![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
32 Cards in this Set
- Front
- Back

Step 1 in allergy response?
|

DC* phagocytoses antigens and begins to express costimulatory molecules [B7-1 (CD80); B7-2 (CD86)] and CCR7 which causes it to travel through lymph to LN* paracortex (T cell area). This starts the adaptive immune response. DCs activated in this way (without recognition of microbial products by PRRs* since the antigen is not a microbe) do not produce IL-12.
|
|

Generic Allergic Response
Step 2? |

*DCs present peptides from ingested antigens on MHC class II to naïve CD4+ T cells. CD28 on T cells also binds costimulatory molecules (listed above) on DCs. Naïve CD4+ T cells become activated.
|
|

Generic allergic response
Step 3? |
*IL-4 from previously activated CD4+ TH2 cells or mast cells causes differentiation of newly activated CD4+ T cells into TH2 effector and long-lived TH2 memory cells. Some TH2 effector cells lose expression of CCR7 (and begin to express some CXCR5), causing them to move out of LN paracortex and toward the LN follicles.
|
|

Generic Allergic Response
Step 4? |

Antigens enter LN* via lymph and activate naïve B cells in LN follicles by binding to their BCR (C3d on antigen also binds CR2 on B cell)*. Newly activated B cells begin to lose expression of CXCR5 and begin to express CCR7, causing them to move toward the newly activated CD4+ TH2 cells at the edges of the LN follicles. Bound antigens are taken up by receptor-mediated endocytosis into activated B cells, processed into peptides, and loaded onto class II MHC and presented to these TH2 cells.
|
|

Generic Allergy Response
Step 5? |

IL-4 (+ IL-13) produced by TH2 cells, and interactions between CD40L on the TH2 cells and CD40 on the B cells, cause B cells to class switch from IgM to IgE.
|
|

Step 6?
|

B cells differentiate into plasma cells that secrete IgE antibodies which bind FceRI (high affinity receptor for IgE) on mast cells (also on eosinophils and basophils).
|
|

Generic Allergic Response
Step 7? |

Other effector TH2 cells lose expression of CCR7 and travel out of LNs* to other sites where the antigen is present, being presented by local antigen-presenting cells (i.e., macrophages). Cytokines from these TH2 effector cells are responsible for:
IL-5: eosinophil production (by bone marrow) and activation IL-4: differentiation of newly activated CD4+ T cells into TH2 cells in local LNs IL-13 (+ IL-4): mucus secretion by epithelial cells IL-13: stimulation of fibroblasts to synthesize collagen (long-term this can cause tissue fibrosis) IL-4, IL-13 and IL-10: alternatively activate macrophages, so that they produce IL-10, TGF-b and growth factors. Although alternatively activated macrophages play an important role in wound healing, cytokines produced by these cells (especially TGF-b) may cause pulmonary fibrosis. |
|

Generic allergic response
Step 8? |

Cross-linking of FceRI on mast cells or basophils (not shown) by multivalent antigens* activates these cells which causes them to degranulate*, produce/release lipid mediators, and secrete cytokines (IL-1, TNF-a; IL-4, IL-5 and IL-13). Lipid mediators*, chemotactic factors, PAF* and cytokines released from mast cells recruit and activate eosinophils, basophils, neutrophils and TH2 cells*. Products from these recruited cells amplify the reaction, cause tissue damage and inflammation.
Cytokines from activated mast cells are responsible for: IL-1 and TNF-a: inflammation IL-5: eosinophil production (by bone marrow) and activation IL-4: differentiation of more newly activated CD4+ T cells into TH2 cells in local LNs IL-13 (+ IL-4): mucus secretion by epithelial cells IL-13: stimulation of fibroblasts to synthesize collagen (long-term this can cause tissue fibrosis) |
|

Generic allergic response
Step 9? |

Major basic protein and eosinophil cationic protein (both toxic to epithelial cells), and proteases from eosinophils contribute to tissue damage.
|
|
|
Development and Migration of B and T cells
|

|
|
|
CXCR5
|
Chemokine receptor that binds chemokines produced in LN follicles
|
|

CXCR5
|
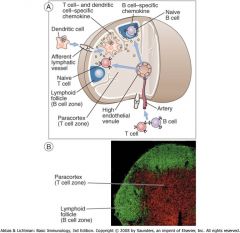
Chemokine receptor that binds chemokines produced in LN follicles
|
|

CCR7
|

Chemokine receptor that binds chemokines produced in LN paracortex
|
|
|
Actiavted T and B cell interaction
|

|
|
|
What stimulates class switching to B cell IgE?
|

IL-4 produced by TH2 cells
|
|
|
Atopic
|

Genetically predisposed to allergy
CD4+T cells respond to IL-4; this happens more often in people who are atopic |
|
|
IL-4
|

Induce B cells to class switch to IgE
|
|
|
IL-5
|

Important in development and activation of eosinophils
|
|
|
IL-13
|

Stimulates mucus secretion by epithelial cells (an allergy/asthma symptom)
|
|

Mast Cells
|

Arise in BM from stem cells;
IL-9 = mast cell production |
|

Sensitization phase of immediate hypersensitivity
|

TH@ cells produced to antigen (bee venom); IL-4 from TH2 induces B cells to switch to IgE
Plasma cells produce IgE; IgE binds with high affinity to FCR1s on mast cells, basophils and eosinophils throughout the body |
|
|
What kind of antigen is necessary to cross link bound IgE on FCR1s on mast cells?
|
Multivalent antigens;
cross linking results in mast cell activation and degranulation |
|
|
What kind of antigen is necessary to cross link bound IgE on FCR1s on mast cells?
|

Multivalent antigens;
cross linking results in mast cell activation and degranulation |
|
|
Anaphylaxis
|

Antigen cross links IgE bound on FCR1s on mast cells; mediators released upon degranulation can cause bronchial constriction, massive tissue edema and cardiovascular collapse
|
|
|
Products of activated mast cells and anaphylaxis
|

Mast cell granules contain vasoactivate amines (HISTAMINE), lipid mediators and platelet activation factor
Granule contents and lipid mediators are primary cause of immediate or initial reaction (within minutes) of vasodilation, vascular leakage, and smooth muscle spasm |
|
|
Late Phase of Immediate Hypersensitivity Reaction
|

Leukocytes recruited to site;
|
|

Why do pts receive broad spectrum antiinflammatory drugs (corticosteroids) after severe allergic attacks?
|

Inflammation caused by tissue damage during late phase allergic reactions (leukocyte recruitment)
|
|
|
How do basophils contribute to Type I hypersensitivity (and anaphylaxis)
|

basophils are structurally similar to mast cells; are blood granulocytes that express high levels of FC3R1; when recruited to tissues they act like mast cells by producing vasoactivate amines, lipid mediators and cytokines; they thus contribute to type I hypersensitivity reactions
|
|

Superantigens and shock
|
Exposure to high concentration of superantigen activates large numbers of T cells (eventually leads to anergy)
Activated T cells produce large amounts of IFN-g (and TNF-a) IFN-g activates large numbers of macrophages which produce pro-inflammatory cytokines (IL-1, TNF-a) and nitric oxide (NO) TNF-a activates endothelial cells Activated endothelial cells produce NO This “cytokine storm” (especially TNF-a and NO) can cause shock due to peripheral vasodilation (decreases blood pressure) |
|
|
Toxic Shock Syndrome Toxin
|

TSST-I exotoxin of staph aureus
|
|
|
How do PRR cause septic shock?
|

Microbial (or damage) product binds to PRR (i.e., LPS binds TLR4)
Binding causes activation of receptor-bearing cells which produce factors (i.e., TNF-a, IL-1, IL-6, NO for macrophages) Endothelial cells become activated in response to microbial products or cytokines (i.e., TNF-a) Activated endothelial cells produce NO, IL-6 and IL-8* TNF-a, NO (+many other factors*) cause vasodilation (etc.) resulting in shock |
|
|
Describe the role of C5a and C3 a (called anaphylatoxins) in shock
|

Complement activation (directly by microbes; or indirectly through proteolysis by plasmin (cleaves C3) or kallikrein (cleaves C5), or proteolysis by mast cell proteases causes activation of mast (and endothelial) cells
Mast cells have receptors for C5a and C3a Because of the ability of C5a and C3a to activate mast cells, they are called anaphylatoxins Additionally: - C5a can cause vasodilation directly - C5a is chemotactic for leukocytes |

