils, most often associated with AIDS |
|
|
|
Oral Cancer
|
bleeding from mouth, poor appetite, difficulty chewing and swallowing, poor nutrition with weight loss, thick or absent saliva, painless oral lesion that is red raised or eroded, thickening or lump in cheek.
Dx: biopsy of lesion MRI or CT to see spread. Nursing dx: risk for ineffective airway clearance, impaired oral mucous membranes, impaired verbal communication, disturbed body image, acute pain. |
|
|
|
oral cancer
|
risk for ineffective airway clearance: nonsurgical management: HOB elevated, encourage coughint or suction, teach coughing techniques, monitor resp status and breath sounds, administer humidified 02 administer meds; steroids, antibiotics, aspiration precautions; monitor swallow cough and gag reflex, administer liquid meds or crush, thickened liquids
surgial management: tracheostomy if extensive surgery or edema in which they will lose speech temo NPO until sutures r healed. decannulation possible after postop edema resolves trach may be permanent for some pts. give oral care every 4hrs. |
|
|
|
oral cancer
|
impaired oral mucous membrane: nonsurgical management: oral care q2-4 hrs, soft toothbrush, lip lube, avoid commercial mouthwash and lemon glycerin swabs, rinse with sodium bicarb solution or warm saline, radiation: external beam or implantation, chemotherapy: adjunct to surgery or radiation.
surgical manage pre op: small excision: informed consent and teaching, larger surgery: teaching temp trach loss of speach, NPO IV in place, post op pain mgmt. activity out of bed next day, surgical drains. surgical mgmt post op: maintain airway patency, gental oral care as ordered tske care of suture line, relieving pain, promoting nutrition. homecare: follow treatment plan, taste sensation may be lost, thickened liquids fkr dysphagia, soft foods for stomatitis, inspect mouth qday, use chemo brush and frequent rinsing, saliva substitute for xerostomia dry mouth, avoid sun, clean with gentle non deodorant soap. |
|
|
|
acute sialadenitis
|
inflammation of salivary gland leading to decreaae in saliva production. producing fever general malaise
administer IV fluids for hydration, warm compresses, massage, saliva sub and use of sualagogues include lemon slices and fruit flavored candy. |
|
|
|
salivary gland tumors
|
slow growing painless mass involving facial nerve to wrinkle brow, raise eyebrows, squeeze eyes shut, wrinkle nose, pucker lips, puff out cheeks, grimace or smile.
surgical excision. |
|
|
|
what might u notice in a patient with inadequate digestion and oxygenation as a resukt of oral cavity problems
|
dysphagia
dyspnea stridor or wheeze changes in speech or voice copious thickened oral secretions excessive coughing during meals. assess: breath sounds, oxygen sat, ability to cough n clear airway, ability to manage excessive oral secretions, and ability to chew n swallow respond by: place HOB elevated, apply ox as needed, suction oral cavity as needed, encourage deep breathing and coughing every 2 hrs, increase fluids to liquefy secreations depending on swallowing ability, notify resp therapist or RRT if interventions arnt successful |
|
|
|
GERD
|
gastic secretions(pH 1.5-2) flow upward into esophagus(pH 6-7) due to weakening of LES.
4factors: inappropriate relaxation of LES, irritation, delayed gastic emptying, abnormal esophageal clearance. causes: obesity pregnancy hiatal hernia med fatty foods caffiene alcohol smoking NG tube more than 4 days after pyloric surgery tomatoe products, anticholinergic drugs. symptoms: belching, flatus, dysphagia from esophageal stricture, esphagitis from inflammation, epigastic pain, heartburn(dyspepsia), feeling of fluid accumulation in throat(globus), chronic cough, laryngitis n morning hoarsness, wheezing N/V, water brash, odynophagia (painful swallowing) Dx assessment: 24hr ambulatory pH monitoring keeping a diary, EGD, esophageal manometry nursing dx: acute or chronic pain, risk for aspiration, impaired swallowing. nursing care: avoid foods that cause problems like caffeine fatty spicy foods milk products alcohol licorice and encourage 4-6 small meals avoid eating snacks or 2-3h before bed sleep with head elevated increase fluid intake. sleep in the right side laying position. medical mgmt: antacids maalox or mylanta 1 hr before and 2 hrs after meals, H2 receptors like pepcid zantac n axid decrease acid, PPIs like prilosec protonix nexium are for more severe gerd, stool softners weight loss surgery if necessary(stretta procedure)(LNF) |
|
|
|
antacids
|
mylanta and maalox
increase pH of gastic contents give 1 hr before and 2 hrs after meals and bedtime. work best on empty stomach. watch for constipation |
|
|
|
H2s
|
zantac, pepcid, axid
decrease gastic secreations by blocking histamine receptors in parietal cells. admin at bedtime, observe for dysrythmias, do not mix with tomatoe based mixed vegetable juices only with apple juice. |
|
|
|
PPIs
|
prilosec, prevacid, protonix, aciphex, nexium.
decreases gastric acid long acting. take before meals if difficulty swallowing open capsule and mix with apple juice do not crush break or chew do not give IV with other drugs. |
|
|
|
Hiatal Hernia
|
sliding hernia is most common, esophagogastric Junction and portion of fundus slide upward into the thorax. see asthma sx at night.
rolling hernia fundus rolls into the thorax beside the esophagus. anemia is common with these. assessment: heartburn, regurgitation, pain, dysphagia, belching(eructation), worsening after eating or when in recumbent postition. mgmt: same as GERD, H2 zantac avoid eating late and foods associated with reflux. remain upright several hours after eating. aviod vigorous activities, refrain from tight clothing. LNF same as GERD so teach about chest tubes n NG tube for several days oral intake started gradually, deep breathing is very painful so give analgesics. watch for bleeding and infextion. nutritional care for complications of surgery include gas bloating syndrome pt has difficulty belching to relieve distention and aerophagia air swallowing from attempting to reverse or clear acid reflux teaxh them to relax before meals and eat and drink slowly frequent ambulation or give simethicone crushed and dissolved in water. stool softeners. |
|
|
|
achalasia
|
esophageal motility disorder LES cannot relax
s/s: dysphagia regurgitation of food substernal chest pain loss of weight halitosis treatment: medications like anticholinergic, nitrates, and calcium channel blockers, diet and position changes, dilation of LES surgery esophatomyotomy nursing care: post op care dilation monitor for bleeding and signs of perforation NPO for 1h post op liquids for 24hrs. postop for esophagomyotomy chest tubes drains enteral feedings monitor for infection n healing. |
|
|
|
esophageal tumors
|
causes: tobacco alcohol barretts esophagus diet and genetics.
s/s: dysphagia odynophagia wt loss, regurgitation, vomiting, foul breath, chronic hiccups, pulmonary complications, chronic cough, hoarseness. silent tumor in early stages. assessment: psychosocial anxiety n fear diagnostic: barium swallow tissue biopsy via EGD CT or PET scans. nursing dx: imbalanced nutrition less than, risk for aspiration, impaired swallowing, acutr or chronic pain, ineffective coping, anticipatory grieving, spiritual distress. imbalanced nutrition less than body requirements nonsurgical interventions include. nutritional therapy, swallowing therapy, chemotherapy, radiation, photodynamic therapy, esophageal dilation, endoscopic therapies, surgical removal of the tumor. surgical magmt: esophagectomy removal of part of the esophagus or esophagogastromy removal of paet of esophagus and proximal stomach. post op care: highest is resp care intubation and mech ventilation for first 16-24 hrs, cardiovascular care, wt mgmt, NG mgmt, nutrional care, discharge planning, direct wound support during changing and repositioning. do not irrigate or reposition the NG tube of a pt post op of esophageal surgery unless requested by surgeon. 6-8 small meals a day and fluids between meals. |
|
|
|
ng care
|
|
|
|
Gastritis
|
inflammation of the stomach lining. mucosal barrier of stomach is broken allows HCL acid and pepsin to damage. can cause pernicious anemia.
chronic gastritis type A: non erosive: inflamed glands fundus and stomach body. type B: inflammed antrum glands entire stomach. Atrophic: deep glands all layers of stomach stomach muscles atrophy can lead to PUD. causes: H.pylori, impaired immune system, meds like NSAIDs ASA corticosteroids, chronic alcohol, caffeine, smoking, allergrns, toxic chemicals s/s: epigastic pain, indigestion, cramping, anorexia, N/V, hematemesis, anemia, intolerance to fatty spicy foods. flareups. dx with EGD. medical mgmt: meds antacids like maalox, H2 n PPIs sucralfate, bismuths, antibiotics. vitamin b12 supplements avoid aggravating foods. nursing care: encourage smoking cessation, decrease eliminate alcohol stress reduction, teach pt about medications. |
|
|
|
peptic ulcer disease
|
erosion of wall of esophagus, stomach or duodenum. erosion can extend through thr muscle to the peritoneum. 2 types are gastric which are deep and penetrating and duodenal which are high acid secretion. stress ulcers mulitple shallow erosions.
ulcer complications: hemorrhage: if an ulcer erodes through a blood vessel it is a life threatening hemorrhage. Perforation: if ulcer erodes through thr mucosal wall patient will develop peritonitis. pyloric obstruction: the pylorus becomes scarred has edema and inflammation. causes: erosions caused by exposure to irritants meds, smoking, alcohol, food allergens, H.pylori. family history. gastric: gnawing sharp pain 30min-2h after eating eating makes it worse weight loss and anorexia nausea pallor epigastic tenderness hyperactive bowel sounds. duodenal: pain gnawing and dull 2-4h after eating similar to hunger pains eating relieves pain weight gain is common pallor epigastic tenderness hyperactive bowel sounds. nursing dx: acute or chronic pain. deficient knowledge. imbalanced nutrition less than. disturbed sleep pattern, nausea, fatigue, risk for falls. drug therapy: provide pain relief eradicate H.pylori infection, heal ulcerations prevent recurrence, give antisecretory drugs(PPI) and H2 and prostaglandin analogues like cytotec. diet therapy: bland non irritating diet during acute symptomatic phase avoid bedtime snacks alcohol and tobacco. hypovolemia mgmt: monitor vs InOs HnH lytes, admin IV fluid NS or LR as ordered, if active bleeding give fresh frozen plasma watch for falls. ulcer bleeding mgmt: monitor NG placement to empty stomach, room temp NS lavage vie NG tube for vasoconstriction, h2 blockers ppis antacids n vasoconstriction or cautery via EGD. nonsurgical mgmt: perforation: immediately replace fluids blood and lytes administer antibiotics keep NPO. pyloric obstruction: NPO insert NG tube correct metabolic alkalosis and dehydration. surgical mgm: MIS: csn remove chronic ulcers and treat bleeding. Vagotomy: eliminates acid secreting stimulus to gastric cells and decreases response of parietal cells. pylorplasty: facilitates emptying of stomach contents. |

|
|
|
tube placement
|
|
|
|
|
gastric cancer
|
most commonly adenocarcinoma primarily in the pyloric area.
risks: H.pylori, hystory of polyps, pernicious anemia, achlorhydria absence of HCL acid, gastrectomy, diet, genetics s/s: vague epigastic discomfort or indegestion, postpradinal fullness, ulcer like pain that doesnt respond to therapy, anorexia, weakness, blood in stools hematemesis, vomiting after fluids or meals. treatment: surgery partial or total gastric resection, chemotherapy and or radiation. EGD with biopsy. nursing care: preop NG tube before surgery TPN after. watch for dumping syndrome which is rapid emptying of food contents into small intestine which shifts fluid to gut causing abd distention 30 min after meal desire to lie down pallor. late is caused by excessive insulin release. give high fat and protein diet. low carbs no milk or sugars. nutrional mgmt: deficiencies in b12 folic acid and iron imparied calcium metabolism reduced absorption of calcium and vitamin D. lie flat after eating. |
|
|
|
IBS/spastic colon/nervous colon
|
appear in young adult hood and continue. combo of environmental immunologic genetic hormonal and stess all can play a factor. more in woman. may lead to secondary depression.
most common concern is pain in LLQ. nausea associatef with meal time and defecation, constipated stools are small n hard followed by watery stools with mucus. belching gas anorexia and bloating. test: hydrogen breath test. NPO for 12hb4 test. n q15min for hout. interventions: dietary fiber to est reg bowel habits regular meals n drink 8-10 cuos of liquid a day. drugs like toviaz for overactive bladders may help. probiotics IBS-C: psyllium bulk forming lax, metamucil. amitiza not for men tske with food n water. IBS-D: antidiarrheals imodium psyllium alosetron. |
|
|
|
herniation
|
portion of intestines protrudes through a weakened area of the abdominal wall
types: indirect or direct inguinal more in males. direct inguinal hernias: pass through a weak point in the abdominal wall femoral hernias: fat pulls even thr bladder into thr sac umbilical hernias: congenital in infancy...aquired is in obese people.. nonsurgical mgmt: may be pushed back in or reduced by MD called reducible. abdominal binder or truss most often for men is a pad made wuth firm material held over thr hernia with a belt may be used. irreducible cant be pushed back and requires immediate surgery. surgical: MIIHR also called a herniorrhaphy remain NPO before surgery. hernioplasty is a mesh patch to reinforce the weakened muscle. avoid coughing. may experience difficult voiding and bladder emptying may need straight cath. |
|
|
|
colorectal cancer
|
involves epithelial and surrounfing tissue of the colon and rectum
risks: hx of inflammatory bowel disease, polyps, age older than 50 and family hx, high fat diet and red meat. s/s: change in bowel habits, hematochezia, rectal bleeding, abdominal pain, distention, ascites, nausea, cachexia. most common is chronic blood loss and anemia. no gross blood from tumor on right side but with tumors on left side of colon and rectum. FOBT is not reliable. lab tests: H&H values usually decreased, elevation of CEA, double contrast barium enema, CT scan, flexible sigmoidoscopy, colonoscopy. 1:invades up to muscle layer, 2: invades other organs, 3:any level of tumor invasion n upto 4 lymphs, 4: many lymphs and distant mets. nursing dx: anticipatory grieving, distrubed body image, fear, powerlessness, impaired nutrition, acutr or chronic pain. treatment: radiation, chemo 5fu leucovorin eloxatin, avastin. surgery (colon resection, colectomy with colostomy temp or perm or ileostomy, AP when rectal tumors are present. preop: consult with et nurse, bowel prep golytely, NG tube. postop: colostomy should be reddish pink n moist snd protrude about 3/4 inch from abd wall. should not be dark, purple or dry or firm. empty whrn its 1third full. absorbent dressing over wound, avoid sitting long n stool softener. cut 1/8 to 1/16 inch larger than stomal pattern on wafer portion. clean wjth mild soap n water dont use moisture soaps. apply skin sealant. and wound care mgmt, NG tube. make refurals to an ostemate. or social worker. |
|
|
|
intestinal obstruction
|
mechanical obstruction coliky crampy pain that comes and goes and nonmechanical (paralytic ileus) commonly caused by handling the intestine during surgery.
causes: tumors hernias fecal impac strictures from crohns, intussusception vovulus fibrosis adhesions. obstruction high is met alk obstruction low is met acid. s/s: constant diffuse discomfort abdominal distention decrease or absent bowel sounds or borborygmi vomiting obstipation no passing of stool and hiccups diarrhea in partial obs. test: endoscopy, barium enema, CT. wbc increased in strangulation. hemo hemacrit and bun are elevated to say dehydration. loss of serum sodium chloride and potassium. ABG tell met acidosis or alk. nonsurgical management: NPO with salem sump pump on low contin suction with a vent or pigtail.assess for placement q4h. if placement is est aspirate contents and irrigate with 30mL of saline every 4hrs. fluid and lytes, pain mgmt, drug therapy broad spectrum IV antibiotics. semi fowlers. surgical: exploratory lap. preop: teaching snd NG tube with suction if time permits. postop: monitor NG tube and normal care. clear liquid diet and ng capped if pt vomits suvtion is put back on. opiods with stool softner. |

|
|
|
abdominal trauma
|
mostly caused by MVA. spleen is most common organ for blunt trauma but liver is for penetrating trauma like gun shot.
assess: ABC then focus on risk for hemorrhage shock and peritonitis mental status vital signs n skin perfusion are priority cause mild shock is pale cool and moist, moderate is diaphoresis n deceased urine. severe shock changes in loc by agitation disoriention and memory loss. absent or diminished bowel sounds could indicate blood bacteria or chemical irritant in cavity. ascultate for bruits in abdomen which could indicate renal artery injury. RL rib injury for liver and LL rib injury for spleen. dullness. tests: DPL and FAST. ABG, CBC if elevated wbc indicates ruptured spleen or intestinal injury, BUN, lytes, liver function tests, coagulation study. nursing care: 2 large IVs in upper extremities. type and crossmatch blood 4-8units. insert foley. NG tube. monitor vitals q15min. report changes immediately. watch IAP norm is 0-5. |
|
|
|
IAP
|
norm is 0-5 if over 20 acidosis and ischemia occur. if untreated damage to intestines increases risk for sepsis multiple organ dysfunction MODS and death.
report any increase immediately or a sustained or repeated level of 12 or higher is considered IAH or ACS. give vassopressor drugs n fluids. |
|
|
|
Polyps
|
villous adenomas are greater cancer risk. family hx of FAP or HNPCC. 40-50yrs.
pedunculated polyps r stalk like. sessile polyps r broadbased n flatter. s/s: asymptomatic, gross rectual bleeding, intestinal obstruction treat: polypectomy or colectomy remvoal of colon if family history. |
|
|
|
hemorrhoids
|
swollen or distended veins.
internal: cannot be seen external: can be seen n can prolapse which can bleed. risks: straining obesity HF, prolonged sitting or standing, weight lifting. s/s: bleeding swelling bright red blood itching n mucus. treat: fiber; whole grains, veggies, fruits, liquids maintain healthy weight. cold packs sitz baths use cleasing towelts instead of toilet paper. surgery and give high fiber and fluids but no laxatives. first bowel movement is painful give colace which is a stool softener. |
|
|
|
malabsorption symdrome
|
s/s: chronic diarrhea unabsorbed nutrients n steatorrhea because deficiency of bile salts. b12 deficiency. weight loss, bloating farting bruising anemia bone pain, edema cause by hypoproteininemia
test: schrilling test measures urine b12 for dg of pernicious anemia. bile acid breath test for bile salt. interventions: diet, water vitamins like folic acid and b complex fat vitamins like ADEK, minerals like calcium iron and mag, pancreatic enzyms like pancrelipase. antidiarrheals, antibiotics, |
|
|
|
appendicitis
|
RLQ pain. can lead to peritonitis.
abd pain cramplike in epigastic area anorexia nv mcburneys point where pain increases with cough or movement and relieved by bending the right hip or the knees which suggests peritonitis. rebound tenderness. wbc with shift to left meaning newwbcs. nonsugrical: NPO, IV fluids to replace lyte imbalance. semi fowlers DO NOT GIVE LAXATIVES OR ENEMAS OR HEAT. surgical: appendectomy eithet by lap...NOTES... or by open. get out of bed evening of. if peritonitis NG tube is placed. pain mgmt. |
|
|
|
peritonitis
|
acute inflammation of peritoneum
primary: vascular system seconday: from abd disorder normal p.cavity contains 50mL which prevents friction during peristalsis. if infection it walls off...if walling off fails widespread peritonitis occurs. hyperemia occurs and fluid is shifted into third spacing causing hypovooemic shock n kidney failure peristalsis stops leading to septicemia and resp problems from pressure on diaphragm. s/s: ridgid board abdm. abd pain, distended abd nv anorexia diminished bowel sounds no flatus rebound tenderness fever tachycardia dehydration hiccups... generalized the pain is wide spread. nonsurgical mgmt: IV fluids, broad antibiotics, weight, I and o, NG tubr, NPO, oxygen n pain control. surgical: laparotomy monitor loc and I and o abd vitals for hr after...semi fowlers. removes chemical irritant and repair cause of fecal impaction. irrigation if drainage is manual use sterile techniques. nursing interventions: bedrest semi fowlers monitor I n o daily weight abd girth encourage TCDB leg exercises oral hygiene wound care. |
|
|
|
gastroenteritis
|
rotavirus or norwalk virus fecal oral route
travelers diarrhea ir shigellosis dysentery nv myalgia headache malaise dehydration drink fluid replace sodium and potassium 0.45 sodchl IV n potassium IV. dont give things to prevent bacteria from leaving body. ..only antibiotics stool sample for cause. sitz baths panty liners |
|
|
|
Ulcerative Colitis
|
tiny abscesses form which produce purluent drainage sloughs the mucosa and ulcerations occur. results in loose stools containing blood mucus poor absorption of nutrients and thickening of colon wall.
s/s: diarrhea of pus and blood 15-20 stools a day. abd cramping and pain. involuntary loss of stool. psychosocial effects. remissions and exacerbations. narrow colon. tenesmus. can be mild moderate severe with anemia tachycardia fever or fulminant more than 10stools a day may need transfusion. 30-40yrs of age and again at 55-65. complications are fistulas cancer and osteoporosis. tests: wbc ESR is consistant. low sodium and pot n chloride. barium enema and colonoscopy. diarrhea interventions: record color volume frequency and consistency. id factors that cause or contribute. eliminate gas producing foods spicy and lactose foods. low fiber diet. monitor skin. weight daily. rest the bowel so NPO n TPN. ensure easy access to bathroom. drugs: aminisalicylate compounds 5 ASA called sulfasalazine. glucocorticoids like prednisolone...immunomodulators humira combined with steroids. antidiarrheals. surgical mgm: restorative proctocolectomy w ileo pouch anal anastomosis. through the anus. RPC IPAA 2stages to help bowel temporary ileo and then removed.. or total proctocole with permanent ileostomy. ileo is usually placed in RLQ shouldnt prolapse or retract n b pinkish to cherry red. wait for ileostomy adaptation wear a pouch at all times. skin care is a priority. treat RPC IPAA with flagyl if inflammation. assess for blood in stools melena monitor hnh n lytes vs prepare for pos transfusion. observe for megacolon which is fever tachycardia distended abdomen. avoid crowds n infections n gassy n thicker poop foods like nuts cabbage corn celery apples wuth peels n popcorn. |
|
|
|
difference in crohns and UC
|

|
|
|
|
illeostomy care
|
use skin barrier
use skin care products like sealants and ostomy creams watch for redness. emptu pouch when 1/3 full chsnge pouch during inactive times like before meals n night or when waking change entire pouch system q3-7 days. chew food thoroughly avoid high fiber high cellulose foods like corn peanuts coconut chinese veggies string beans meats shrimp lobster rice bran and veggies with skins like tomatoes corn n peas. avoid enteric coated medications. contact hcp if no stool in 6-12hrs. if stomal swelling abd cramping or distention occurs remove pouch with faceplate lie down fetal position begin abd massage apply moist towels drink hot tea. |
|
|
|
crohns disease CD
|
idopathic inflammatory disease all layers of bowel involved bowel fistulas malabsorption of vitamin n nutrients leads to fibrosis scarring n thickening of walls.
manifestations: 5-6 soft loose stools not bloody. steatorrhea. RLQ pain before and after bowel movements. anemia low b12. Dx: Colonoscopy UGI n CT. drug therapy: 5AS, MTX to suppress immune system. humira headache nv are common se. nutrition therapy: TPN or elemental diet. during remission a low residual diet. high cal/protein/vitamin low fiber diet. make sure wounf drainage isnt contacting skin cause its caustic. use skin barriers and ostomy pouches to protect. antibiotics. surgery: segmental resection of diseased bowel stricturoplasty. community based care: monthly vitamin b injections diet and med teaching fistula mgmt. |
|
|
|
diverticular disease
|
diverticulosis pouch like herniations through the muscular layer of colon
diverticulitis inflammation of one ir more diverticula. clinical Manifestation: diverticulitis: mild to severe pain left lower quad. elevated wbc low grade fever abdominal distention nv blood in stool. men more affected n older than 60. test with barium enema after given antibiotics. nonsurgical mgmt: broad spec antibiotics like flagyl antifungal and analgesics for pain. in severe: IV fluids antibiotics antifungals anticholinergics n IV opiods bedrest clear liquids or NPO with NG tube. if active providr low fiber when inflam resolves give high fiber. surgical: colon resection colostomy temporary or permanent. avoid foods with seeds. |
|
|
|
anal disorders
|
abscess: induration n pus mgmt with InD n antibiotics. sitz baths n stool softners.
fissure: tear in anal lining. can be painful. if acute usally resolves on own if chronic surgical tx may be needed. pruritus dyuria n dyspareunia. colonoscopy. give metamucil bulk forming agent. n hydrocortisone cream fistula: abdnormal tract leading from anal canal to the perianal skin. pruritus purulent discharge tendernesd pain with bowel movemts. do proctoscopy and surgery fistulotomy. sitz baths analgesics and bulk forming metamucil. |
|
|
|
common types of food poisoning
|

|
|
|
|
cirrohsis
|
hardening irreversible scarring
slow deveolping common causes are hep c alcoholism liver enlarges and biliary obstruction. hep b and d worldwide also. s/s early: few fatigue weakness exhaustion loa nasuea weight loss. later: yellow of skin from jaundice rashes petechiae spider angiomas ascites brusing because its not clotting, bleeding infection becsuse its not filtering and ur body is open to infextion, jaundice because liver isnt processing rbc which leads to anemia. big time bruising with alcoholics. hyperglycemia because liver isnt metabolizing glucose so glucose is free flowing in ur body. ascites is aldosterone keep sodium and water and gets rid of potassium impaired breathing snd reduced urination. bad breath gynecomastia. hepatic artery oxygenated blood.. portal vein: brings nutrient rich blood in from GI with hardening its going to start backing up leading to portal hypertension and splenomegaly n thrombocytopenia. hepatic duct: transports bile into gallbladder factors are: alcoholism leads to defic in thiamin mag multi vitamins malnut from vit b virus like hep n toxicity.. hepatic encephalopathy: ammonia cauding cns problems from high protein diet leading to ammonia smell on breath trouble concentrating fruity breath tremor lactulose drink that binds to ammonia snd excreted through stool. eat high protein foods n high carbs to get rid of ammonia since it binfs to protein ir cirrohsis but with encephalopathy u get mod protein and simple carbs. no sedatives. check for asterixis n fector hepaticus. esophageal varices: bleeding when portal vein cant bring blood into hardened liver dark stools red if active bleeding tortured ropy thin walled can cause death. to orevent bleeding use beta blockers like propranolol. antibiotics. iV teripressin watch heart. use EVL with banding or sclerotherapy balloon tamponade with intubation. nursing interventions: promote resr ambulation periods leg elevated high cal mod protein diet assess skin wounds admin antiitch meds no soap use lotions for dry skin. daily weights. low sodium diet. lots of vitamins. labs: AST n ALT bilirubin serum proteins ammonia PT prolonged. CT MRI US. biopsy. EGD, ERCP. treat: paracentesis void before. resp support so ascultate lungs often. elevate hob 30degrees elevate legs weight apply oxygen TIPS. potassium supplement. avoid alcohol n tobacco. |
|
|
|
jaundice
|
hepatocellular is because liver cant effectively excrete bili leads to excessive circulation of bili levels.
obstructive: from edema fibrosis or scarring of the hepatic bile channels snd ducts. |
|
|
|
hepatitis A
|
rna virus
transmitted fecal oral route fecal contaminated food or drinking water. flulike symptoms. not life threatening leaves body. |
|
|
|
hep b
|
dna virus
unprotected sex with infected partner. sharing needles. needle sticks. blood transfusion. hemodialydis. maternal fetal route. open cuts n sores. IV. may become immune and clear virus or become a carrier. |
|
|
|
Hep C
|
rna virus
transmitted percutaneously iv drug use blood transfusion unsan tattoo, sharing needles. dont share razors toothbrushes or earrings. chronically infected forever doesn't leave. leading to cirrrosis major factor. |
|
|
|
Hep D
|
delta virus
cannont survive on own requires HBV to replicate sex and iv drug users. |
|
|
|
Hep E
|
waterborne epidemics
fecal oral route mostly in other countries...travelers. resolves on its own. |
|
|
|
Hepatitis
|
fulminant often fatal
chronic as with b or c. cirrohsis hepatocellular carcinoma signs: hepatomegaly splenomegaly palpable liver symptoms: flulike tests: liver function tests. antibodies, hep c use elisa nursing dx: fatigue nausea imbalanced nutrition activitu intolerancr care: rest diet high carb n cal mod fat n protein small meals. meds antiemrtjcs vitamins fluids. no alcohol. chronic HBV a interferon administer subq se are hairloss flu symptoms muscle weakness n aching chronic HCV pegylated a interferon with ribavirin se are anemis anorexia cough rash insomnia. teach: strict and frequent hygiene dont share bathrooms individual bathroom utebsils. dont prepare food for family dont donate blood avoid alcohol use condom or abstain carry med alert bracelet |
|
|
|
signs of hemorrhage n shock
|

|
|
|
|
liver cancer
|
primarily hepatocellular
no early symptoms late is wt losd anorexia weakness jaundice bleeding surgery early transplant if late do hepatic artery embolism and chemo organ transplant for the perfect patient antibiotics for surgery. immunosuppressive drugs forever |

|
|
|
cholecystitis
|
inflammation of gallbladder
acute: calculous or acalculous. calculous results with cholelithiasis which are gallstones that obstruct the cystic duct or common bile duct called choledocholithiasis. gallstones are usually bile cholesterol bili bile salts calcium n proteins. cholesterol stones form from metabolic imbalances or cholesterol and bile salts. pigmented stones are associated with cirrhosis of liver. acalculous is associated with kinking ot twisting resulting in a decreased flow most causes are sepsis trauma burns TPN multisystem organ faikure major surgery or hypovolemia. chronic cholecystitis calculi are always present and results in repeated episodes of cytic duct obstruction. s/s: jaundice, Icterus (eye yellowing). causes obstructuve jaundice or intrahepatic jaundice. pruritus. vague upper abdominal pain that radiates to right shoulder anorexia nv dyspepsia eructiation flatus fullness blumbergs sign fever clay colored stools or steatorrhea. often referred to as gallbladder attacks. risk factors for cholecystitis: women aging obesity rapid weight loss or fasting increased cholesterol HRT family hx TPN crohns DM pregnancy genetics. 4Fs femal forty fat fertile. labs: wbc count indicate inflammation. AST and LDH elevated indicating abnormal liver function. view stones by xray. or US of right upoer quad. ERCP or MRCP. nonsurgical tx: opiod analgesics dilaudid. antiemetics ESWL: patient lies on water filled pad and shock waves break up stones. or use internal/external drains. surgical: cholecystectomy removal of gallbladder. lap chole is gold standard. give iv antibiotics. carbon dioxide to inflate cavity. early ambulation to get that carbon out keep hob elevated. TCDB. if T-tubr is used dont lift system above site if insertion to prevent backup of bile. low fat diet. |
|
|
|
gallbladder cancer
|
women than men and rare.
signs are anorexia wt loss nv abd bloating fever malaise jaundice enlarged spleen n liver test: CT MRCP CEA n CA19-9. intervention: pronosis is poor. surgery is either potentially curative or palliative. do simple cholecystectomy. extended romoved gall lymphs and small psrt of liver. |
|
|
|
acute pancreatitis
|
serious inflammation process that is caused by premature activation of excessive pancreatic enzymes that destroy ductal tissue and pancreatic cells resulting in auto digestion and fibrosis. NHP is diffusely bleeding pancreas tissue with fibrosis n tissue death.
4 major processes occur: lipolysis causeing hypocalcemia, proteolysis leading to gangrene, necrosis of blood vessels caused by elastase n trypsin. and inflammation when leukocytes cluster n a pseudocyst can form. complications: jaundice, type 1 DM, left lung pleural effusions pneumonia, ARDS, shock causes: trauma external obstruction metabolic disturbances like hyoerlipidemia hypercalcemia renal disturbances familial ulcers alcoholism toxic drugs. pancreatic attacks during holidays when heavy alcohol drinking. signs severe abdominal pain in mid epigastic area or left upper quad. sudden onset and radiates to back left flank or left shoulder. worsened by laying supine and finds relief in the fetal position. wt loss. gray blue discoloration of flanks n perumbilical region. tests: amylase elevated in 12-24 hrs if remained elevated it mesns cyst. lipase takes longer to elevate but stays for 2 weeks. bilirubin and phosphatase sre elevated. decresse in calcium.and mag and albumin. c reactive protein TNF suggests necrosis n inflammation. nonsurgical mgmt. ABCs. abdominal pain with pain control dilaudid n IV isotonic fluids. fasting and rest. ask about passing flatus n last BM. fetal position antibiotics n H2s. NPO. TPN n weighed every day. resp every 8 hrs and provide oxygen as needed. do sphincterotomy to open oddi if cant then go to surgery. after healing small frequent meald mod to high carbs high protein low fat. limit activities to one floor at home no stair climbing. no alcohol. surgical: MIS to drain cyst. |
|
|
|
enzymes of pancreas
|
trypsin: edema necrosis hemorrhage
elastase: necrosis of blood vessels n ductal fibers lesding to hemorrhage phospholipase A: fat necrosis cell membrane disruption lipase: fat necrosis kallikrein: edema shock. |
|
|
|
chronic pancreatitis
|
progressive destructive disease.with remission n exacerbations...mostly caused by alcohol for CCP causing panc to become hard n firm. mostly in men. chronic obstructuve pancreatitis. autoimmune pancreatitis n idiopathic. all cauding steatorrhea stools are pale bulky frothy n smell horrible. protein malabsorption results in starvation edema of the feet legd hands caused by decrease in levels of circulating albumin. DM. chronic lung and breathing problems.
signs: intense burning or gnawing pain adb tendernesd ascites left upprr quad mass resp compromise seen by dimished breath sounds dyspnea or orthopnea, steatorrhea wt loss jaundice dark urine polyuria polydipsia polyphagia tests: ERCP CT MRI US nursing: mang pain assist with nutritional intake n prevent recurrence. nonsurgical: analgesia for pain. PERT to prevent malnutrition. creon should not be crushed or chewed n take with meals or snacks n water. after h2s. wipe lips after. if capsule n cannot swallow pierce it and mix it dont crush it. do finger stick blood glucose levels FSBG q2-4hrs. give TEN or TPN. surgical: drains cyst. lap chole. sphincterotomy. limit activities to one floor at home no stair climbing. |
|
|
|
pancreatic cancer
|
adenocarcinoma grow rapidly abd spread to stomach galldbladder duodenum n intestine.
head of liver most common site. may cause jaundice. cancers of body n tail spread more extensively. complications: venous thromboembolism. usually 60-80. DM. chronic pancreatitis. cirrhosis. high intake of red meat like bacon. long term exposure to chemicals. obesity. signs: jaunide chsnges in stool color n icterus. fixed mass in LUQ fatigue. vague constsnt dullness n referred back pain by pressure on nerve plexus.leg or calf swelling. nv. splenomegaly. GI bleeding. ascities. weakness. clay colored stools. wt loss. tests: elevated CEA CA 19-9. CT. ERCP to place a PTB drain which drains bile. nonsurgical: palliative pain mgmt n tumor spread. chemotherapy or radiation 5 fu. kinase inhibitors. opiods. external beam radiation to shrink tumor. implantation of radioactive iodinr 125 seeds. biliary stents. surgical: MIS partial pancreatectomy for tumors smaller than 3cm. large tumors use whipples(panpancreatectomy) or radical pancreatectomy. preop: jejunostomy for feeding. TPN to provide nutrition. PICC line. iV care. NPO 6-8 hrs before. check glucose often watch for hemorrhage with monitoring pulse bp skin color n mental status. wound infextion. bowrl obstruction. postop: NPO NG tubr to suppress stomach make sure tubes arnt kinked and are draining properly. drainage should be serosanguineous. most disruptions of site happen 7-10 days later. semi fowlers. watch for peritonitis from a fistula formation. decrease vascular pressure with a swanganz cath. insulin as needed. |
|
|
|
vegitarians
|
lactovegetarian eats milk cheese and dairy but avoids meats.
lactoovovegitarian includes eggs the vegan only eats plant foods and maybe fish. vegans can develop anemia from b12 deficiency. so teach to eat fortified cereals soy or meat substitute. |
|
|
|
nutritional screening
|
height
weight both are for baselines. weight history eating habits ability to chew n swallow changws in appetite if patient cant stand use a zliding blade knee height caliper. |
|
|
|
changes is body weight formulas
|

|
|
|
|
BMI formula
|

|
|
|
|
malnutrition
|
PEM: either by Marasmus fat n protein wasted serum proteins preserved. Kwashiorkor is lack of protein with adequate calories. combo of these.
signs: negative nitrogen balance weight loss decreased muscle mass n weakness. hypoproteinemia. cachexia muscle wasting. decreased activity tolerance, lethargy, intolerancr to cold edema dry flaky skin poor wound healing risks: aging, environmental factors n health problems. limited income, poor eyesite. lack of transportation loneliness physical illness failure to thrive drugs pain. assess: chewing n swallowing. dysphagia can cause pneumonia. dentures that dont fit right. labs: hemoglobin for anemia. high hematocrit n albumin for dehydration. PAB. Transferrin. cholesterol n TLC below 1500. nutritional mgm: 6 small meals a day pureed or soft diet for those thst cant chew or have no teeth edentulous. appropriate temps and mouth care before feeding. n pain mgmt before feeding. MNS like ensure. vitamins to prevent anemia. TPN or TEN. |
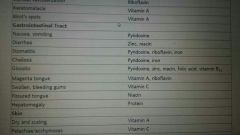
Manifestation of nutritional deficiencies
|
|
|
TEN
|
those who csnt maintain nutrional status alone. those with permanent neuromuscular impairment n cant swallow or those who cannot eat.
methods of delivery id NET nasally like NG tube n smaller bore NDT which are for a shorter term also smaller bores are 8-12franks. enterostomal feeding tubes are gastostomies n jejunostomies...gastrostomy is a stoma created from abd wall to stomach with a short feeding tube called a PEG tube. a jejunostomy is long term feedings wheb its desirable to byoass the stomach. tube feedings are either:. bolus which ie an intermittent feeding of a specified amount of food at set intervals during a 24hr period q4hrs. continuous is small amounts are continuously infused over a specified time cyclic feedings infusion is stopped for s specific time in each 24hr period usually 6 hrs or longer called down timr to allow for activities complications: clogged tubing refeeding syndrome: when nutrition is restarted for a patient in a starvation state. seen by shallow resp weakness acute confusion seizures increased bleeding. tube misplacement or dislodgement abd distention nv fluid snd lyte embalance. tube feeding care n maintenance: if using a NG or NDT use soft flexible small bore tube smaller than 12fr n confirm by xray. if using a gastrostomy or jejunostomy assess sitr for signs of infection or excoriation which is excessive redness n drainage. rotate tubr 360 each day and check in and out play of about 1/4 inch if it cannot be moved notify hcp. cover site with dry sterile dressing and change once a day. check and record residual every 4-6 hours change tubing every 24-48 hrs. irrigation set no more than 24hrs for continuous feedings add only 4hrs of feeding at a time to prevent bacteria. discard unused cans after 24hrs. hob elevated 30degrees n for one hour after for bolus but kept for other feedings. monitor labs. maintaining a patent tube: flush with 20-30mL of water q4hrs during continuous n before n after each intermittent before and after drug administration use warm water n after checking residual. if clogged use 30mL of water to flush with gentle pressure avoid carbonated beverages n no cranberry juice. when aspirating fluid wait at least an hour after drug administration n then flush the tubr to clear it with 20ml of air. pH of gastic id 0-4.0 if tubr has moved into intestine pH will be 7-8 test in lungs with capnometry two most common electrolyte embalances are hyperkalemia n hyponatremia. |
|
|
|
Parenteral nutrition
|
IV therapy to maintain or improve nutrional status.
usually through a cannula or catherter in the large distal vein of arm or through PICC line. TPN is through centrally accessed veins usually through PICC or subclavian or internal jugular veins usually through infusion pump. so monjtor infusion rate and for hyperglycemia lesding to dehydration n shock. potassium and sodium embalances are common with insulin. hypercalcemia prolu from immobile. care for TPN check orders for accuracy monitor rate hourly if unavailable give 10 or 20% D/W until some can be obtained. dont catch up on offtime pump monjtor weight monitor lytes n FSBS q 4hrs. change iv tubing every 24 hrs change dressing on iv every 48-72hrs. have second nurse check before giving TPN. |
|
|
|
obesity
|
overweight is 10% greater BMI 25-29
obesity is 15-20% of body weight greater BMI of 30 or more WC of 35 for women and 40 for men. morbid obesity is BMI greater than 100% and WC greater than 40 complications: type 2DM hypertension hyperlipidemia CAD stroke PAD metabolic syndrome sleep apnea obesity hyperventilation syndrome depression urinary incontinence gallstones gout chronic back pain osteoarthritis decreased wound healing. drugs that cause weight gsin: corticosteroids estrogens NSAID antihypertensive antidepressants antiepileptic and certain oral antidiabetics. assessment: habits, history, family, panniculus observe for candida. any previous attemos to lose weight. what food means to them. behaviors. nonsurgical mgmt: short term fasting or very low calorie diets protein spsring and liquid formula. unbalancrf low carb diet likr Atkins or south beach. 1 pound a week subtract 500 calories a a day. get excersice. drug therapy likr anorectic drugs thst suppress appetite like orlistat se sre palpitationd diarrhea constipation restlessness insomnia dry mouth blurred vision chsnge in sex drive anxiety. behavioral mgmt like a diary log n couseling. surgical: liposuction. n surgery is last resort. bariatrics surgeries are gastric restrictive reduce size of stomach n limit amount of food that can be eaten pts usually of gain the weight back or malabsorption surgeries which interfers with the absorption process of food and nutrients in which pts usually keep.the weight of or a combo of both preop: reinforce health teaching with education classes. operative: gastric restriction surgeris are: LAGB band around proximal stomach. for LSG they remove the protion of the stomach where ghrelin the hunger hormonr id secreted. most common malabsorption surgery is the Roux en Y gastic bypass where the pts stomach duodenum and part of the jejunum is bypassed. postop: airway mgmt. n safety extra wide beds n personnel to help move pts. skin breakdown, NG tube patency never reposition tube becsuse its movement csn disrupt the suture line. clear liquids introduced slowly...pureed foods, broth, souo, eater n milk 24-48after. liquids or pureed for 6 weeks. watch for anastomotic leaks which shows as increasing back shoulder abd pain restlessness tachycardia and oluguria. apply abd binder to prevent wound dehiscence, semifowlers cpap ventilation at night for breathing monitor oxygen sat at 2L compression stockings. absorbent padding remove cath 24hrs. out of bef on day of surgery. ambulate. measure girth. 6 small meals. obesity is chronic life long. |
|
|
|
hormones known as adipokines work to affect appetite n fat metabolism
|

|
|
|
|
discharge teaching after bariatric surgery
|

|
|
|
|
gastric cancer diet
|
TPN
HIGH FAT : HIGH PROTEIN: whole milk n milk products peanut butter nuts n seeds beef chicken fish pork n eggs. high calorie: sugar cream gravy oil butter mayo dried fruit avocado and honey. LOW CARBS: so they will be high in residue so things like fruits and veggies whole grains |
|
|
|
cirrohsis diet
|
HIGH CALORIE: sugar cream gravy oil butter mayo dried fruit avocado n honey.
PROTEIN RESTICTED DIET: just enough protein to maintain nutritional status: pastas bread cookies wafers geltatin made with wheat starch. carbs in powder or liquid form. some veggies and fruit. |
|
|
|
pancreatitis diet
|
HIGH CARB:
HIGH PROTEIN: milk and milk products peanut butter nuts and seeds beef chicken fish pork eggs. LOW FAT: low fat saturated fat trans polyunsaturated and monosaturated. |
|
|
|
hepatic encephalopathy
|
HIGH PROTEIN/HIGH CARB: whole milk and milk products peanut butter nuts and seeds beef chicken fish pork and eggs. white bread cereals and pastas.
|
|
|
|
ostomy diet
|
avoid high fiber high cellulose foods...
no fruits veggies whole grains or things that cause gas like broccoli and limit dairy products. |
|
|
|
UC diet
|
low fiber:
foods high in carbs are low in residue so white bread cereals pastas. high protein/calorie diet: sugar avocado seeds beef chicken pork fish eggs cream gravy oil butter mayo honey. avoid milk products and fruits and veggies and whole grains. |
|
|
|
Crohns diet
|
low residual high cal protein vitamin low fiber diet:
foods high in carbs are low in residue so white bread cereals pastas. sugar avocado seeds beef chicken pork fish eggs cream gravy oil butter mayo honey. avoid milk products and raw fruits and veggies and whole grains. |
|
|
|
cholecystitis/cholelithiasis diet
|
low fat liquids like powdered supplements high in protein carbs stirred into skim milk. avoid fried foods pork cheese and alcohol. have a low fat high carb high protein diet.
|
|

