![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
Questions on a diabetes history?
|
Autonomic complications
Microvascular complications: nephropathy, retinopathy, neuropathy. Macrovascular complications: CVS, CVD, PVD Family history Treatment Compliance Hospital admissions Specialist appointments |
|
|
Autonomic complications of diabetes?
|
Erectile dysfunction.
Gastroparesis - do you feel full easily after a meal? do you vomit? Have you had any formal imaging for gastro? Postural hypotension - when you stand up do you feel dizzy or unwell? |
|
|
What infections are particularly common in girls with type 1 diabetes?
|
Thrush (vaginal candidiasis)
|
|
|
What is the pathogenesis of type 1a?
|
Autoimmune destruction of the insulin producing beta cells.
|
|
|
What is the pathogeneiss of type 1b?
|
Non autoimmune.
|
|
|
What are some of the factors in the causation of type 1 dibaetes?
|
Closely associated with HLA genes.
Lifelong risk of type 1 dibaetes is increased in close relatives of a patient with type 1 symptoms. |
|
|
What environmental factors are linked in the causation of type 1 diabetes?
|
Perinatal: increased birth weight, maternal age.
Viruses Diet: cow's milk and cereal at early age thought to be implicated. |
|
|
What autoimmune disorders are associated with type 1 diabetes?
|
Hypothyroidism
Coeliac disease Addison's Vitiligo Autoimmune polyglandular syndromes Pernicious anaemia |
|
|
What is the fasting plasma glucose to diagnose diabetes?
|
> 7.0 mmol/L
|
|
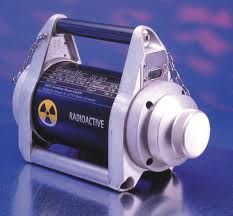
(a) Outline the principles of gamma radiography.
|
Gamma radiography uses the transmission of gamma rays from a sealed ionising radiation source through a test object on to a film placed on the opposite side. The film records the intensity of the radiation received and since cracks and flaws are hollow, a greater intensity of rays pass onto the film and the defects are shown up as darker regions.
|
|
|
What is the random plasma glucose needed to diagnose diabetes?
|
11.1 mmol/L
|
|
|
What is an additional test to help diagnose type 1 diabetes?
|
Islet cell antibodies
GAD Insulin antibodies |
|
|
What other investigations should be done in a suspected type one DM?
|
C-peptide (low in type 1)
Insulin levels |
|
|
What is impaired fasting glucose?
|
5.6 - 6.9
|
|
|
What is impaired glucose tolerance?
|
7.8 - 11.0
|
|
|
What HbA1c would diagnose diabetes?
|
< 6.5%
|
|
|
What is HbA1c?
|
Glycated haemoglobin. Gives an idea of the average blood sugar of last 3 months.
|
|
|
How can anaemia skew the HbA1c?
|
It can make it falsely low.
|
|
|
Name all the common symptoms of diabetes.
|
Polyuria
Polydipsia Weight loss Infection Visual blurring DKA Hyperosmolar hyperglycaemia state Asymptomatic |
|
|
Which type is HHS more commonly seen in?
|
Type II more so than type I.
|
|
|
Which type is more likely to have ketoacidosis?
|
Type I diabetes.
|
|
|
What are some features of non-proliferative retinopathy?
|
Blot haemorrhages
Microaneurysms Cotton wool spots |
|
|
What is the problem with proliferative nephropathy?
|
Proliferative - new unstable blood vessels can develop so need to laser blood vessels.
|
|
|
What is the concern with diabetic nephropathy?
|
Can lead to renal failure and diiabetic nephropathy.
|
|
|
Risk factors to develop nephropathy in a diabeic?
|
Famiily history
Smoking Hypertension Poor glycaemic control |
|
|
Which medications are good to treat nephropathy?
|
ACE-Inhibitor
or ARB |
|
|
What causes neuropathy?
|
Microvascular disease affecting the small nurtient vessels that supply peripheral nerves.
|
|
|
What is the first-line for diabetic pain?
|
Amytryptilline
GaBA pentin Sodium valproate |
|
|
What investigations should you do in a DKA?
|
Blood gasses
BSL Ketones FBE UEC Consider LFT Lipase CRP Blood cultures CXR/AXR |
|
|
Why might lipase be raised in DKA?
|
Not diagnostic of pancreatitis.
It is just raised sometimes. |
|
|
When do you cease an insulin infusion in a DKA patient?
|
Ketones going down
pH going up |
|
|
When is dextrose started with the insulin infusion in a diabetic patient?
|
When BSL < 15 can give 10% dextrose.
|
|
|
What is the problem with potassium when giving insulin to a DKA?
|
giving insulin can drive potassium into the cell
|
|
|
What are the three components to DKA?
|
Anion gap acidosis
Hyperglycaemia Ketoacidosis |
|
|
How is the anion gap calculated?
|
Na - (Hco3 + Cl)
|
|
|
How do you get DKA?
|
Breakdown of adipose tissue
Causes free fatty acids Converted in the liver into ketone bodies The hyperglycaemia causes dehydration because of osmotic diuresis. |
|
|
What are the clinical features of DKA?
|
Polyuria
Weight loss blurred vision n + v abdominal pain hyperventilation confusion |
|
|
What are precipitating factors for DKA?
|
Infection (pneumonia or UTI)
discontinuation or inadequate insulin therapy acute major illnesses such as MI new onset type I poor compliance with insulin malfunction of insulin pump |
|
|
How to treat DKA?
|
Fluid replacement (normal saline)
IV insulin measure serum glucose hourly until stable if initial serum potassium below 3.3 mmol/L make sure you give aggressive fluid and potassium replacement prior to treatment with insulin |
|
|
What are the features of hyperosmolar hyperglycaemic state?
|
Elderly patients
Develops gradually Usually not acidotic or ketotic Profoundly dehydration, hypotension, tachycardia, altered mental status Marked hyperglycaemia, hyperosmolality Volume depletion and hyperglycaemia are the main features Treatment is via volume replacement and insulin therapy |
|
|
What is lantus?
|
Recombinant human insulin analogue
Basal long-acting insulin Usually once-daily subcut, but often BD. usually given in morning or night |
|
|
What is detemir? (levemir)
|
Basal long acting insulin
twice daily subcut peaks 3 - 14 hours, duration up to 24 hours only approved for type 1 diabetes |
|
|
What are the benefits of CSII?
|
Flexibility
Better control Less injections Cost - only available for type 1 diabetes with private health insurance - 8000 to 10000 dollars for a pump |
|
|
What is DAFNE?
|
Diet
Adjusted For Normal Eating - Run by diabetic educators to calculate how much insulin is needed for how many grams of carbohydrates. |
|
|
Where are common injection sites?
|
Subcutaneous: buttocks, abdomen, upper thigh, arm.
|
|
|
What can repeated insulin injections cause?
|
Lipohypertrophy.
Patients like it because it is painless but very little insulin is absorbed. |

