![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
Airspace disease
|
Alveoli fill with fluid or exudate (displacing the air within them).
Areas of alveolar filling appear dense, white and radio opaque. |
|
|
Consolidation
|
Means the lobe of the lung is essentially airless (as the alveoli are filled with inflammatory exudate).
|
|
|
Air Bronchogram
|
The larger central airways (still filled with air)
are surrounded by dense lung tissue and stand out in bold relief |
|
|
What structures are included in the pulmonary interstitium?
|
It includes the alveolar walls, interlobular septa and the peribronchovascular interstitium.
|
|
|
Interstitial Lung Disease
|
While the majority of these disorders do affect the airspaces, the predominant abnormality is thickening of the interstitium which may be due to the accumulation of fluid, cells or fibrous tissue.
(inflammation, infection,, fibrosis, fluid) |
|

|
Normal
|
|
|

Lung metastases
|
|

|
Metastases from renal cell cancer
|
|

|
Thymoma. A chest x-ray (A) reveals an unusual contour over the right hilum That the hilum is not obscured (no silhouette sign) indicates that the mass must either be in front of or behind the hilum. If filling-in of the space behind the top of the sternum and the ascending aorta is seen, you are most likely dealing with an anterior mediastinal lesion.
|
|
|
Differential diagnosis of mediastinal masses
|

|
|
|
|
Thymoma. A chest x-ray (A) reveals an unusual contour over the right hilum That the hilum is not obscured (no silhouette sign) indicates that the mass must either be in front of or behind the hilum. If filling-in of the space behind the top of the sternum and the ascending aorta is seen, you are most likely dealing with an anterior mediastinal lesion.
A computed tomography scan (B) reveals a soft tissue mass (arrow) just to the right of the aorta. This is the most common location of a thymoma. |
|

|

Thymoma. A chest x-ray (A) reveals an unusual contour over the right hilum That the hilum is not obscured (no silhouette sign) indicates that the mass must either be in front of or behind the hilum. If filling-in of the space behind the top of the sternum and the ascending aorta is seen, you are most likely dealing with an anterior mediastinal lesion.
A computed tomography scan (B) reveals a soft tissue mass (arrow) just to the right of the aorta. This is the most common location of a thymoma. |
|

|

Sarcoid; marked lymphatnopathy is seen in the region of both hila in the right paratracheal region
|
|

|

Lymphadenopathy at both hila; transverse contrast enhanced computer tomography scan of the upper chest
|
|

|

(PULMONARY PARENCHYMAL FIBROSIS) Asbestosis tends to be prominent in the lower lobes and in the subpleural areas. When disease is advanced, the lungs are small, streaks of fibrosis outline lobar and interlobar septa, and the visceral pleura is invariably thickened. "Honeycombing" may be prominent subpleurally and in the lower lobes. Pleural plaques are distinctive, smooth, white, raised, irregular lesions usually found on the parietal and rarely on the visceral pleura. They may vary from small to extensive (up to 50 cm2) and are usually nonadherent. Common sites are the posterolateral mid-lung zones, where they may follow the rib contour, and on the diaphragm.
|
|

|

The reticular pattern of end-stage fibrotic (honeycomb) lung is characterized by cystic airspaces surrounded by irregular walls. The distortion of normal lung morphology by extensive fibrosis results in irregular dilatation of segmental and subsegmental airways (traction bronchiectasis); in the periphery of the lung, it can be difficult to distinguish dilated airways from true honeycomb change.
|
|

|
fine reticular lines in both lower lobes suggestive of interstitial pneumoniae
|
|

|
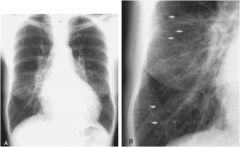
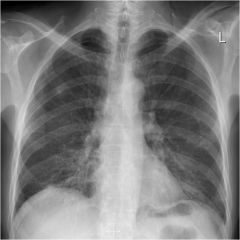
Early findings of congestive heart failure. The major signs on upright posteroanterior chest x-ray (A) are cardiomegaly and redistribution of the pulmonary vascularity. Normally the vessels to the lower lobes are more prominent than those in the upper lobes; however, here they appear at least equally prominent. On a close-up view (B), small horizontal lines can be seen at the very periphery of the lung (arrows). These are known as Kerley B lines and represent fluid in the interlobular septa.
|
|

|

CT scan thorax with IV contrast , axial image Lung window of a patient with cardiac failure. CT scan shows bilateral pleural effusions (red arrows), and interlobular septal thickening ( yellow circles and yellow arrow heads) in keeping with pulmonary edema.
|
|
|
DiGeorge's Syndrome
|
DiGeorge Syndrome, also called congenital thymic aplasia, is caused by a
deletion in chromosome 22q11.2. A transcription factor called TBX1 (T box-1) is encoded within this deleted chromosomal region. Mutations in the gene that encodes TBX1 result in a similar defect in thymic development. In both cases, there is a selective T cell deficiency which makes these patients susceptible to: viral infections due to a lack in CTLs; mycobacterial infections due to a deficiency in cytokines from TH1 cells, like IFN-γ, that are required for macrophage activation; and some fungal infections (Pneumocystis jiroveci), also due to a deficiency in T-dependent responses. |
|
|
Double Negative Thymocytes
|
Do not express CD4 or CD8; they are about to start rearranging the TCRB chain locus
|
|
|
Double Positive
|
Cd4+ and Cd8+
|
|
|
Positive Selection
|
While they are in the thymic cortex, double-positive thymocytes must bind self-MHC with self-peptides
on the cortical epithelial cells at least weakly or they will undergo apoptosis. |
|
|
Why are Ig levels decreased in DiGeorge's syndrome?
|
Decreased in severe dz bc a lack of T cell help for T-dependent antibody response
|
|
|
Association of thymic disorders with myasthenia gravis
|
Mh is a NMJ dz; associated with thymic hyperplasia or thymoma
|
|
|
Where does pleural fluid originate from?
|
Systemic vessels of the pleural membranes, specifically the lymphatics of the parietal pleura
|
|
|
Which pleural membrane is more important for normal pleural fluid formation?
|
Parietal
|
|

|

P = visceral pleural
F = fibrous supporting tissue S = fibrous septa M = mesothelial cells L = lymph vessels |
|
|
Pleural Cavity
|

|
|
|
Transudative Effusion
|
Alterations in hydrostatic or oncotic pressure (without altering pleural permeability); MCM = heart failure but also cirrhosis or nephrotic syndrome
|
|
|
Exudative Effusions
|
Secondary to processes that result in increased capillary permeability; MANY causes including pneumoniae, cancer, embolism, viral infection, TB
|
|
|
Chylous Effusion
|
Milky white effusion; commonly due to neoplastic damage to thoracic duct
|
|
|
Empyema
|
Pus in pleural space
|
|
|
Hemothorax
|
Pleural fluid hematocrit greater than 50% of peripheral blood hematocrit; bloody fluid in pleural space
|
|
|
Iatrogenic Effusion
|
May be due to feeding tube or CVP perforating SVC; results in infusion of IV oslution or tube feedings into the pleural space
|
|
|
Pleuritic Chest Pain
|
Pain or discomfort that worsens on inspiration; can indicate inflammation of parietal pleura
Pain location can be over site of inflammation or referred to neck, shoulder, abdomen |
|
|
What symptoms indicate pleural effusion
|
Pleuritic Pain (bc inspiration is compressing pleural fluid); unexplained dyspnea
cxr confirms |
|

|
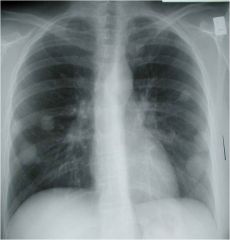
Normal chest xray
|
|

|
Large right pleural effusion
|
|

|
Interstitial pulmonary edema secondary to left heart failure' small left pleural effusion
|
|
|
Pale yellow/straw colored pleural fluid
|
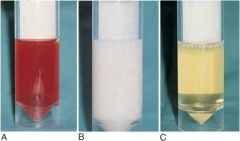
Transudate
|
|
|
Red pleural fluid
|

Blood; due to malignancy, trauma, pulm infarct
|
|
|
White (milky) pleural fluid
|

Chylothorax/chylous pleural effusion
|
|
|
Putrid odor to pleural fluid
|

Anaerobic empyema
|
|
|
Turbid pleural fluid
|

Inflammatory exudate
|
|
|
High lipid content pleural fluid
|
Chylothorax
|
|
|
Characteristics of mycobacterium
|

Nonspore forming, aerobic rods
Complex lipid rich cell wall Acid fast staining |
|

Sequence of events in primary pulmonary tuburculosis
|

A. Time frame of first 3 weeks
B. Time frame greater than 3 weeks |
|
|
Which cells are mainly infected in TB
|

Macrophages; early infection = unchecked proliferation. Late infection = macrophage stops proliferation and caseous granulomas develop
|
|
|
What happens 3 weeks after a TB infection?
|

Approximately 3 weeks after the infection a T helper (TH1) response develops and activates the macrophages
Mycobacterial antigens enter the draining lymph node and are displayed to T cells initiating the response TH1 cells in the lymph nodes and lung produce IFN gamma INF gamma stimulates the formation of the phagolysosome in the infected macrophages and is therefore critical in enabling the macrophage to control the TB infection The TH1 response is also involved with granuloma formation and the development of caseous necrosis Macrophages stimulated by IFN gamma can differentiate into “epithelioid histiocytes” which can then fuse to form giant cells Activated macrophages also secrete TNF which can result in the recruitment of additional monocytes The reactivation of infection or reexposure to the organism in a previously sensitized host results in a rapid immunological response but can also cause significant tissue destruction |
|
|
Primary Tuberculosis
|

Develops in individuals who are previously unexposed
Elderly and immunosuppressed who lose immunity can develop primary TB again |
|
|
Secondary Tuberculosis
|

Develops in previously sensitized hosts; reactivation of latent infection; exogenous reinfection
Classically involves the apices of the upper lobes of on eor both lungs Brisk reactoin due to preexisting hypersensitivity and cavitation can readily occur; can result in erosion of the cavity airway causing increased infectivity through coughing of infected sputum |
|

|
Ghon Complex; area of gray/white inflammation; combination of parenchymal lung lesion and nodal involvement; usually undergoes fibrosis; radiologically detectable as calcification
|
|

|

A and B: Tubercle. Note the central caseation and the surrounding epithelioid and multinucleated giant cells. This is the normal response seen in those who have cell-mediated immunity.
C: This is a tubercle without caseation D) This is an example of a reaction in an immunosuppressed patient (without cellular immunity) – note sheets of macrophages packed with mycobacteria. |
|

|

The initial lesion is typically an area of consolidation less than 2 cm diameter that is located within 1-2 cm of the apical pleura
; may heal w fibrosis or dz may progress |
|
|
Scrofula
|
Tb involvement of hte cervical region
|
|
|
Intestinal TB
|
Swallowing of coughed up infectious material
|
|
|
Potts disease
|
Tb infection of vertebrae
|
|

|
Miliary TB involving the spleen; the cut surface shows gray white tubercles
|
|
|
|
Acid fast stain; red rods of TB
|
|
|
|
Acid fast stain; red rods of TB
|
|

|
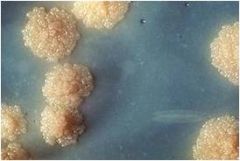
Egg based mycobacterial culture; dry, granular, buff colored colonies
|

