![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
96 Cards in this Set
- Front
- Back
|
What are 3 characteristics that are useful on plain film to determine the type of heart disease
|
cyanosis
pulmonary vascularity cardiac size |
|
|
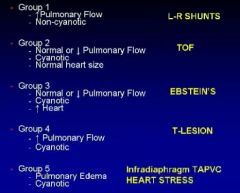
What are the 5 groups of congenital cardiac disease
|
|
|
|
What are group 1 CHD
|
L to R shunt
|
|
|
What are the findings in a group 1 congenital defect
|
increased pulm vasc
non-cyanotic |
|
|
What is an example of a group 2 defect
|
TOF
|
|
|
What are the findings in group 2 defect
|
normal/decreased pulm flow
cyanotic normal heart size |
|
|
Are group 2 defects cyanotic with a normal heart size
|
yes and they have normal flow
(might look normal but are cyanotic) |
|
|
What are the findings of a group 3 congenital heart disease
|
normal or decreased pulm flow
cyanotic large heart |
|
|
What is the main difference between group 2 and 3
|
group 3 has a big heart (both are cyanotic with normal/decreased pulm flow)
|
|
|
What is an example of a group 3 CHD
|
ebsteins
|
|
|
What are the findings in a group 4 CHD
|
increased pulm flow
cyanotic |
|
|
What is the difference between group 2 and 4
|
increased flow
|
|
|
What is an example of a group 4 defect
|
T-lesion
|
|
|
What are the findings in a group 5 defect
|
pulmonary edema
cyanotic |
|
|
What is the difference between group 4 and 5
|
more pulmonary overload?
|
|
|
What is an example of a group 5 defect
|
infradiaphragmatic TAPVC and Heart stress
|
|
|
What is the most common group
|
group 1
|
|
|
Which group has all the right to left shunts
|
group 1
|
|
|
What do group 2 and 3 have in common
|
decreased or normal pulm flow and cyanotic
|
|
|
Is group 5 comprised of rare diseases
|
yes
|
|
|
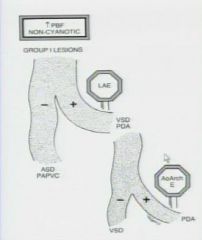
What is the rule for group 1 lesions
|
|
|
|
What do if a pt is group 1 and has LAE
|
then its VSD or PDA and you must determine if the pt has Aortic enlargement if not then it is VSD
|
|
|
What if a pt has no LAE
|
then it is ASD or PAPVC
|
|
|
What group is a non-cyanotic pt with increased pulmonary vascularity
|
group 1
|
|
|
What group is a pt with cyanosis and normal or decreased pulmonary vascularity
|
group 2
|
|
|
What are some plain film findings of TOF
|
diminshed pulmonary contour
boot shaped heart right aortic arch |
|
|
If a pt is group 2 what must the patient be
|
TOF
|
|
|
A pt with normal vascularity, cyanotic and enlarged heart
|
group 3
|
|
|
What is the most common lesion in a group 3
|
ebsteins anomaly
|
|
|
What is the ddx of a group 3 lesion
|
tricuspid atresia with restricted ASD
pulmonic stenosis with intact ventricular septum tricuspid regurgitation of newborn |
|
|
If there is diminished pulmonary flow what group must it be
|
2 or 3
|
|
|
Does ebsteins anomaly have an increased heart size
|
yes
|
|
|
If you see increased pulmonary vascularity in a patient with cyanosis what group
|
group 4
|
|
|
If there is a group 4 lesion what must you do first
|
look at the superior mediastinum and determine if it is narrow (if narrow then TGA)
|
|
|
What are the findings of TGA
|
increased pulmonary flow
cyanotic Narrow heart base |
|
|
What is the ddx of group 4
|
TGA, Truncus, TAPVC, Ticuspid atresia, Tingle Ventricle, DORV and DOLV
|
|
|
what are the Group 4 T lesions
5 |
TGA, Truncus, TAPVC, Tricuspid, Tingle Ventricle
|
|
|
What is DORV and DOLV
|
double outlet right ventricle
double outlet left ventricle |
|
|
What if the superior mediastinum is enlarged in a group 4 lesion
|
TAPVC supracardiac type
|
|
|
What are the findings of TAPVC
|
increased pulmonary flow
cyanotic increased size of superior mediastinum |
|
|
What is the MC group 5 lesion (although rare)
|
pulmonary edema (more severe)
cyanotic |
|
|
What are the findings of TAPVC infradiaphragmatic type
|
normal heart and superior mediastinum
cyanotic pulmonary edema |
|
|
What is the ddx of group 5 lesions
|
reversible heart stress
structual |
|
|
What are 7 causes of reversible heart disease
|
severe anemia
asphyxia hypocalcemia hypoglicemia arrhythmia hypervolemia myocarditis |
|
|
What are the structual causes of group 5 lesions
|
coarctation
|
|
|
What group are severe anemia
asphyxia hypocalcemia hypoglicemia arrhythmia hypervolemia myocarditis located in |
group 5
|
|
|
What are the 4 most common clinical indications of MR in adults with chd
|
post op TOF
Occult L-R shunt Post op complex CHD Coronary artery anomaly |
|
|
What are the findings of TOF
|
VSD
overriding aorta pulmonary stenosis RV Hypertrophy |
|
|
What is a severe variant of TOF
|
pulmonary atresia with VSD
|
|
|
What percent of TOF pts have right aortic arch
|
25%
|
|
|
What type of VSD is seen in TOF
|
perimembranous
|
|
|
Is the aorta overriding
|
yes, both blood from the left and right ventricle can enter the aorta (because there is a VSD)
|
|
|
What must be evaluated in pt with post op TOF
|
pulmonary regurgitation
residual stenosis RV volumes and functions |
|
|
What are the residual stenosis that occur in TOF
|
valvular
peripheral |
|
|
What sequences are needed for TOF repair imaging
|
Cine MR (short axis)
Velocity encoded cine MR |
|
|
ELECTRICAL FORCE
|
PUSHES _NOT_ PULLS ELECTRON'S THROUGH CONDUCTING OR SEMI-CONDUCTION MEDIUM
|
|
|
What should you look at on the sagital cine
|
flow jets around the pulmonary artery (look for regurgitation and stenosis of PA)
|
|
|
What two images are used to get Blood flow
|
magnitude and flow and these are multiplied
|
|
|
What color will the flow be during systole
|
postitive (it will turn dark during systole if it reverses)
|
|
|
What must be compared in all TOF post op pts
|
the flow of the right and left pulmonary arteries
|
|
|
What are the normal flow numbers of the PA
|
55% to left
45% to the right |
|
|
What are some occult L-R shunts
|
supracristal VSD
sinus venosus ASD PAPV (RUL vein to the SVC or RA) Hypogenetic lung syndrome (scimitar syndrome) |
|
|
What is the causes of a PAPVC that may be occult
|
RUL vein to SVC or RA
|
|
|
What is scimitar syndrome (hypogenetic lung syndrome)
|
is characterised by a hypoplastic lung that is drained by an anomalous vein into the systemic venous system.
|
|
|
What is scimitar syndrome a combination of
|
It is essentially a combination of pulmonary hypoplasia and partial anomalous pulmonary venous return (PAPVR).
|
|
|
What side does scimitar syndrome most commonly occur
|
the right side
|
|
|
Where does the anomalous vein most commonly drain into
|
The anomalous vein usually drains into
IVC : most common right atrium or portal vein |
|
|
What is the arterial supply of the lung
|
The lung is frequently perfused by the aorta, but the bronchial tree is still connected and thus the lung is not sequestered.
|
|
|
What are the MR findings of scimitar syndrome
|
CXR findings are that of a small lung with ipsilateral mediastinal shift, and in one third of cases the anomalous draining vein may be seen as a tubular structure paralleling the right heart border in the shape of a Turkish sword (“scimitar”). The right heart border maybe blurred.
|
|
|
Describe a supracristal VSD
|
The location of the supracristal VSD, with its close proximity to the aortic root, accounts for the common development of aortic insufficiency with this defect. Left-to-right shunting of blood through the defect is believed to progressively pull aortic valve tissue (especially the right coronary cusp) through a Venturi effect
|
|
|
What are the complications assoicated with supracristal VSD
|
Patients with small, isolated supracristal VSDs may have no symptoms or signs of congestive failure such as might be observed with a large shunt. Progressive aortic insufficiency may develop late in the first decade of life. Larger defects of the outlet septum frequently are associated with forms of aortic outflow obstruction (eg, coarctation, interrupted aortic arch). In such cases, symptoms of congestive heart failure and possible circulatory collapse appear early.
Patients with larger, isolated supracristal VSDs may develop congestive heart failure early in infancy due to a large left-to-right shunt. |
|
|
Is it possible to have bilateral PAPVC
|
yes (the right side might connect to a vertical vein from the left BCV to the left atrium)
|
|
|
What do you see in scimitar vein syndrome on plain film
|
a curve-linear opacity leading from the RU chest to below the diaphragm
-Mediastinum deviated to the right (hypoplastic right lung) -Elevated right hemidiaphragm (hypoplastic right lung) |
|
|
Where is the sinus Venosus ASD located
|
between the superior vena cava and the left atrium
|
|
|
What type of ASD is easily missed on echocardiography
|
sinus venosus
|
|
|
What percent of pt patients with sinus venosus have an associated PAPVC
|
95%
|
|
|
Where is the associated PAPVC of sinus venosus located
|
RUL
|
|
|
What are the two surgeries for D-transpostition
|
arterial switch
atrial switch via baffles |
|
|
What is the main complications of an arterial switch
|
pulmonary stenosis
|
|
|
What are the main complications of atrial switch
4 |
decreased RV function
shunts stenosis of baffles clots |
|
|
Is the right ventricle still connected to the aorta after a baffle procedure for TGA
|
yes, a baffle is made so the blood from the left atrium goes to the right ventricle
|
|
|
Where is the aorta in relation to the pulmmonary artery in TGA
|
anterior
|
|
|
What causes the stenosis in the arterial switch for TGA
|
the pulmonary artery is moved to its normal posion anteriorly and this causes streching of the pulmonary artery leading to stenosis
|
|
|
Where is the aorta in relation to the pulmonary artery in L-TGA (corrected)
|
it is also anterior and to the left (hence L-TGA), but in this the left atrium is connected to the right ventricle (sort of what the baffle procedure does) so it is congenitally corrected
|
|
|
How would you describe the morphology of the infundibulum of the right ventricle
|
complete circle muscular infundibulum (see this on axial and wont be seen on the left) and the left is fibrous
|
|
|
How would you describe the septum of the right and left ventricles
|
right is irregular
left is smooth |
|
|
What is the MC coronary atery origin anomaly
|
MPA
|
|
|
What are two ectopic origins of coronary arteries
|
MPA
ectopic aorta |
|
|
What are 3 anamolous courses of the coronary arteries
|
anterior to the RVOT
interarterial (main pulm artery and aorta) retrocardiac |
|
|
What type of anomalous coronary course is associated with sudden death
|
interarterial
|
|
|
What is ALCAPA
|
anomalous left coronary artery for the pulmonary artery
|
|
|
What is myocardial bridging
|
the coronary artery within the myocardium
|
|
|
Where is Myocardial bridging most frequently seen.
|
Myocardial bridging is most commonly observed of the LAD
|
|
|
What is more important in myocardial bridging the depth or the length
|
The depth of the vessel under the myocardium is more important that the lenght of the myocardial bridging.
|
|
|
What is interarterial anomalous coronary
|
There is an anomalous origin of the LCA from the right sinus of Valsalva and the LCA courses between the aorta and pulmonary artery.
This interarterial course can lead to compression of the LCA (yellow arrows) resulting in myocardial ischemia. |
|
|
What percent of pt with ALCAPA precent with CHF in the 1st 2 MOL
|
Approximately 85% of patients present with clinical symptoms of CHF within the first 1-2 months of life. (bc of MI's)
|

