![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
What is the only thing that changes from the arterial end to the venous end of the capillary?
|
Plasma hydrostatic pressure (Pc)
Starts at 40 mmHg, decreases to 10 mmHg |
|
|
Starling Equation
|
Pv = Kf ([Pc-Pi] - [Nc - Ni])
|
|
|
LP Ratio
|
LymphConc /Plasma Conc
|
|
|
Reflection Coefficient
|
RC = 1 - L/P
|
|
|
Increased fluid within the interstitial gel (edema)
|
Fluidin the interstitial gel becomes free and interstitial hydrostatic pressure increases
(sponge getting hypersaturated and not absorbing anymore) |
|
|
What "squeezes" the interstitial gel as we move around
|
Muscle contraction; squeezes excess fluid into lymph (like a sponge)
This is why the interstitial gel is usually a negative value |
|
|
Lymph Flow as a Function of Pressure in the interstitial space
|
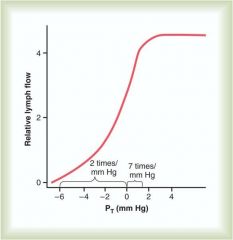
|
|
|
What is located at the junction of arterioles and capillaries?
|
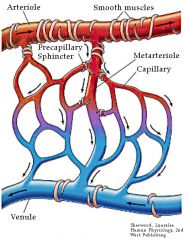
Precapillary Sphincters; smooth muscle band which can help direct blood
|
|
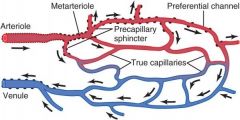
True capillaries
|
Do not have smooth muscle; consist of a single layer of endothelial cells surrounded by a basement membrane
|
|
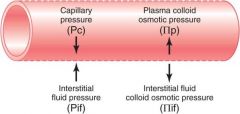
Filtration Forces
|
Pc = capillary hydrostatic pressure (mmHg)
Pi = interstitial hydrostatic pressure (mmHg) Nc = capillary oncotic pressure (mmHg) Ni = interstitial oncotic pressure (mmg)iu |
|
|
An increased Pi indicates what?
|
Absorption/opposition of filtration out of the capillary
(Interstitial pressure is pushing back against the fluid trying to get out) |
|
|
What value is Pi normally?
|
Close to 0 or slight negative (bc of muscle contractions constantly squeezing the fluid out of it)
|
|
|
An increase in Nc indicates what?
|
Opposes filtration; sucks fluid back into the capillary
Could be increased by increases in protein concentrations in the blood (dehydration) |
|
|
What decreases Nc?
|
Decreases in protein concentration; favors filtration/secretion into the interstitial fluid
|
|
|
An increased Ni indicates what?
|
Favors filtration/opposes absorption
Dependent on protein concentration in the interstitial fluid, which is normally low since very little protein is filtered |
|
|
Factors that increase filtration
|
Increase Pc (increased arterial or venous pressure) or Ni
decreased Nc (decreased protein conc in blood) or Pi (inadequate lymphatic function) |
|
|
At the arteriolar end of a cpaillary, Pc is 30 mmHg, Nc is 28 mmHg, Pi is 0 mm Hg and Ni is 4 mm Hg. Will filtratoin or absorption occur?
|
Net pressure = (30-0) - (28-4) mmHg = +6 mmHg
Bc the pressure is positive, filtration will occur |
|
|
At the venous end of the same capillary, Pc has decreased to 16 mm Hg, Nc remains at 28 mm Hg, Pi is 0 mm Hg, and Ni is 4 mm Hg. Will filtration or absorption occur?
|
Net pressure = (16-0) - (28-4) mm Hg = -8 mmHg
Bc the net pressure is negative, absorption will occur |
|
|
Function of Lymph
|
Normally theres a net filtration from capillaries into interstitial gel; excess filtered fluid is returned to circulation via lymph; lymh also returns filtered protein to circulation
|
|
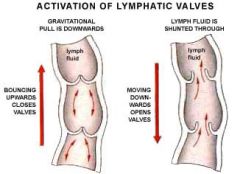
Unidirectional Flow of Lymph
|
One way flap valves permit interstitial fluid but not leave lymph vessels; flow through larger lymphatic vessels is unidirectional and aided by one way valves and skeletal muscle contraction
|
|
|
Edema
|
Volume of interstitial fluid exceeds capacity of lymphatics to return it to circulation; can be caused by excess filtration or blocked lymphatics
|
|

IL-6 and blood cell differentiation
|
Stem cells into myeloid and lymphoid progenitor cells
|
|

IL-7 and blood cell differentiation
|
Stem Cell Differentiation into Lymphoid Progenitor
|
|

IL-15 and blood cell differentiation
|
Natural Killer Cell
|
|
|
Where do B cells rearange their ag receptors and where are they selected?
|

Bone Marrow
|
|
|
where do T cells rearrange their receptors and where are they selected?
|

Thymus
|
|
|
After entering through the blood, where do B cells (expressing CXCR5) migrate to in the lymph node?
|
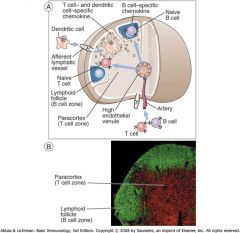
LN Follicles
|
|
|
After entering through the blood, where do T cells (expressing CXCR7) migrate to in the lymph node? What about DC cells?
|
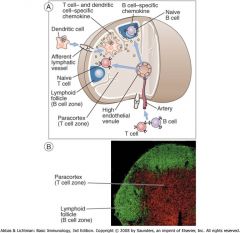
Paracortex
|
|
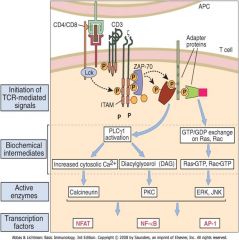
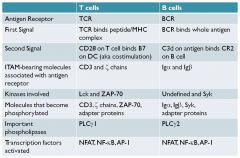
T Cell Activation
|
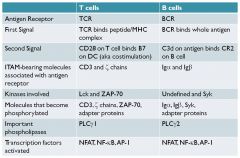
NFAT = nuclear factor of activated T cells
NF-kB AP-1 |
|
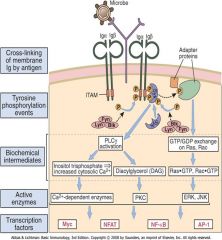
B Cell Activation
|
|
|
|
Function of IL-2
|
causes CD4+ TH cell proliferation
|
|
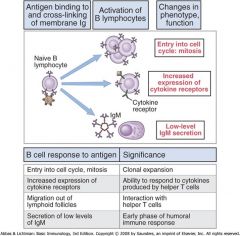
B cell Proliferation
|
Upregulated MHC II; express B7 to interact w/ TH cells; secrete low levels of IgM
|
|
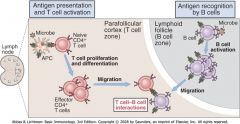
Activated B & T cell Interactions
T: reduce CCR7 expression, increase CXCR5 expression; migrate toward LN follicle B: reduce CXCR5, increase CCR7; migrate towards LN paracortex; they meet at edge of the follicle |

CD40L (T): CD40(B) interaction + cytokines (T) stimulate B cell proliferation
|
|
|
Why do lymph nodes swell?
|

Germinal Center Reactions
|
|

Germinal Center anatomy
|
Mantle Zone: resting B cells that did not bind antigens from current infection
Dark zone: rapid B cell proliferation Light zone: B cells compete to bind to follicular dendritic cells |
|
|
Describe the normal B cell antigen response
|

|
|
|
What is the difference in specificity and Ig isotype of a reactive lymph node and lymphoma?
|
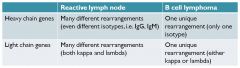
|

