![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
where are glomeruli located
|
cortex
|
|
|
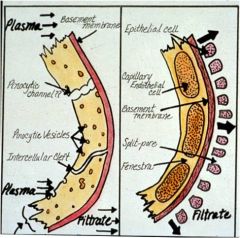
glomerular capillaries (no protein gets cross)
|
permeability of glomerulur capillary greater than permeability of muscle capillary for small molecular compounds, but smaller for proteins (more protein across muscle capillary than glomerular capillary)
|
|
|
post-renal problems (kidney stones)
|
Pt goes up
Q = Kf [(Pc - Pt) - (Pip - Pit)] |
|
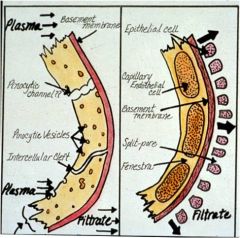
permeability of muscle cap to kidney cap
|
negative charge interacts w podocytes; they fuse/go away when you start spilling protein; dissappearance of podocyte = onset of micro albuminemia
|
|
where does protein trapped supepithelially go back through basement membrane back into capillary?
|
charge on all three layers are negative; proteins pushed back by negative charge
|
|
|
glucose is freely filtered
|
100 ml of water filtered = 100 ml of glucose filtered
filter out 100 ml, across filtration barrier into bowmans space; point: glucose free to filter, protein is not |
|
|
renal cap vs muscle cap
|
hydrostatic stays same, oncotic pressure increases in renal capillary
in muscle hydrostatic decreases towards venous side, oncotic decrease |
|
|
explain how tone of afferent/efferent arteriole can be altered to change plasma hydrostatic pressure
|
you can constrict one or the other independently to regulate pressure
|
|
|
filtration/equilibrium
|
offsetting pressures are equal to eachother from that point on to the end of the capillary
|
|
|
diabetes insipidous
|
no ADH
|
|
|
compare conc of glucose in the afferent and efferent arterioles
|
they're equal; when you move water you move glucose bc it's FREELY FILTERED unlike protein
|
|
|
factors which affect ability of molecules to move across the glomerular cpiallary
|
creatinine, urea, glucose
same conc in urine as in plasma bc they're all freely filtered |
|
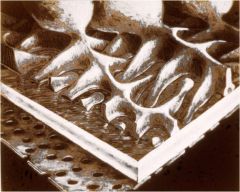
purpose of podocyte
|
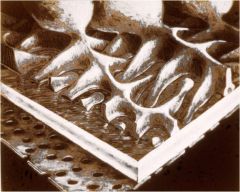
support to capillary basement membrane (bc theres on muscle in renal capillaries); inbetween interlocking parts is a filtration slit which is where filtration is thought to take place
|
|
|
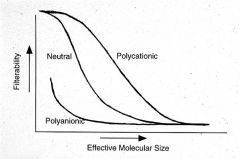
polyanionic = negative = not filtered well
neutral = bettter polycatoinic = positive = filtered best |
|
|
Donnan effect
|
proteins are held back in capillary fluid (negative charged); hold back positively charged ocmpounds like sodium or potassium
negatively charged compounds get pushed across faster |
|
|
how can you increase GFR and decrease renal blood flow
|
constrict efferents flow goes down, pressure goes up bc the flow is not getting up, GFR goes up, renal blood flow go down
|
|
|
how can insulin be used to calculate the GFR
|
C = UV/P
you can only do this with inulin bc it is freely filtered and is neither reabsorbed nor secreted |
|
|
characteristics a compound must have before it can be used to calculate GFR
|
cant be toxic, must be measurable, cant alter GFR, freely filtered, must be secreted or reabsorbed
|
|
|
rhabdomyolysis
|
breakdown of muscle; can be toxic to kidney
|
|
|
Pin x GFR = Uin x V
|
Urine volume x Concentration = amount excreted
Qf = Qe |
|
|
where is filtrate generated?
|
glomerulus
|
|
|
where does distal tubule pass next to?
|
glomerulus
|
|
|
what can the kidney synthesis
|
bicarb, some hormones
otherwise only puts stuff INTO the blood or takes it OUT of the blood |
|

How is renal tubular fluid obtained?
|
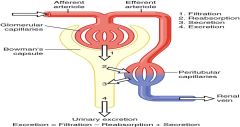
filtration (at glomerulus) and secretion
|
|
|
How much work do kidneys do?
|
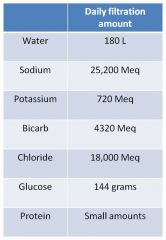
Huge amount (180L water); most material comes from blood and most goes back to blood
its a way to eliminate things from blood that we dont need |
|
why do we not need to consume this volume of filtered material
|
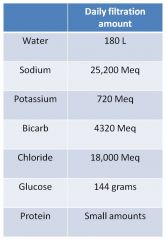
most material filtered by kidney is reabsorbed (similar to gut; material from blood into tubule, which makes it outside body)
|
|
|
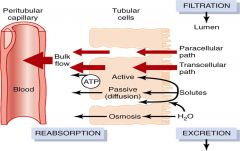
Filtration generates fluid -> (all small components from blood, no rbc or large proteins)
We absorb water by absorbing all the ions which drives the fluid through back into blood after filtration |
|
|
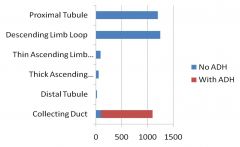
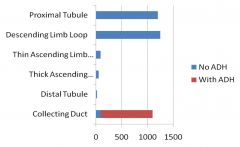
note collecting duct is impermeable to water without ADH initiation of aquaporin transport to membrane
|
|
|
which segment reabsorbs the most sodium
|
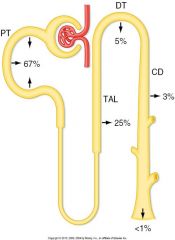
most in prox tubule
|
|
|
which segment absorbs sodium to adjust renal interstitial fluid concentrations?
|
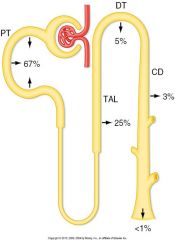
loop of henle
|
|
|
which segment is associated with regulation of sodium for body?
|
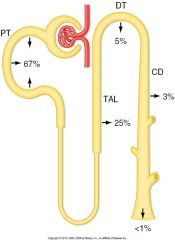
3% in CD; this is where sodium in blood is mostly regulated; all the other absorbtion sites are necessary
|
|
|
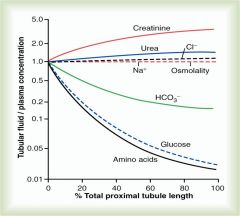
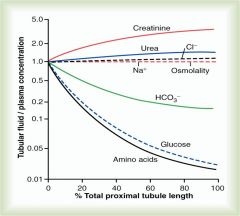
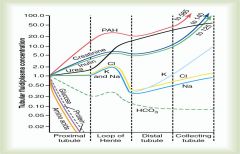
note AA, glucose at the end of the prox tubule are virtually zero; it means they are completely reabsorbed as the fluid moves along the proximal tubule
note the Na and Cl conc dont change much bc they draw water with them whenever theyre reabsorbed bicarb gradually reabsorbed (major buffer system in body) urea and creatinine as they move along their concentration begins to rise which indicates that they're not being reabsorbed |
|
|
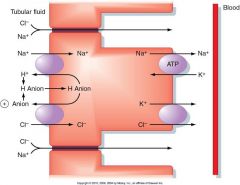
Na and H absorbtion in first half of prox tubule
|
Absorb sodium, secrete hydrogen which binds to bicarb (which generates C02 and water) -> this is how bicarb is reabsorbed bc bicarb is not permeable but C02 and water are permeable -> C02 diffuses out into the body to be reconverted into the body or secreted through lungs
this leaves Na, Cl, K, and water in the second half of prox tubule |
|
|
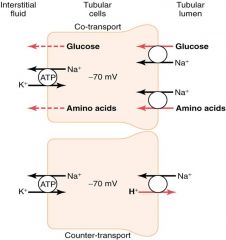
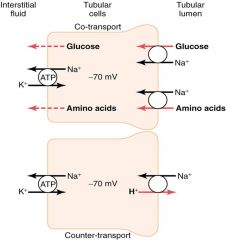
Secondray active transport: Glucose down conc. gradient by facilitated diffusion, Na exchanged by Na/K pum, same w/ amino acids (same as GI)
Note sodium, hydrogen exchange, combines with bicarb for C02, C02 reabsorbed note sodium bicarb exchanger (secondary active) |
|
|
Hydrogen ions going out, anion comes back in; electrically neutral process so doesnt disturb Na or cl reabsorption
These are mechanisms by which rebaosprtion processes are going on; specific transporters; |
|
|
why is glucose not normally present in urine?
|
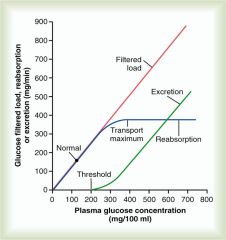
at normal blood glucose levels (blue line = transport); amount in filtered load is totally reabsorbed under normal conditions
|
|
What is the glucose excretion for this patient? (GFR = 90, plasma glucose = 2 mg/ml, Tm = 150)
|
Filteredglu = GFR x Pglu = 90 x 2 = 180 mg/min
Reabsglu = Tmax = 150 mg/min Excretglu = 30 mg/min |
|
|
What stuff is secreted in the proximal tubule?
|
Endogenous anions, cations, drugs; once this stuff is in the renal filtrate it ends up in the urine
|
|
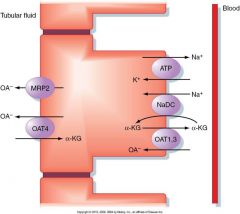
anions
|

Yes you have to know what OAT1,3,4 do; they can be targets of drugs causing excretion or reabsorbtion
cations |
|
|
distal convoluted tubule: continues the dilution started by the ascending limb
|
at the top of loop of henle you have the highest conc of fluid in the body; as it moves up it loses ions (diluting fluid) as it enteres DCT; as it contines sodium and Cl reabsorbed back into body but water is NOT rebaosbred (these cells dont have aquapores); this dilutes fluid
|
|
|
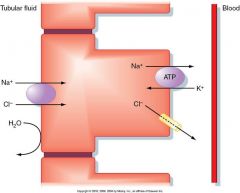
Sodium chloride transport in early distal tubule
|
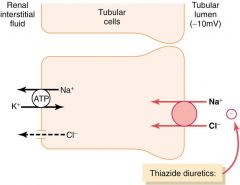
Site for thiazide diuretics; if you block the reabsorbtion of sodium and chloride you have a large ionic content in tubule which traps water in the tubule which is excreted in collecting duct
|
|
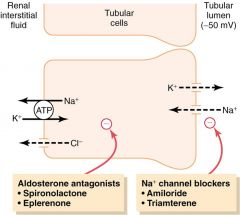
what does aldosterone do?
reabsorption of sodium (not really regulation bc the sodium came from blood and puts it back into blood) |
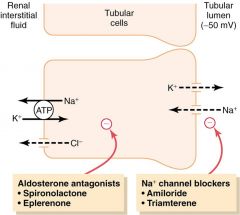
Potassium into tubular lumen, sodium reabsorbed, potassium taken out of interstitial fluid
SECRETION of K in exchanged for Na and Cl; Na/K pump sensitive to aldosterone which moves greater amounts of sodium into blood which leads to increased potassium excretion |
|
|
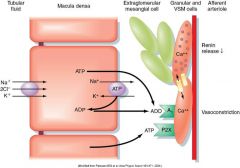
Macula densa
|
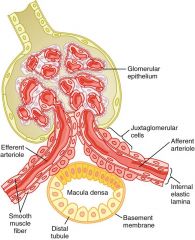
located on distal tubule; J/G cells along afferent and efferent arterioles
constrict afferent (filter less) constrict efferent (filter more bc increased pressures) can adjust both proportionally where nothing changes |
|
|
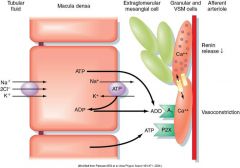
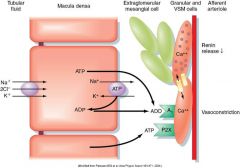
cells in macula densa sensitive to how much sodium is being reabsorbed; too much sodium in tubular fluid leads to too much sodium being reabsorbed which signals to cells to release adenosine and ATP detected by granular and vascular smooth muscle cells on afferent arteriole; will active CaC which will raise levels in smooth muscles = vasoconstriction
|
|
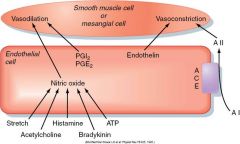
Note ATP will release NO in cell but in the macula densa ATP causes vasoconstriction when is acts ON muscle receptors
|
|
|
|
be familiar with this slide
|

