![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
68 Cards in this Set
- Front
- Back
|
Std. Deviations Acceptable for Medical Care
|
(+) or (-) 2SD
|
|
|
Accuracy
|
Error prone and doubtful
|
|
|
Precision
|
Repeatable and reproducable
|
|
|
Sensitivity
|
Probability that a result will be (+) in presence of disease (high sensitivity = not likely to give false negative)
Sensitivity = TP/(TP+FN) |
|
|
Specificity
|
Probability that a result will be negative in absence of disease (high specificty = not likely to give false positive)
Specificity = TN/(TN+FP) |
|
|
Predictive Value
|
PV(+) = TP/(TP+FP), how good a positive test is in prediction of disease
PV(-) = TN/(TN+FN), how good a negative test is in prediction of disease |
|
|
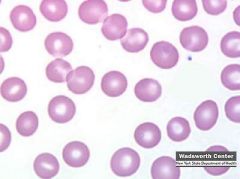
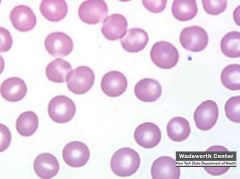
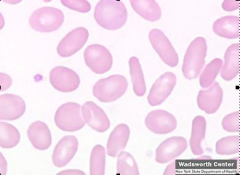
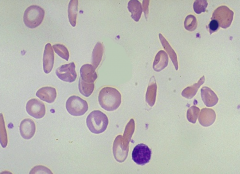
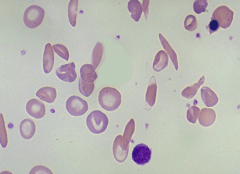
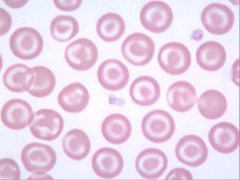
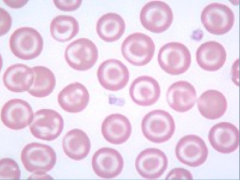
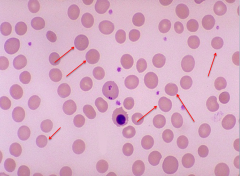
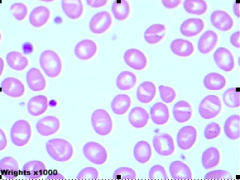
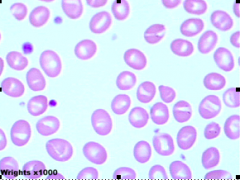
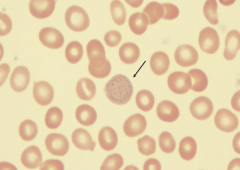
Erythrocyte
RBC, biconcave, central pallor (1/3) of cell due to ⬇[Hb] in center. Uniform shape, 7.2 microns. 120 day life span (spleen has immunological fxn by stimulating macrophages to remove dead/old RBC and inclusions. Pitting - removal of inclusions) |
|
|
Anisocytosis
|
Abnormal variation in size of RBCs. RDW > 18
|
|
|
Macrocyte
Large RBCs seen in Vit.B12 or folate deficiency (megaloblastic anaemia). Seen in pernicious anaemia, liver disease, in patients with underactive thyroid glands, in some bone marrow diseases, and sometimes in pregnancy. |
|
|
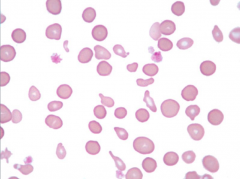
Microcyte
Small RBCs. Seen iron deficiency anaemia, long-standing inflammation due to infections or conditions such as rheumatoid arthritis, or to an inherited disorder such as thalassaemia |
|
|
Poikilocytosis
Variation in the shape of an RBC and may include several different abnormalities at the same time |
|
|
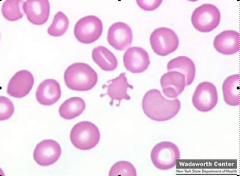
Acanthocytes (spur, thorn or spiculated cells)
Irregular shaped cells with 5-10 spines. May be present with liver or thyroid conditions, or in post-splenectomy patients. |
|
|
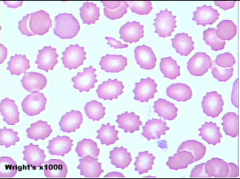
Echinocytes (burr, crenated or berry cells)
May have 10-30 spiny projections and often seen in patients with renal failure or malnutrition May be an artifact- something caused during sample preparation |
|
|
Elliptocytes
Elliptical-shaped RBC seen in hereditary elliptocytosis and various anaemias. |
|
|
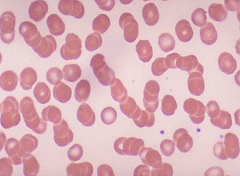
Rouleaux
RBCs that appear as a stack of coins caused by ⬆[Plasma protein] or when dehydrated. Seen in patients with inflammatory illnesses, anaemia, multiple myeloma or macroglobulinaemia |
|
|
Sickle cells
Crescent-shaped RBCs characteristic of sickle cell anaemia. |
|
|
Target cells (leptocytes or codocytes)
RBCs that look like a bull's-eye, ⬆[Hb] in center of cell. Seen in patients with liver disease, iron deficiency, haemoglobinopathies, (abnormal inherited forms of haemoglobin), thalassaemia. Also may be an artifact of smear-making process. |
|
|
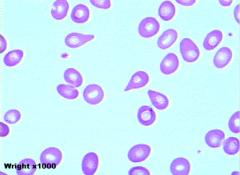
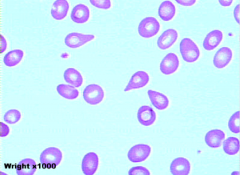
Teardrop cells (dacrocytes)
RBCs that resemble a teardrop. Often seen in patients with myelofibrosis |
|
|
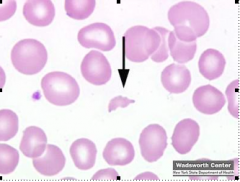
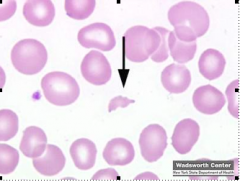
Schistocytes (Keratocyte, Horn cell)
Fragments or broken pieces of RBCs. This may be due to a disorder that is causing the red blood cells to be especially fragile or due to mechanical haemolysis as seen sometimes with devices such as artificial heart valves, or in severely burned patients. |
|
|

Spherocytes
Sphere-shaped RBCs found in hereditary spherocytosis or in autoimmune haemolytic anaemia. |
|
|
Hypochromasia
|
The RBC is pale in colour due to L[Hb] and contains a large, central pallor > 1/3 of the cell. This may be seen in a variety of disorders including thalassaemia and iron deficiency.
|
|
|
Polychromasia
|
Blue-staining RBCs, indicating that they are immature due to early release from the bone marrow. Earlier = more grey-blue coloration
|
|
|
Stomatocytes
RBCs that are loosely folded, with mouth-like pale areas across the cells. Seen in heredity stomatocytosis, lead poisoning and thalassemia trait |
|
|
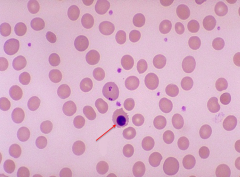
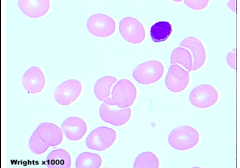
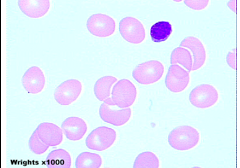
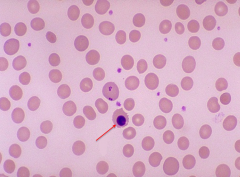
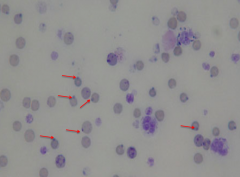
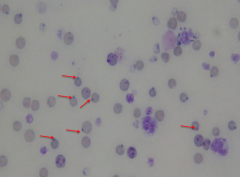
Nucleated RBCs (normoblasts)
Very immature RBCs Small, round, or ovall nucelus with coarser chromatin strands, pink cytoplasm. Generally, seen when there is a extreme need for RBCs to be released by the bone marrow. Seen in abrupt blood loss, severe anaemia, myelofibrosis, thalassaemia, miliary tuberculosis and in cancers that involve the bone marrow. nucleated RBCs can be normal in infants for a short time after birth. |
|
|
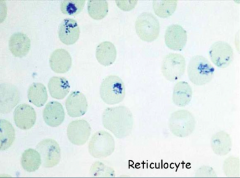
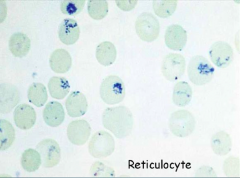
Reticulocytes
AKA macrocyte that is kicked out early from marrow, also polychromatophillic. rRNA in cell causes increased pigmentation. Earlier = larger in size/more rRNA. Seen with acute blood loss, hypoxia, RBC destruction (“haemolysis”, such as in sickle cell disease, glucose-6-phosphate dehydrogenase (G6PD) deficiency and autoimmune haemolytic anaemia). |
|
|
Basophilic stippling
Small dark-blue dots in RBC that represent the precipitation of nuclear material (rRNA). Seen in heavy metal poisoning (such as lead), nutritional deficiencies, or myelofibrosis. |
|
|
Heinz bodies
Granules the RBCs when stained with crystal violet, represent denatured Hb. Seen in enzyme (G6PD) deficiency, unstable haemoglobin variant, thalassaemia, and autoimmune haemolytic anaemia. |
|
|
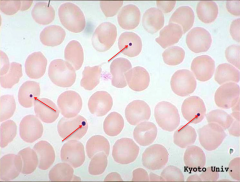
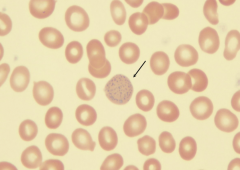
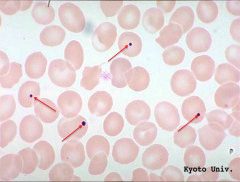
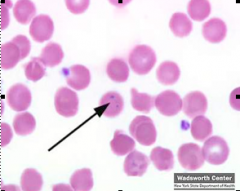
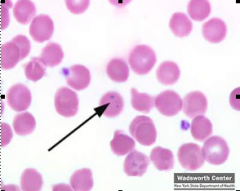
Howell-Jolly Bodies
Small round remnants of nuclear DNA inside cell. Seen in sickle cell anaemia, haemolytic or megaloblastic anaemias, and may be seen after a splenectomy. |
|
|
Pappenheimer bodies
Granules of iron in RBC found along the edge, often in clusters. |
|
|
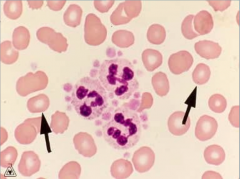
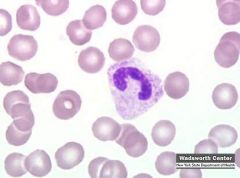
Neutrophils (also called segmented neutrophils, polymorphonuclear cells, polys or PMNs)
Function is to engulf and destroy invading organisms. 65 - 80% of the total WBC count in the peripheral blood. 2 - 5 nuclear lobes connected by a thin strand of nuclear material. Seen in greater numbers during infections, malignancies or extreme stress situations. Using a standard Romanowsky dye These granules (specific granules and azurophilic granules) contain enzymes and proteins that neutralise or destroy microorganisms. |
|
|
Toxic granulation
Large dark blue granules in the cytoplasm, associated with severe infection, chemical poisoning, alcohol abuse. |
|
|
Vacuolisation
|
Vacuoles appear as holes in the cytoplasm and are frequently found in association with toxic granulation.
|
|
|
Döhle bodies
Irregular greyish or greenish inclusions in the peripheral cytoplasm of neutrophils. Nuclear remnants that are often seen in association with toxic granules and vacuoles. Present in burns, trauma, acute or systemic infections, and exposure to cytotoxic agents (ie, chemotherapy). Also be seen in normal pregnancy. |
|
|
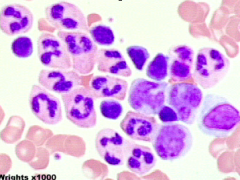
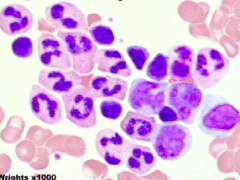
Blasts
|
Immature granulocytes, evenly stained chromatin, no granules
|
|
|
Auer Bodies (Auer Rods)
Unique, pink or red rod-shaped inclusions that are seen in very immature granulocytes ("blasts") in patients with acute myeloid leukaemia(AML). |
|
|
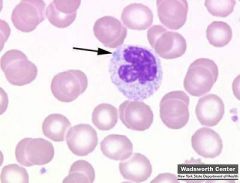
Band Neutrophil
Immature neutrophils with a non-segmented but elongated nucleus. Normal if seen in small numbers (<5% - <10%) but if ⬆ of them, there is said to be a “left shift.” (>15%) Seen in acute infection: stimulates increased neutrophil production causing the bone marrow to prematurely release some WBCs before they have matured to the neutrophil stage. |
|

|

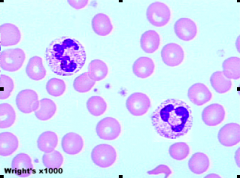
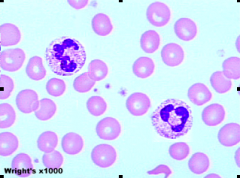
Hypersegmented Neutrophil (Right Shift)
Neutrophils with 6 or more nuclear segments. Seen in B12 and folate deficiency, less often with iron deficiency and rarely with infections. |
|
|
Eosinophils
2 or 3 lobes to their nucleus and contain characteristic reddish/orange granules in their cytoplasm. Seen inn allergic responses and parasitic infections. About 1 - 3% of WBCs are eosinophils. |
|
|
Basophils
Multi-lobed nucleus and have many dark blue granules (which contain histamine) in their cytoplasm. 1% of WBCs are basophils. Seen during an allergic response, ulcerative colitis, chronic sinusitis, chicken pox and immunisations. A significant increase happens in certain myeloid leukaemias. |
|
|
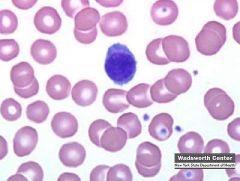
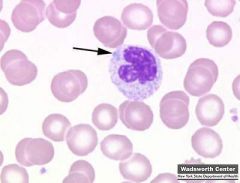
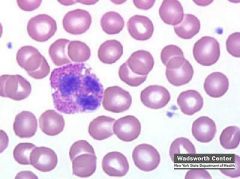
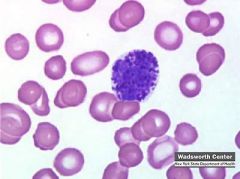
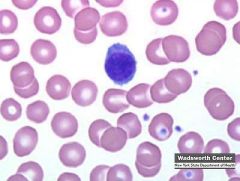
Lymphocyte
Small (7 - 10 um) and round in shape. Nucleus = large compared to the cytoplasm and smooth/dark blue. Cytoplasm = pale blue and generally does not contain any granules. 2 major types of lymphocytes, B cell and T-cell, but they cannot be distinguished when viewed under the microscope using standard staining techniques. Must use flow cytometry. B cells create specific antibodies while T-cells can activate B cells as well as recognise and destroy invading organisms. Lymphocytes make up about 20% to 40% of the total WBC count. |
|
|
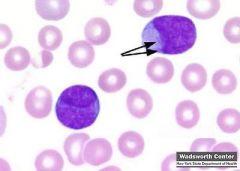
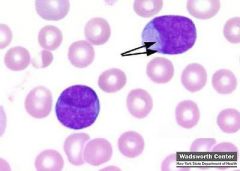
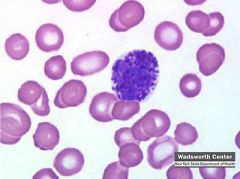
Hairy cells
|
Lymphocyte that have tiny projections that make them appear hairy under the microscope. They are found in hairy cell leukaemia.
|
|
|
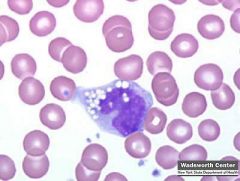
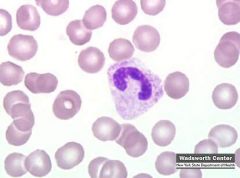
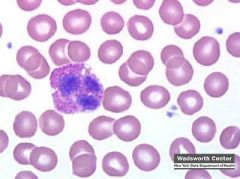
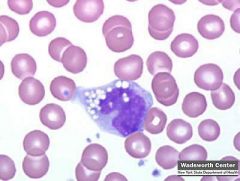
Monocytes
Largest of the WBCs and comprise less than 6% in normal blood. Abundant blue-grey cytoplasm that is irregular in shape and have a folded nucleus. Ingest microorganisms and respond to infection and inflammation by releasing certain proteins (monokines) that can inactivate bacteria. When stimulated by cytokines, monocytes can move out of the bloodstream and become tissue macrophages. |
|
|
hCG
|
Only produced by placenta (via syncytial trophopblasts of chroionic villi) and tumors.
β-subunit has the unique properties to HCG. Only test for β using monoclonal ab – good test. α-subunit shares properties w/ FSH, LH, TSH |
|
|
Pregnancy Tests
|
Serum test is more accurate (urine tests can have FP resulting from drugs/protein).
Positive = 10 mIU/mL (5 days post conception). Home pregnancy tests lack specificity but have ok sensitivity. |
|
|
hCG Levels
|
Normal: doubles q48h, reaching max at 10 wks.
Abnormal:⬆ [hCG] past 10 wks = mole. FP = hCG producing tumors FN = test is ordered too early Ectopic pregnancy - lower hCG levels than expected. Twin pregnancies - higher hCG levels due to two placentas |
|
|
Hydatidiform mole
|
Seen in young and older pregnancies. hCG produced by mole can induce hyperthyroidism (⬆T4)
|
|
|
L/S Ratio
|
Lecithin/Sphingomyelin Ratio.
Determines if lungs are mature enough (have enough surfactant). > 2.0 not likely to develop RDS. < 2.0 RDS likely |
|
|
NTD
|
Neural tube defects.
|
|
|
AFP
|
α-fetoprotein.
Made in yolk sac early and GI/Liver later, circulates in fetal plasma/amniotic fluid. Reaches maternal blood at 14-22 wks. AFP testing is only a screening test. ⬆AFP = NTD, omphaloceles, hydroencephalus, twins. ⬇AFP = Down's, overestimation of gestational age (most common). If Amniotic fluid AFP = ⬆, also check for ⬆AF AChE should also be measured since it is only produced my neural tissue |
|
|
Triple Test
|
Measures AFP, hCG, unconjugated estradiol. Down's = ⬇AFP, ⬇estradiol, normal hCG
|
|
|
MOM
|
Multiple of Medians.
Each lab determines own AFP reference values based on sample size/time in gestation. Median is obtained for each week. MOM = AFP result/median of specific week. |
|
|
Erythropoiesis
|
Marrow pushes oldest cells out first in anemic conditions
RBC → Retic → Shift Retic → Metarubicyte (nucleated RBC) Stimulated by erythropoietin. Shift retic - released at least one day early |
|
|
α - Thalassemia
|
Hb disorder
RDW normal due to similar shape of RBC Deletions of 1 - 4 genes - Unable to use Hb electrophoresis for 1 and 2 deletions, can use α/β-chain analysis - 3 deletions - abnormal Hb = Hb-H disease = deletion of both α-globin genes, formation of 4 β-chains (migrates the fastest) - 4 deletions - incompatible w/life, Hb-Barts - 4 γ-chains |
|
|
β - Thalassemia
|
Hb disorder
RDW normal due to similar shape of RBC β-thal minor (β/β⁺) - Mild microcytic anemia = 1 β-chain slightly normal - Hb electrophoresis - ⬇ HbA β-thal major (β⁰/β⁰) - Severe hemolytic anemia - RBCs w/α-chain inclusions removed in spleen - ⬆ unconj. bilirubin (jaundice) - RBCs w/α-chain inclusions undergo apoptosis in bone marrow - Hb elctrophoresis - No HbA |
|
|
Iron-Deficiency Anemia
|
Body compensates by increasing hematopoiesis → faster production of RBC (⬆RDW)
Serum ferritin test = elevated in infections/malignancies → will mask Fe deficiency Caused by - Blood loss - Lack of iron - Inability to abs. iron - Pregnancy (⬆ demand for iron) |
|
|
Hyperbilirubinemia
|
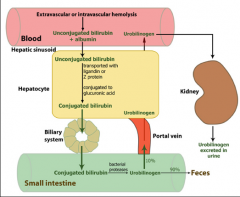
Bilirubin - yellow breakdown product of normal heme catabolism, excreted in bile and urine.
Causes jaundice UCB (indirect) Lipid soluble Increase suggests Increased production of UCB - hemolytic anemias Decreased uptake/conjugation - newborn jaundice CB (direct) Water-soluble Increase suggests Mixed - viral hepatitis (defect in uptake, conjugation of UCB, secretion of CB) Obstructive - drug induced, billiary cirrhosis Decreased bile flow - gallstone in common bile duct, carcinoma of pancreas head Newborns don't have glucuronyl transferase after birth and are unable to conjugate UCB |
|
|
RBC
|
Red blood cell count
|
|
|
Hb
|
Hemoglobin count
Indicates O₂ capacity of blood See decrease during infancy since Hgb F switches to Hgb |
|
|
Hct
|
Hematocrit
Ratio of volume of RBC to whole blood Changes in plasma vol. will affect hematocrit Approx 3x Hb |
|
|
RBC indicies
|
MCV
Mean corpuscular volume = (Hct/RBC)(100) Avg. vol of RBCs MCHC - Mean corpuscular Hb Concentration = Hb/Hct - Tells you about color of cells (polychromasia) Decrease - ⬇ Hb synth. → hypochromasia Increase - spherocytosis - Avg [Hb] in a given vol of packed RBC MCH (lesser value - not really needed) |
|
|
RDW
|
Red cell distribution width
Tells you about size of cells (⬆RDW = anisocytosis) ⬆ in early Fe deficiency anemia and mixed anemias Only microcytic anemias associated w/ ⬆ RDW |
|
|
WBC
|
Raw amount of WBC
If differential = divides leukocytes by percentage (band neutrophils, segmented neutrophils, lymphoytes, etc.) |
|
|
Granulocytes
|
Granules = lysosomal in cytoplasm
Neutrophils Bands/Stabs - immature, "Left shift" if there are a lot in circulation Eosinophils/Basophils Eosino - found in lungs/intestinal mucosa Basop - found in perip. blood Monocytes/Macrophages Mono - immature macrophages in circulation Macrophages - mature moncytes in tissue |
|
|
Lymphocytes
|
T-lymphocytes - cell-mediated immunity
B- lymphocytes - form Ab NK cells - kill shit |
|
|
Reticulocyte Count
|
Indicates effective erythropoiesis
% Retic = (retic count/1000 RBCs)/10 Reported as a percentage Falsely ⬆ in anemia, must be corrected for degree of anemia Corrected Retic. Count = (actual Hct/45)(retic. count) If you have polychromatophillic cells Index = corrected retic. count/2 |
|
|
ESR
|
Erythrocyte Sedimentation Rate
Normally cells have negative charge around them → repels other RBC Pathological - RBC settle rapidly due to positively charged plasma proteins that coat the surface → causes aggregation (rouleaux) Good for monitoring activity of inflamm. conditions, but is non-specific/non-sens. → use CRP (fast response and hangs around until infection) |
|
|
How do you determine if anemia is immunologic or not?
|
Non-immunologic - inherited
Immunologic - Ab on RBC, can test for this. Direct Antiglobulin Test (DAT) IgM and IgG differ in size. IgM is large enough to form agglutinated cells (spans distance = lattice structure). IgG is not long enough → no agglutination Coombs reagent = anti-human IgG is long enough to span distance between cells → agglutination DAT (+) = immunologic anemia |
|
|
MAHA
|
Microangiopathic Hemolytic Anemias
DIC = Disseminated Intravascualar Coagulation TTP = Thrombotic Thrombocytopenic Purpura HUS = Hemolytic-Uremic Syndrome Symptoms: Anemia and schistocytes on smear The endothelial layer of small vessels is damaged, resulting in fibrin deposition and platelet aggregation. The small clots consume coagulation proteins and platelets = normal coagulation disrupted. Small clots also disrupt normal blood flow to organs, resulting in malfunction. As RBCs travel through damaged vessels, they are fragmented = intravascular hemolysis and schistocytosis. The resulting schistocytes are also targeted for destruction by the reticuloendothelial system in the spleen, due to their narrow passage through obstructed vessel lumina. |

