![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
57 Cards in this Set
- Front
- Back
|
Frank Starling Relationship
|
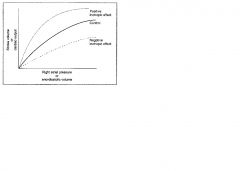
Increase in stroke volume and cardiac output in response to an increase in venous return or end diastolic volume
Increases in end diastolic volume cause an increase in ventricular fiber length, which produces an increase in developed tension; this mechanism matches cardiac output to venous return |
|
What mechanisms shift the frank starling relationship up or down
|
Changes in contracility
Increased contractility; increased cardiac output for any level of right atrial pressure or end diastolic volume Decreased contractility; decrease in cardiac output for any level of right atrial pressure or end diastolic volume |
|
|
Preload
|
End diastolic volume, related to right atrial pressure; increased venous return = increased end diastolic volume = lengthened ventricular fibers
|
|
|
Afterload
|
Aortic pressure in the left ventricle; increases in aortic pressure cause an increase in afterload on the left ventricle
for the right ventricle it's pulmonary artery pressure; increases in pulmonary artery pressure cause an increase in afterload on the right ventricle |
|
|
When is the velocity of contraction at a fixed muscle length maximal?
|
When the afterload is zero
|
|
|
What decreases the velocity of contraction at a fixed muscle length?
|
Increases in afterload
|
|
|
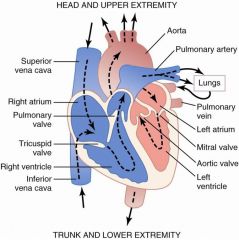
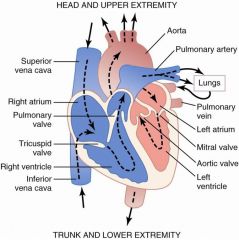
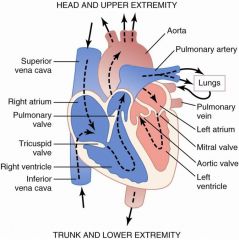
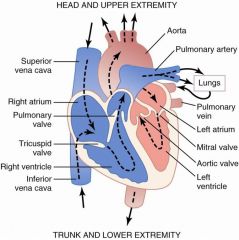
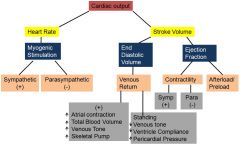
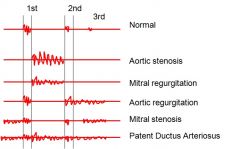
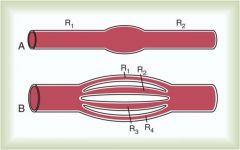
Name the valves!
|
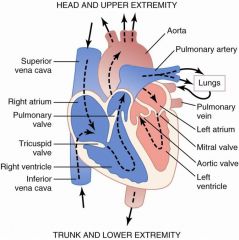
Clinical significance; usually tricuspid/mitral and aortic/pulmonary are simultaneous; if there is a delay that you can hear a difference there may be a pathologic condition involved
|
|
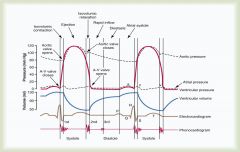
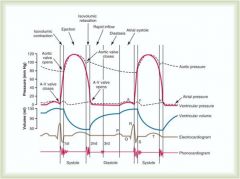
What is the first heart sound heard during the cardiac cycle?
|
Closure of the AV valves; closes with alot of force due to rapid increase in pressure in the ventricles compared to low pressure in the atria
Their large size = lower pitch "lub" |
|
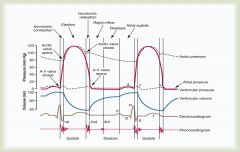
What is the second heart sound heard during the cardiac cycle?
|
Aortic and Pulmonary valves closing; sound is a little sharper and higher pitched then first sound "Dub"
|
|
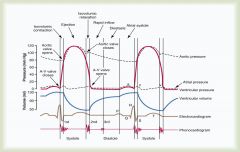
What is the 3rd heart sound heard in the cardiac cycle?
|
Very low pitch; caused by blood rushing into ventricles
|
|
What is the 4th heart sound in the cardiac cycle?
|
atrial contraction late in diastole; hard to hear with stethoscope except in hypertensive patients with a thick left ventricle
|
|
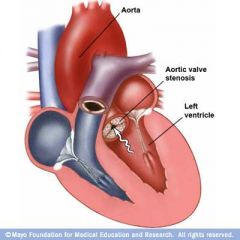
Stenosis of Valve
|
Stenosis = narrowing of valvular opening and fluid can't flow through as easily
2 problems; turbulent flow through valve (additional noise occuring when normal heart sound would not be heard) increase in pressure from which the blood is flowing and decrease in pressure in receiving chamber ex) AV stenosis = increase in atrial chamber, decrease in ventricular chamber |
|
|
Stroke Volume
|
Amount of blood expelled from heart each time it beats
|
|
|
Heart rate
|
Number of times the heart beats per minute
|
|
|
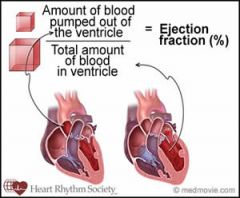
Cardiac Output
|
Amount of blood pumped out of the heart per minute
|
|
|
Why might you have a decreased stroke volume at high heart rates?
|
Ventricles fill less = less output per beat = less stroke volume
|
|
|
Cardiac Output = ?
|

Cardiac Output = Stroke Volume x Heart Rate
|
|
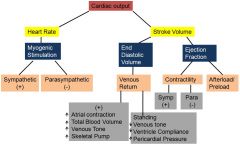
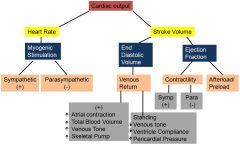
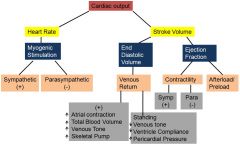
How is cardiac output regulated?
|
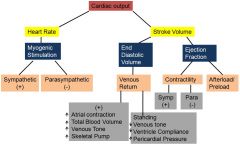
Know these relationships well
|
|
How does standing affect venous return?
|
Decreases it decreasing end diastolic volume, decreasing stroke volume, and decreasing cardiac output
|
|
|
What the normal ejection fraction?
|
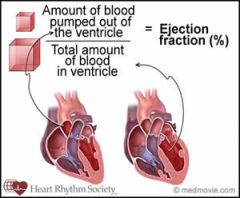
70%
|
|
Relationship of contractility and ejection fraction
|
Increase contractility = increased ejection fraction
Decreased contractility = decreased ejection fraction |
|
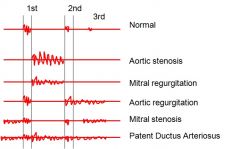
What is a potential complication of aortic stenosis?
|
Left ventricular hypertrophy
Heart is overworked; increased oxygen demand; growth of heart tissue = decreased contractility = decreased cardiac output |
|
How might aortic regurgitation affect ventricular pressure?
|
Increases ventricular pressure
|
|
Mitral Stenosis Complications
|
Increased atrial volume leads to increased atrial fibrillation; increased left atrial pressure could lead to pulmonary edema; increased right ventricular pressure could lead to right vent. failure
left ventricule normal |
|
Mitral Regurgitation Complications
|
Increased left atrial pressure can -> pulmonary edema
increased left atrial volume -> atrial fibrillation |
|
|
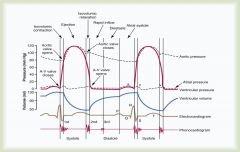
What is the pressure in the aorta relative to the ventricle during the rapid ejection phase?
|
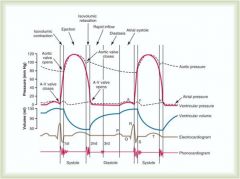
Aortic pressure is less; this is why blood is flowing through it from the ventricle
|
|
|
When does the aortic valve open?
|
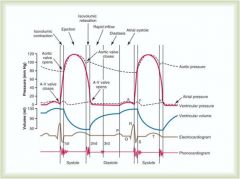
When ventricular pressure meets and exceeds aortic pressure
|
|
|
Why is blood flow to the heart muscle highest in diastole?
|
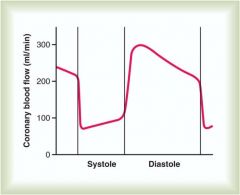
The heart contracting also prevents blood from flowing into it; coronary blood flow does not start until heart relaxation (diastole)
|
|
|
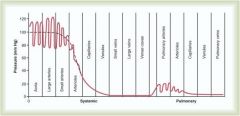
Pressure drops in capillaries as you move from arterial to venous side
|
|
|
Ohms Law
|
Q = dP/R
|
|

|
As the radius increase, the tension on the wall of a vessel increases (assuming constant pressure)
e.g. in the aorta it has a large cross sectional area relative to other vessels, larger radius, at a given pressure the tension on the walls will be greater; if the tension becomes great enough you get a tear in the wall which can cause a dissecting aneurysm |
|
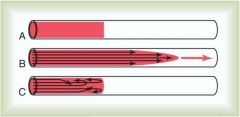
Reynolds Number
|
Useful for determining when turbulent flow will occur
Above 200-400 will result in turbulent flow at a branch in an artery Numbers above 2000 will result in turbulent flow in a straight artery Re = (V)(d)(p)/n |
|
|
Poiseuille's Law
|

Explains the effect of a radius change relative to blood flow rate
Diameter from 1,2 and 4; radius is a significant factor on the flow rate F = (pi)dP(r^4)/8nL |
|
|
Effect of Resistance in Series and Parallel
|
Series: the resistance is added
Parallel: As you increase # of capillaries the total resistance will decrease, so you consider conductance 1/Rtot = 1/R1 + 1/R2...etc |
|
|
Distensibility =?
|
Increase in volume/[(Increase in pressure)(original volume)]
|
|
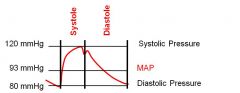
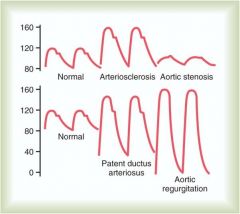
Relate to arterial pulse pressure
|
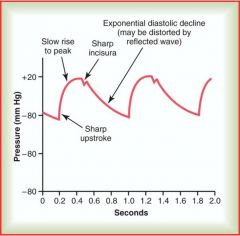
Incisura (notch)
Compare pressure in aorta to arterial pulse pressure Influences: perssure generated by left ventricle and total peripheral resistance by all the arterioles added to together; high resistance = lower runoff slope, lower peripheral resistance = rapid decay in pressure |
|
|
MAP = [(systolic-diastolic)/3] + diastolic pressure
MAP = ((120-80)/3) + 80 |
|
|
Vascular Filling Pressure
|
Pressure obtained in arteries and veins after heart stops; after heart stops blood flows from arteries into veins until an equilibrium pressure is reached; generally = 7 to 12 mmHg
|
|
|
why does systolic pressure increase as we move down the vascular tree from the heart towards the ankles?
|
Rebound from wall of aorta + wave of returning blood bouncing back through oncoming pulse of blood
But we really don't completely understand |
|
|
Relationship Between Heart & Circulatory System
|
Blood flow to tissue is delivered based on need
Cardiac output is determined by the sum of this need Pressure is controlled by other factors in the body which regulate and control pressure independently |
|
|
PDA and AR; high drop off pressure difference; resistance to outflow has been reduced by openings
|
|
|
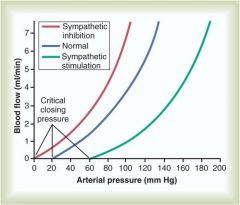
Effect of sympathetic inhibition and stimulation on arterial pressure and flow
|
|
|
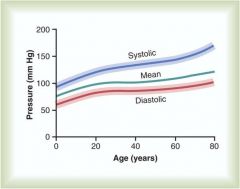
Blood Pressure and Age
Hardening of arteries may contribute to this |
|
|
Compliance
|
C = dV/dP
Used to compare how easily a vessel can be distended; you can only make an accurate measure when the vessel is filled and you add volume (otherwise there is no change in pressure); at this volume you reach the capacitance of the vessel and from there you can measure compliance (measure of wall of vessel, need filled vessel) |
|
|
Capacitance
|
Filling the container (what is its capacity)
|
|
|
When and only when can you measure compliance?
|
Only after the system is full
|
|
|
Volume distribution between venous and arterial
|
2/3 venous
1/3 arterial Note compliance of arterial side = 6.54 mils, if you add 6.54 mils the bp will increase 1 mmHg On venous side, youd have to ad 1650 ml of blood to make the bp increase 1 mmHg |
|
|
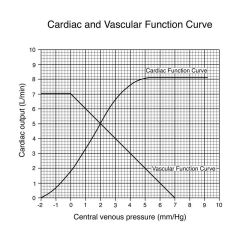
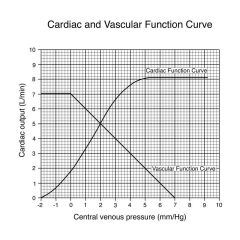
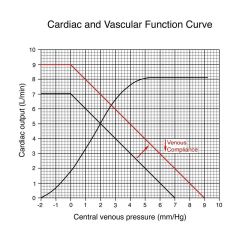
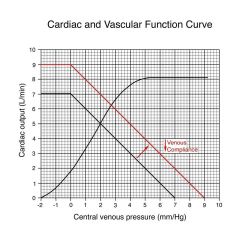
As we increase venous pressure we increase cardiac output
If we stop heart and move cardiac otput to zero, there would be an equilibration of bp at 7 mmHg; where two lines cross gives us a representation of where this system would operate (CO = 5, VP = 2) |
|
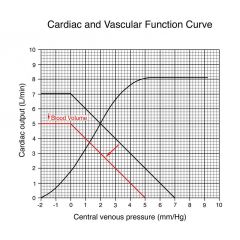
What happens to venous pressure if you decrease CO to 0
|
equilibration at 5 mmHg; filling pressure has decreased from 7 to 5 because of decreased volume in system; new cardiac output would be 3.8L and venous pressure would be 1.2
|
|
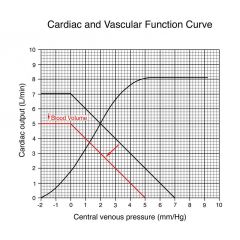
What happens if you add blood?
|
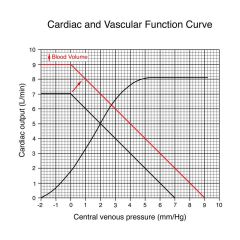
Filling pressure increases to 9
CO increases from 5 to 6.2 and venous pressure increases from 2 to 2.8 |
|
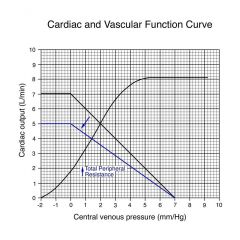
Increase total peripheral resistance
|
Done by constricting arterials; since we increase afterload by increasing TPR, CO decreases from 5 to 4, and VP decreases from 2 to 1.4
the decrease in CO is due to decreased VP and that the heart is having to pump against an increased pressure VP decreases because there is increased resistance to flow from arterial to venous side; more blood from |
|
|
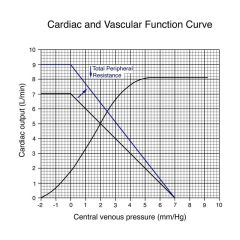
CO increases, VP increases, filling pressure remains the same; anytime we change TPR we change the slope of the line
changing blood volume changes filling pressure but does not change the slope |
|
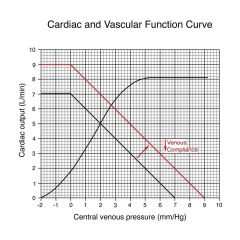
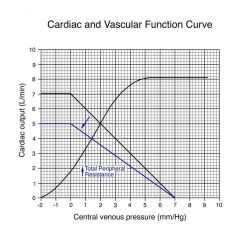
Decreasing venous compliance
|
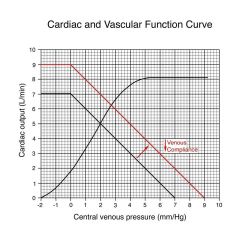
Makes change similar to what occurs if you add blood volume; equivalent to making walls of veins stiffer/thicker; equivalent to reducing the size of the container
amount of blood remains the same but an increase in VP due to the fact that the container is effectively smaller |
|
Increase in venous compliance
|
Similar to making wall of vein more distensible; similar to making container larger;
VP decreases, CO decreases, filling volume has decreased; similar to loosing blood |
|
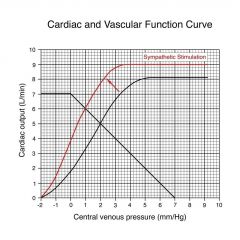
|
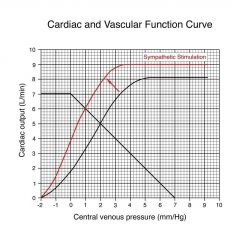
Increase CO to 6, decrease VP from 2 to 1
the decrease in VP is because were moving more blood from venous to arterial side; |
|
|
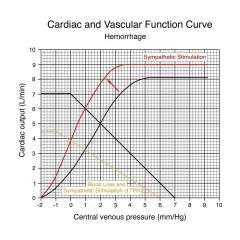
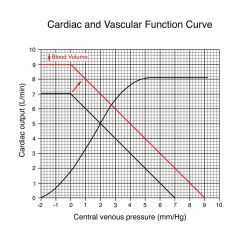
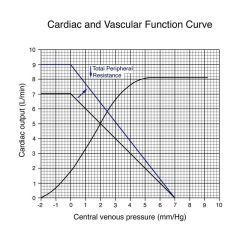
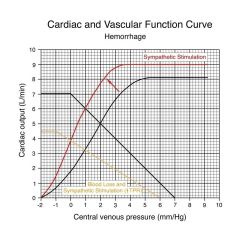
Decrease in filling pressure from 7 to 6 due to blood loss; resulted in increased sympathetic stimulation pushing curve up to left; increase in total peripheral resistance which changed shape of vascular function curve; now we function where golden and red line cross, right at 0 VP, CO = 3.8
Mistake: central venous pressure should flatten and go straight across at central venous pressure of 0 |
|
|
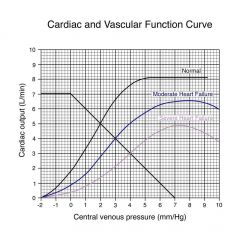
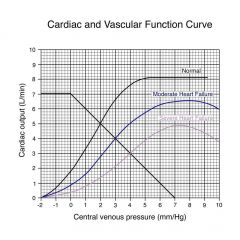
Even though we have the ability to stimulate the heart through sympathetic system, the heart can not respond; when this occurs blood pressure decreases
|

