![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
Crew Cut Appearance
|
Beta Thalassemia Major;
|
|
|
Beta Thalassemia Major
|
B chain is absent -> severe anemia requiring blood transfusion (due to secondary hemochromatosis)
Marrow expansion (crew ut on skull x-ray) -> skeletal deformities; chipmunk facies |
|
|
Beta Thalassemia Minor
|
B chain is underproduced, usually asymptomatic, diagnosis onfirmed by increased HbA2
|
|
|
Hydrops Fetalis
|
Deletion o fall 4 alpha globin genes (alpha-thalassemia); hemoglobin Barts (Excess gamma globin chains form tetramers)
|
|
Paroxysmal Nocturnal Hemoglobinuria
|
Mutation in PIGA -> GPI linked complement regulator proteins deficient -> nocturnal red cell lysis due to increased complement activity secondary to decrease in pH during sleep
|
|
|
Classic paroxysmal nocturnal hemoglobinuria presentation
|
episodic red/brown urine (due to hemosiderinuria) = iron deficiency ; prothrombotic state (leading cause of death in those w/ PNH)
|
|
|
Immunohemolytic Anemia
|
Antibodies lead to premature destruction of RBC
|
|
|
Direct Antiglobulin Test (direct Coombs test)
|
For immunohemolytic annemia;
Pts red cells mixed w/ serum containing antibodies that target human immunoglobulin or complement; if ig/complemtn are present = agglutination |
|
|
Indirect Antiglobulin Test (indirect Coombs test)
|
Pt serum mixed w/ rbc w/ known antigens; if ab present for given antigen agglutation occurs
|
|
|
Warm Autoimmune Hemolytic Anemia
|
IgG Ab that do NOT fix complement and are active at 37C
|
|
|
Cold Autoimmune Hemolytic Anemia
|
IgM antibodies that agglutinate red blood cells at low temperatures (below 30C); happens in periphery (fingers, toes, nose)
IgM binding fixes complement |
|
|
Tx for autoimmune hemolytic anemia?
|
Steroids; splenectomy; immunosuppresive therapy
|
|
|
Paroxysmal Cold Hemoglobinuria (Cold Hemolysin Hemolytic Anemia)
|
IgG autoantibodies bind the P blood group ag in the cooler regions of the body; complemt mediated hemolysis occurs when circulation reaches warmer regions; possibly fatal intravascular hemolysis
|
|
|
Drug Induced Immune Hemolytic Anemia; Drug Absorption Mechanism
|
The drug binds to the red blood cell membrane and the antibody attaches to the drug without interacting with the erythrocyte
An example is penicillin |
|
|
Drug Induced Immune Hemolytic Anemia; Immune Complex Mechanism
|
The antibody reacts with new antigenic sites created by the combination of the drug and the membrane
An example is quinidine |
|
|
Drug Induced Immune Hemolytic Anemia; Autoimmune Mechanism
|
Antibodies bind to the red cell membrane in a manner indistinguishable from autoimmune hemolytic anemia
An example is alpha methyl dopa |
|
|
Hemolytic Anemias Resulting from Trauma to RBC
|
Cardiac Valve Protheses (turbulent flow = shear forces)
Vessel narrowing due to fibrin deposition = shear stresses/cell damage Peripheral blood smear findings = schistocytes (helmet cells, triangle cells) |
|
|
How to differentiate between megaloblastic anemia caused by folate or B12 deficiency?
|
Increased homocysteine but with ELEVATED methylamalonic acid in B12 deficiency (normal in folate deficiency)
|
|
|
Megaloblastic Anemia
|
Impaired DNA synthesis secondary to inadequate B12 or folate levels (thymidine) -> maturation of nuclesy delayed relative to maturation of cytoplasm
Morphologic finding: hypersegmented neutrophils) |
|
|
Pernicious Anemia
|
Type of megaloblastic anemia secondary to autoimmune gastritis; vitamin B12 deficiency due to impairment of intrinsic factor production)
|
|
|
Transferrin
|
Iron binding protein which transports iron in the serum; delivers iron to cells
|
|
|
Ferritin
|
Protein iron complex in liver, spleen, bone marrow, skeletal muscle
Used as a marker for body iron stores |
|
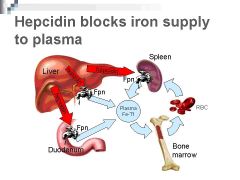
Hepcidin
|
Peptide that regulates iron absorption; inhibits transfer of iron from enterocytes to the plasma; if the body has adequate iron stores elevated hepcidin levels inhibit iron absorption into the blood (if iron stores low, hepcidin levels decrease and iron absorption unimpaired)
|
|
|
Ascorbic Acid
|
Enhances absorption of inorganic iron
|
|
|
Tannates (tea)
|
Impairs absorption of inorganic iron
|
|
|
Most common causes of iron deficiency
|
Adult men/postmenopausal women: GI blood loss until proven otherwise
|
|
|
Anemia of Chronic Disease (ACD)
|
Inflammation -> increase hepcidin -> decreases absorbed iron
|
|
|
Iron Deficiency Anemia (Microcytic, Hypochromic)
|
Decreased iron due to chronic bleeding, malnutrition/absorption disorders or increased demand (pregnancy) -> decreased heme synthesis
|
|
|
Plummer Vision Syndrome
|
Esophageal webs; microcytic hypochromic anemia; atrophic glossitis
|
|
|
Pica
|
Desire to consume items such as clay or flour due to iron deficiency
|
|

Fanconi Anemia
|
Inherited defect in DNA repair; aplastic anemia
Upper extremity deformities w/ radius, wrist and thumb abnormalities most prevalent |
|
|
Aplastic Anemia Pathogenesis
|
Pancytopenia w/ severe anemia, neutropenia and thromboytopenia; normal cell morphology but hypocellular bone marrow w/ fatty infiltration
|
|
|
Aplastic Anemia Causes
|
Failure or desturction of myeloid stem cells due to radiation/drugs, viral agents, fanconi's anemia, idiopathic
|
|
|
Aplastic Anemia bone marrow histology
|
Diminished hematopoietic cells; fat cells, fibrous stroma, lymphocytes/plasma cells (marrow becomes mostly fatty)
|
|
|
Pure Red Cell Aplasia
|
Marrow disorder resulting in suppression of erythroid progenitors; often secondary to thymoma
|
|
Myelophthisic Anemia
|
Space occupying lesion destroy marrow architecture/depress productive capacity; most common cause is metastatic cancer
|
|
|
Chronic Renal Failure w/ Secondary Anemia
|
Decreased synthesis of erythropoietin
|
|
|
Hepatocellular Liver disease w/ secondary anemia
|
Decreased marrow function; erythroid precursors primarily effected
|
|
|
POlycythemia
|
Elevated hematocrit associated w/ increased hemoglobin levels
|
|
|
Relative polycythemia
|
Decreased plasma volume associated w/ dehydration
|
|
|
Stress Polycythemia
|
Gaisbock Syndrome; idiopathic
|
|
|
Primary Absolute Polycythemia
|
Increased hematocrit due to myeloid neoplasm (polycythemia vera); RBC precursors proliferate in an erythropoietin independent fashion
|
|
|
Secondary Appropriate Polycythemia
|
Increased erythropoietein stimulate red cell progenitors (may be compensatory or pathologic)
|
|
|
Reticulocyte Production Index (RPI)
|
MEasure of the degree of reticulocytosis
RPI <2 = inadequate bone marrow response RPI > 2 = appropriate bone marrow response for the degree of anemia |
|
|
Laboratory Tests which indicate hemolysis
|
1. Decreased haptoglobin
2. Elevated bilirubin 3. Elevated LDH 4. Presence of urine hemoglobin or hemosiderin 5. Plasma hemoglobin |
|
|
Why would an RPI be greater than 2?
|
Acute blood loss; hemolysis
|
|
|
Causes of microcytic anemia
|
Iron deficiency anemia; anemia of chronic disease; thalassemia; sideroblastic anemia
|
|
|
Sideroblastic Anemia
|
Bone marrow produces ringed sideroblasts rather than healthy bone marrow
|

