![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
122 Cards in this Set
- Front
- Back
|
(05-April) (07-April) (11-September-Bank)
The carotid sinus derives its nerve supply from the A. vagus nerve B. glossopharyngeal nerve C. ansa cervicalis (hypoglossi) D. middle cervical ganglion E. stellate ganglion |
B
Glossopharyngeal supplies sensory for - Pharynx - Tonsils - Posterior 1/3 tongue - Carotid sinus and carotid body Glossopharyngeal supplies motor for - Stylopharyngeus muscle - Secretomotor fibres for parotid gland |
|
|
(05-April) (05-July) (06-March) (11-September-Bank)
The muscles of the upper eyelid receive a somatic nerve supply from the A. oculomotor nerve and a parasympathetic supply from the superior vagus nerve B. oculomotor nerve and a sympathetic supply from the superior cervical ganglion C. ophthalmic division of the trigeminal nerve and a parasympathetic supply from the superior vagus nerve D. ophthalmic division of the trigeminal nerve and a sympathetic supply from the superior cervical ganglion E. ophthalmic division of the facial nerve only |
B
- Occulomotor nerve supplies superior rectus muscle and levator palpebrae superioris - (also carries fibres from the superior cervical ganglion which is SNS) |
|
|
(07-April) (07-July) (10-March-Bank) (10-August-Bank) (11-September-Bank)
Movement(s) produced by the motor components of the C67 nerve roots is/ are A. elbow flexion B. elbow pronation and supination C. finger flexion and extension D. shoulder abduction and lateral rotation E. wrist flexion and extension |
E
- C6-7 flex and extend wrist - C5-6 pick up sticks (biceps jerk) - C7-8 shut the gate (triceps jerk) - L3-4 kick the door (knee jerk) - S1-2 buckle my shoe (ankle jerk) |
|
|
(07-April) (07-July) (08-April) (10-March-Bank) (10-August-Bank) (11-September-Bank)
The stellate ganglion is located A. anterior to the anterior scalene muscle (scalenus anterior) B. anterior to the dome of the pleura C. anterior to the thoracic duct D. at the level of the body of C6 (6th cervical spine) E. posterior to the brachial plexus sheath |
A
Stellate ganglion at C7 (anterior to scalenus anterior) |
|
|
(07-July) (08-April) (11-September-Bank)
You are asked to see a 60-year-old male 2 days following a cervical laminectomy because he has new neurological symptoms in his right arm. The surgical team think these may be due to poor patient positioning. The sign that would most help differentiate a C8-Tl nerve root injury from an ulnar nerve injury is A. loss of sensation in the index finger B. loss of sensation in the little finger C. weakness of the abductor digiti minimi muscle D. weakness of the abductor pollicis brevis muscle E. weakness of the first dorsal interosseous muscle |
D
T1 and ulnar have similar sensory and motor distribution - All muscles of hand supplied by ulnar - Except LOAF muscles (supplied by median nerve) - Ulnar nerve injury results in claw hand (Meat) LOAF: - Lateral two lumbricals - Opponens pollicis - Abductor pollicis brevis - Flexor pollicis brevis |
|
|
(08-August-BANK) (11-September-Bank)
The left recurrent laryngeal nerve A. hooks around the arch of the aorta anterior to the attachment of the ligamentum arteriosum B. passes under cover of the lower border of the interior constrictor muscle before entering the larynx C. supplies the cricothyroid muscle D. supplies sensation to the whole of the laryngeal mucosa on the left side E. contains motor fibres derived from the spinal root of the accessory nerve |
B
A – False. Left RLN loops under the arch of aorta posterior to ligamentum arteriosum before ascending. B – True. Passes below the inferior constrictor muscle to innervate intrinsic muscles of the larynx C – False. RLN supplies all laryngeal muscles except the cricothyroid muscle (supplied by the external branch of the superior laryngeal nerve) D – False. Sensory innervation below the cords is from the RLN (sensory innervation above the cords is from the superior laryngeal nerve) E – False. Contains motor fibres derived from the vagus nerve |
|
|
(10-March-Bank) (10-August-Bank) (11-September-Bank)
Interscalene block, patient hiccups...where do you redirect your needle? A. Anterior B. Posterior C. Caudal D. Cranial E. Superficial |
B
Hiccup = phrenic nerve stimulation (occurs when needle too anterior) hence redirect posterior |
|
|
(10-August-Bank) (11-September-Bank)
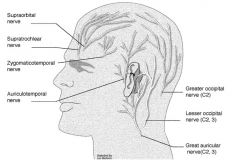
Nerve block for anaesthesia over anterior 2/3 of ear? A. C2 B. Mandibular nerve C. Maxillary nerve D. Ophthalmic nerve E. Vagus |
Trigeminal nerve has 3 branches
- Ophthalmic (sensory to eyes, nasal mucosa, eyelids, eyebrow, forehead, nose) - Maxillary (sensory to maxilla, nasal cavity, sinuses, palate, mid-face) - Mandibular (motor and sensory). Posterior division gives of auriculotemporal nerve, lingual nerve and inferior alveolar nerve Auriculotemporal nerve supplies anterosuperior and anteromedial aspect of the auricle |
|
|
(10-August-Bank) (11-September-Bank)
LUSCS for failure to progress. Spinal is inserted uneventfully. Next day the patient has foot drop. The most likely cause is? A. epidural haematoma B. lumbosacral palsy C. sciatic nerve palsy D. common peroneal palsy E. |
B
- Foot drop occurs most commonly from lumbosacral trunk compression (from baby’s head or forceps compressing nerve against sacrum) - Less commonly can occur with common peroneal nerve palsy from prolonged lithotomy |
|
|
(11-September-Bank)
Post epidural and LSCS, the next day patient have persistent paraesthesia anterior thigh. What other injuries would indicate more of nerve roots instead of peripheral nerve injuries A. Weakness on hip flexion and thigh adduction B. Weakness on knee flexion and plantar flexion C. Urinary incontinence D. Foot drop |
C
Urinary incontinence should not occur with peripheral nerve injuries Meralgia paresthetica - Due to compression of lateral femoral cutaneous nerve - Susceptible due to course from lumbosacral plexus via abdominal cavity to under inguinal ligament (esp. in obstetrics) - Presents as burning pain, paresthesia and hyperesthesia over upper outer thigh exacerbated by valsalva (increases intra-abdominal pressure) - Lower neurological examination should otherwise be normal Lumbosacral nerve roots: Sensory fields between roots have considerable overlap - Areas exclusively served by individual roots = autonomous zones - Anterior thigh = L2 & L3 - Medial calf = L4 - Dorsum of foot = L5 - Sole of foot = S1 Motor involvement - L1 = hip flexion - L2 L3 L4 = knee extension - L5 = ankle dorsiflexion (i.e. foot drop), toe extension - S1 = weak hip extension - S2 S3 S4 = urinary and faecal incontinence Foot drop is also commonly associated with common peroneal nerve compression (susceptible with obstetric stirrups) |
|
|
(11-September-Bank)
Compared to retrobulbar block, peribulbar block is associated with A. More bleeding B. More risk to optic nerve C. More akinetic eye D. Less block to orbicularis oculi |
? All false
Cochrane states both blocks very similarly effective and with similarly low rates of complications Retrobulbar block: LA deposited inside muscle cone - Blocks ciliary nerves, ciliary ganglion, CN II III VI Complications - Allergy - Retrobulbar haemorrhage (results in motor block, closing upper lid, sudden rise in IOP causing proptosis) (can lead to central retinal artery occlusion and stimulation of oculocardiac reflex - bradycardia) - Central retinal artery occlusion due to LA injected into dura - Subconjunctival oedema (chemosis) - Perforation of globe (pain, sudden loss vision, hypotonic, poor red reflex) - Optic nerve atrophy (partial or complete visual loss) Peribulbar block: LA deposited above and below orbit (into orbicularis oculi muscle) - Blocks ciliary nerves, CN III VI Advantage - Less potential for intraocular or intradural injection (injection outside cone) - Less potential for haemorrhage and direct injury to optic nerve - No difference in effectiveness, complete akinesia or requirement for top up LA - Easier to perform Disadvantage - More difficult to get complete dense block - Subconjunctival oedema more common - Periorbital ecchymoses - LA can spread to contralateral eye |
|
|
(11-September-Bank)
Lumbosacral nerve does not supply: A. Subcostal nerve B. Ilioinguinal n C. Iliohypogastric n D. Femoral n E. Genitofemoral n (?) |
A
Subcostal nerve (anterior division of 12th thoracic nerve) |
|
|
(11-September-Bank)
When stimulating the ulnar nerve with a nerve stimulator, which muscle do you see twitch? A. opponens abducens B. abductor pollicis brevis C. adductor pollicis brevis D. extensor pollicis E. flexor pollicis brevis |
C
Ulnar stimulation monitors adductor pollicis brevis (facial stimulation monitors orbicularis oculi) |
|
|
(08-April) (11-March-Bank)
When performing regional anaesthesia for eye surgery, needle damage to the globe of the eye is more common with: A. a globe axial length of less than 25 mm B. patients aged less than 45 years C. peribulbar block using the inferotemporal approach D. peribulbar block using the medial canthus approach E. sub-Tenon block |
C
Most common approach is inferolateral (followed by medial canthus) Peribulbar block (inferolateral) - Iv access & monitoring - Minimal sedation (MDZ 1mg or PPF 20mg + Fentanyl 50mcg) - LA to conjunctiva (proxymetacaine 0.5%) - Patient supine and looking straight ahead - Palpate groove in inferior orbital rim (lateral 1/3) - Insert 25G 25mm needle (transcutaneous or transconjunctival with retraction of lower lid, perpendicular, 1mm lateral 1mm above rim) with 10ml syringe - Advance till hub level with iris (may need slight superomedial angle if hit bone) (observe for rotation of eye suggesting contact with sclera) - Aspirate and inject 6-8ml LA (palpate with other hand, stop if globe becomes tense/proptosed or upper lid falls = retrobulbar hence requiring lower volume) - Digital massage/Honan balloon to spread LA and normalise IOP - If top up required do medial canthus Contraindications peribulbar: - INR > 2 (if high, do sub-tenon or GA) - Axial length > 26mm (suggests sausage shaped eye increasing risk perforation) (if so do sub-tenon or GA) - Perforated or infected eye - Unable to lie supine or still Risks: - Globe perforation (<0.1%) - Retrobulbar haemorrhage (0.07%) - Systemic complications (oculocardiac, neurogenic syncope, seizure) |
|
|
(09-August-Bank) (10-March-Bank) (11-March-Bank)
Your patient given thiopentone by mistake has a porphyric (acute intermittent) crisis with abdominal pain and then seizures. What drug is contraindicated? a. Phenytoin b. Morphine |
A
Safe drugs in porphyria - Midazolam, Flumazenil - Propofol - Fentanyl, Alfentanil, Morphine, Naloxone - Suxamethonium, Atracurium (caution), Rocuronium (caution) - Sevoflurane (caution) - Paracetamol, Tramadol (caution), Ibuprofen (Diclofenac only if no alternative) - Dexamethasone, Droperidol, Ondansetron, Metoclopramide (caution) - Penicillin, Cephazolin, Metronidazole (only if no alternative) - Esmolol, Metoprolol, Labetalol, GTN, Adrenaline - Oxytocin - Lignocaine, Bupivacaine Unsafe drugs in porphyria - Thiopentone - Phenytoin - Ergometrine - Ropivacine |
|
|
(10-March-Bank) (11-March-Bank)
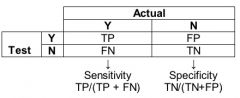
If a test is negative, what proportion will not have the disease: A. Sensitivity B. Specificity C. Positive Predictive Value D. Negative Predictive Value |
D
NPV = True negative rate |
|
|
(11-March-Bank)
The anterior branch of the femoral nerve supplies everything but: A: pectineus B: rectus femoris C: Medial thigh D: anterior thigh E: sartorius |
B
Rectus femoris is supplied by the posterior branch of the femoral nerve Femoral nerve anterior division - Muscular branches to pectineus and to sartorius - Cutaneous branches to: - Intermediate cutaneous nerve of thigh (supplies anterior thigh) - Medial cutaneous nerve of thigh (supplies medial thigh Femoral nerve posterior division - Muscular branches to quadriceps femoris (including rectus femoris) - Cutaneous branch = saphenous nerve (medial knee, leg, ankle and foot) - Articular branches to hip and to knee |
|
|
(11-March-Bank)
During interscalene block placement get medial movement of the scapula. This is secondary to stimulation of: A: long thoracic nerve B: dorsal scapula nerve C: suprascapular nerve D: supraclavicular nerve E: accessory nerve |
E
Spinal accessory nerve supplies trapezius (medial movement of scapula) and SCM - Shrugging indicates needle too posterior to interscalene groove Phrenic nerve supplies diaphragm - Hiccups indicates needle too anterior to interscalene groove |
|
|
(11-March-Bank)
Popliteal block placed from the lateral approach: A: Passes through semimembranosus B: Has eversion of the foot as the end point C: Has increased failure rate compared to a posterior approach D: ? E: Can be performed supine or prone |
C
- A: False. Semimembranosus is a medial muscle (most medial of 3 hamstring muscles) - B: False. End point is of twitches of foot or toes. - Eversion with dorsiflexion indicates common peroneal (is more frequently stimulated as nerve is more lateral) - Inversion with plantar flexion indicates tibial nerve - Both are acceptable if large volumes are used - Tibial signs (inversion and plantar flexion) = end point with single shot - C: True. Posterior approach has lower failure rate (0% compared with 5%) - E: False. Position supine with leg on rest (achilles tendon off the rest to allow recognition of foot movement) - Posterior approach requires prone patient or in lithotomy |
|
|
(11-March-Bank)
During scoliosis surgery with monitoring of somatosensory evoked potentials, which tract are they mainly monitoring? A: Dorsal column B: Spinothalamic tract C: Lateral Corticospinal tract D: Cerebrospinal tract E: Anterior horn cells |
A
SSEP monitors dorsal columns SSEP (somatosensory evoked potentials) - A peripheral nerve is stimulated then a response in an epidural or scalp electrode is looked for - Averaged over 2-3min to eliminate background noise then displayed as voltage vs time (nerve injury = decreased amplitude or increased latency) MEP (motor evoked potentials) - Transcranial electrical impulses stimulate motor cortex then a signal is looked for in epidural electrodes or compound muscle action potentials - More rapidly responding to event than SSEP - Requires MAP > 60mmHg otherwise readings unreliable Anaesthesia and monitoring - Volatiles (20% decrease amplitude), propofol (8% increased latency) and N2O depress SSEP and MEP (Sevo/Remi allows faster wake up and faster neurological assessment but Prop/Remi gives better SSEP signal) - NDMR decreases muscle artefact in SSEP (But full paralysis with NDMR ablates MEP completely making it useless) - Opioids and benzodiazepines have little effect Hence - SSEP: Use heavy remifentanil with light propofol TIVA & PTC NDMR - MEP: Use heavy remifentanil with light propofol TIVA with & no NDMR or NDMR to 1-2 twitches via infusion (OK for accurate MEP) Intraoperative wake up test - Done if change in recorded potential or injury suspected - Surgery halted while GA turned off and emergence allowed (stay on Remi) - Patient asked to move feet - If can move then continue surgery - If paraplegia then remove implants, treat hypotension and anaemia, and give high dose methylprednisolone. |
|
|
(11-March-Bank)
During lumbar plexus block placement, which of the following indicates inappropriate needle placement? A: hip flexion B: hip adduction C: knee extension D: knee flexion E: lumbar extension |
D or A
- Needle too caudad will stimulate sciatic plexus/nerve causing hamstring contraction - Needle too far in will directly stimulate psoas muscle causing hip flexion (subtle) - Aim is to see twitches of quadriceps muscle at 0.5-1.0mA - Lumbar plexus block disperses LA in psoas muscle fascial plane which blocks the roots of the lumbar plexus |
|
|
(05-April) (06-March) (06-July) (08-April) (10-August-Bank)
The sciatic nerve supplies the following muscles EXCEPT A. biceps femoris B. semitendinosus C. semimembranosus D. gluteus maximus E. adductor magnus |
D
- Gluteus maximus supplied by inferior gluteal nerve - Direct motor: Semitendinosus, Semimembranosus, Adductor magnus & Biceps femoris - Sensory: Hip joint - Terminal: Common peroneal & tibial nerves |
|
|
(05-April) (07-April) (07-July) (09-August-Bank) (10-March-Bank) (10-August-Bank)
The innervation of the human larynx is such that A. the internal laryngeal branch of the superior laryngeal branch of the vagus supplies the lingual surface of the epiglottis B. in the cadaveric position the cords are fully abducted C. the recurrent laryngeal nerve supplies all the intrinsic muscles of the larynx D. the glossopharyngeal nerves are sensory to the laryngeal mucous membrane above the level of the vocal cords E. cord paralysis can be produced by a distended endotracheal cuff in the larynx compressing a branch of the recurrent laryngeal nerve against the thyroid cartilage |
E
The anterior branch of the RLN can be compressed against the posterior part of the thyroid cartilage by the ETT cuff |
|
|
(09-August-Bank) (10-August-Bank)
Long duration of surgery, arms stretched out, head turned 30 degrees to right. On waking patient has a neurological deficit. Sensory loss over ventral lateral palm and 3 fingers, some weakness of the hand, weakness of the wrist, some paraesthesia of the forearm and weak elbow flexions. Most likely injury is A. Median nerve B. Ulnar nerve C. C5 nerve root D. Upper cervical trunk E. Musculocutaneous |
C
C5 nerve root |
|
|
(10-March-Bank) (10-August-Bank)
The intercostobrachial nerve: A. Arises from T2 trunk B. Is usually blocked in brachial plexus block C. Supplies antecubital fossa D. can be damaged by tourniquet E. Arises from inferior trunk |
D
Can be damaged by tourniquet |
|
|
(10-March-Bank) (10-August-Bank)
The nerve supplying area of skin between greater trochanter and iliac crest: A. subcostal nerve B. ilioinguinal nerve C. genitofemoral nerve D. femoral nerve E. lat cutaneous femoral nerve |
A
Subcostal nerve |
|
|
(10-March-Bank) (10-August-Bank)
The median nerve A. can be blocked at the elbow immediately medial to the brachial artery B. can be blocked at the wrist between palmaris longus and flexor carpi ulnaris C. can be blocked at the wrist medial to flexor carpi ulnaris D. is formed from the lateral, medial, and posterior cords of the brachial plexus E. provides sensation to the ulnar half of the palm |
A
The median nerve lies medial to the brachial artery at the elbow |
|
|
(10-August-Bank)
Stellate ganglion block. Needle entry next to SCM muscle at C6. Which direction to advance needle ? A. C3 B. C4 C. C5 D. C6 E. C7 |
D
Stellate ganglion is the ganglion formed by the fusion of the inferior cervical and first thoracic ganglion as the meet anterior to the vertebral body of C7 Indications - Pain syndromes - Vascular insufficiency Block - Patient supine with neck extended slightly and rotated slightly to opposite side - Retract SCM and Carotid artery laterally - Palpate for Chassaignac’s tubercle (anterior tubercle of transverse process of 6th cervical vertebra against which carotid artery can be compressed by the finger) - Needle between trachea and carotid sheath at level of cricoid cartilage at C6 level (to avoid pleural puncture) - Direct needle onto tubercle then redirect medially and inferiorly towards body of C6 - After contact with body of C6 retract needle 1-2mm, confirm position with fluoroscopy (spread of contrast cephalad and caudad between tissue planes) = belly of longus colli muscle - 10-15ml injection should result in Horner’s syndrome = successful block (ptosis = droop, miosis = constricted, & anhidrosis) |
|
|
(10-August-Bank)
A 4 year old child with Arthrogryposis multiplex congenita for dental surgery. Jaw rigidity post induction. Likely cause ? A. Temporomandibular joint involvement/ TMJ rigidity B. Inadequate depth of anaesthesia C. Inadequate muscle relaxation/ inadequate sux D. Masseter spasm E. ? |
A
Arthrogryposis = congenital limitation of joint movement - Classical = multiple symmetric contractures in limbs - Distal = hands & feet involved but large joints spared Intubation difficult due to small immobile jaw |
|
|
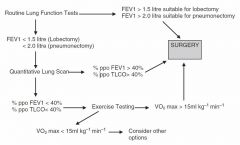
Pneumonectomy algorithm
|
|
|
|
(10-August-Bank)
Patient for pneumonectomy. Pre op FEV1 2.4. (Predicted 4.5L) FVC given as well. For R lower lobectomy. Postoperative predicted FEV1 ? A. 1.3 B. 1.5 C. 1.7 D. 1.9 E. 2.2 |
C
ppoFEV1 = pre-op FEV1 x % function of bad lung x (#segments remaining/total) - 19 segments total - RUL = 3, RML = 2, RLL = 5 (total right = 10) - LUL = 3, Lingula = 2, LLL = 4 (total left = 9) 2.4 x 14/19 = 1.77L (=40% predicted in this case) - Alternative formula = FEV1 x (5 – lobes resected) / 5 (where 5 is whole lung) |
|
|
(10-August-Bank)
You are on a humanitarian aid mission in the developing world. Drawover vaporiser apparatus described being used. Given 400 mm tubing, OMV or diamedica vaporiser, 200mm tubing attached to self-inflating bag. Which other ONE piece of equipment is ESSENTIAL to make this system functional? A. Halothane B. In-line Waters' Canister C. Non-rebreathing valve D. Oxygen source E. Ventilator |
C
Draw over requires non-rebreathing valve - Patient breathes atmospheric air - Drawn over vaporiser by patient’s inspiratory effort - Inhaled through non-rebreathing valve Water’s inline canister = CO2 absorber (not required) |
|
|
(10-August-Bank)
Positive predictive value is: A. The proportion of people without disease who are correctly identified as not having the disease. B. The proportion of people with disease who are correctly identified as having the disease. C. The proportion of people with disease who have a positive test result D. The proportion of people without disease who have a positive test result |
B
- PPV = proportion with a positive test who are correctly diagnosed - PPV = TP/(TP+FP) |
|
|
(07-April) (07-July) (09-August-Bank) (10-March-Bank)
In a trial 75 patients with an uncommon, newly described symptom and 50 matched patients without this symptom are selected for comparison of their exposure to a new drug. The results show Symptom present Symptom absent Exposed to new drug 50 25 Not exposed 25 25 From this data A. the relative risk of this symptom with drug exposure cannot be determined B. the odds ratio of this symptom with drug exposure cannot be determined C. the relative risk of this symptom with drug exposure is 2 D. the odds ratio of this symptom with drug exposure is 1.33 (recurring) E. none of the above are correct |
A
Can always calculate odds ratio but cant calculate relative risk unless we have information about total population |
|
|
(09-August-Bank) (10-March-Bank)
Branches of the mandibular nerve do NOT include the A. auriculotemporal nerve B. long buccal nerve C. lingual nerve D. great auricular nerve E. chorda tympani nerve |
D
Great auricular nerve (chorda tympani nerve is a branch from the lingual nerve) |
|
|
(10-March-Bank)
Plenum Vaporiser A.? something with fresh gas flows B. Relies on a constant flow of pressurised gas C. Out of circle D. Not temperature compensated E. volatile injected into fresh gas flow? |
B
Plenum vaporiser requires upstream positive pressure to push FGF through vaporiser (opposite to draw over vaporiser, uses negative pressure developed by patient spont vent) |
|
|
(10-March-Bank)
Non-normally distributed pain scores. What is the best way to describe spread of data? A. Inter-quartile range B. Standard deviation C. Standard error of the mean |
A
Pain scores = ordinal data - Ordinal = order matters but not difference between values (e.g. pain scores, 10/10 pain is not necessarily 2x as much pain as 5/10) - Interval = difference between values meaningful (e.g. degrees Celsius) - Ratio = difference meaningful and true zero (e.g. height) Use inter-quartile range for interval data that is not normally distributed For normally distributed data Standard Deviation best describes spread from the mean - Parametric = normally distributed symmetrical data - A sample drawn from the population can be assumed to be normally distributed if the sample size is large enough - If the sample is too small then should use non-parametric inferential statistics (does not take into account assumed shape of data spread) - SD describes spread from the mean (68% falls within 1 SD) - SEM describes precision of sample mean (how far is the sample mean from the population mean) |
|
|
(10-March-Bank)
What term means the number of people who are correctly identified as not having a disease: A. Sensitivity B. Specificity C. Positive predictive value D. Negative predictive value |
B
Specificity = TN Rate Specificity = proportion of people who are healthy who are correctly identified - Specificity = TN/(TN+FP) - If a test is 100% specific then ALL well people are correctly labelled well (but there may still be false negatives – so doesn’t help you rule out the disease) - Hence, a highly specific test helps you rule in disease with a positive result (SPIN: High Specificity Positive rules IN) Sensitivity = proportion of people who are sick who are correctly identified - senSitivity (s = sick) - Sensitivity = TP/(TP+FN) - If a test is 100% sensitive then ALL sick people are correctly labelled sick (but there may still be false positives – so it doesn’t help you rule in the disease) - Hence, a highly sensitive test helps you to rule out disease with negative result (SNOUT: High Sensitivity Negative rules OUT) |
|
|
(09-April-BANK) (09-August-Bank)
Which of the following can be used to describe the spread of non-parametric data? A. standard deviation B. interquartile range C. confidence interval D. standard error E. variance coefficient |
B
Interquartile range used to describe spread of non-parametric data |
|
|
(09-August-Bank)
All these nerves provide some sensation to upper arm EXCEPT a. Musculocutaneous b. Intercostobrachial c. Radial d. Circumflex e. Median antebrachial? |
A
Musculocutaneous provides motor above elbow and sensory below elbow |
|
|
(09-August-Bank)
Advantage if supraclavicular over interscalene nerve block for shoulder surgery a. Less phrenic nerve block b. Easier landmarks in obese patient c. Arm can be in any position for block d. Less risk pneumothorax e. Better cover for shoulder surgery? |
A
Because supraclavicular block is performed in a more caudad location in the brachial plexus it decreases risk of neuraxial or phrenic nerve complications (Interscalene block results in phrenic nerve block in almost 100% resulting in 25% decrease in lung function) |
|
|
(09-August-Bank)
The basilic vein a. Arises from the dorsum of the hand b. Follows the superficial radial artery c. Pierces the clavipectoral fascia d. Becomes the brachial vein at the cubital fossa e. Arcs around the radial side of the forearm |
A
The basilic vein drains the dorsum of the hand on the ulnar side |
|
|
(09-April-BANK)
Which distinguishes C8-T1 from an ulnar nerve lesion at elbow? A. Paraesthesia of the 5th digit B. Paraesthesia over index finger C. Flexor carpi ulnaris function D. Paraesthesia/sensory loss over medial forearm E. Adductor pollicis function |
D
Medial cutaneous nerve of the forearm arises from the medial cord of the brachial plexus which is prior to the formation of the ulnar nerve |
|
|
(09-April-BANK)
Asking the patient to look up and in during a retrobulbar block increases the risk of injury to: A. Inferior oblique B. Superior oblique C. optic nerve D. globe E. ophthalmic artery |
C
The Atkinson ‘up and in’ position of gaze increases risk of optic nerve injury |
|
|
(09-April-BANK)
A man presents for an ankle fusion. Which of the following combinations will provide the best block: A. femoral nerve block B. common peroneal and femoral C. tibial and femoral D. ankle block E. sciatic nerve block |
E
Sciatic block is suitable for ankle and foot surgery |
|
|
(08-August-BANK)
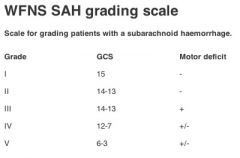
55 year old subarachnoid haemorrhage secondary to aneurysm. Patient is confused with a oculomotor (3rd cranial nerve) palsy, complains of a severe headache. This patient is in Hunt and Hess class: A. 0 B. 1 C. 2 D. 3 E. 4 |
D
3 Hunt and Hess: 1 Asymptomatic, mild headache, slight nuchal rigidity 2 Moderate to severe headache, nuchal rigidity, no neurologic deficit other than cranial nerve palsy 3 Drowsiness / confusion, mild focal neurologic deficit 4 Stupor, moderate-severe hemiparesis 5 Coma, decerebrate posturing |
|
|
(08-August-BANK)
The ascending aorta A. has no branches B. begins at the semilunar valve C. arises from right ventricle D. occupies the superior mediastinum E. lies inferior to the SVC |
B
Occupies the superior mediastinum (also starts from the aortic valve which is a semilunar valve, but so is the pulmonary valve) |
|
|
(08-August-BANK)
The nerve providing sensory supply to the airway muscle below (inferior) to the vocal cords is the A. phrenic nerve B. posterior thyroid nerve C. recurrent laryngeal nerve D. superior laryngeal nerve E. tracheal nerve |
C
Sensory innervation below the cords is from the RLN (sensory innervation above the cords is from the superior laryngeal nerve) |
|
|
(08-August-BANK)
Ciliary ganglion A. sympathetic from inferior cervical ganglion B. located inferiorly within orbit C. may be damaged during a peribulbar block D. preganglionic parasympathetic supply from the supra trochlear nerve E. preganglionic parasympathetic originates from the Edinger Westphal nucleus |
E
Preganglionic axons from the Edinger-Westphal nucleus travel along the occulomotor nerve and form synapses with the ciliary ganglion |
|
|
(05-April) (07-July) (08-April)
In a clinical trial, 3 out of 10 patients develop a complication in the control group, and 1 of 10 patients develops the complication in the treated group. To assess whether this is a statistically significant difference the most appropriate statistical test to use would be the A. Chi-square Test B. Chi-square Test with Yates correction C. Student 's t -test D. Fisher's Exact Test E. Mann-Whitney Test |
D
Fisher’s exact test for 2x2 with small sample size (<50) & non-parametric |
|
|
(05-April) (08-April)
Each of the following findings is consistent with brain death EXCEPT A. absence of diabetes insipidus i.e. continued vasopressin secretion B. Babinski's reflex C. focal EEG (electroencephalogram) activity D. limb movement in response to touch E. nystagmus on injection of cold water into the ear canal |
E
An intact vestibulo-ocular reflex indicates brain stem reflexes are intact and that brain death has not occurred You can still be brain dead with: - Spontaneous spinal movements of limbs - Respiratory-like movements without significant tidal volume - Sweating, blushing and tachycardia - Normal BP without pharmacological support - Absence of DI (normal osmolar control mechanism) - Deep tendon reflexes - Babinski’s reflex intact You can’t be brain dead with: - Decerebrate (flexion) or decorticate (extension) posturing - True extensor or flexor motor responses to painful stimuli - Seizures |
|
(05-July) (08-April)
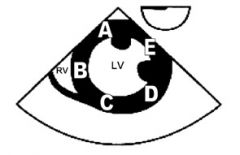
The diagram below is of a transgastric short axis view obtained during a transesophageal echocardiography examination. Which letter corresponds to the area supplied by the right coronary artery? |
A
A = RCA C = LAD E = Circumflex |
|
|
WFNS?
|
|
|
|
(05-July) (08-April)
Cauda equina syndrome A. involves large sensory flibres initially B. is not associated with back pain C. results from compression of nerve roots D. results in loss of sensation confined to the foot E. results predominantly in an upper motor neuron lesion |
C
- A: False. Smaller nerve fibres 1st affected by pressure, ischemia or toxins - B: False. Sensory loss in saddle distribution +/- low back pain - C: True. Usually due to compression (inappropriately large volumes in epidural space) - D: False. Sensory loss in saddle distribution - E: False. Lower motor neurone lesion (primarily S2-S4 sacral nerve roots → bladder atony and loss of voluntary micturition) |
|
|
(06-March) (06-July) (08-April)
The intercostal nerves A. arise as the sensory fibres of the anterior primary rami from their spinal segments B. give off a lateral cutaneous branch at the angle of the rib C. lie in the subcostal groove in only 50% of patients D. lie between the intercostalis intimi muscle and the pleura E. are enclosed in a dural sheath from their origin to the angle of the rib |
C
Branches of the intercostal nerves can be found anywhere between adjacent ribs |
|
|
(06-July) (07-April) (08-April)
Correct statements regarding confidence intervals (CI) include all the following EXCEPT A. CI are derived from the standard error (of the mean) B. CI can be used to assess the precision of population parameter estimates C. the width of the CI depends on the degree of confidence required D. the width of the CI depends on the sample size E. the width of the CI depends on the mean value of the sample |
E
- The mean value of the sample determines the position of the CI not its width |
|
|
(06-July) (08-April)
In morbidly obese patients drugs can be administered on a per kilogram of total body weight (TBW) or on a per kilogram of ideal body weight (IBW) basis. It is correct to say, A. atracurium should be administered on an IBW basis B. induction dose of propofol should be administered on an IBW basis C. induction dose of thiopentone should be administered on a TBW basis D. suxamethonium should be administered on a TBW basis E. vecuronium should be administered on a TBW basis |

B
A: False. Atracurium should be dosed on TBW (or 20% greater than IBW) B: True. Propofol dosed at IBW for induction C: False. Thiopentone dosed at IBW for induction D: False. Suxamethonium dosed at TBW BUT up to 120-140mg - Due to increased cholinesterase activity proportional to body weight - Doses 120-140mg known to provide satisfactory conditions for patients >140kg E: False. Vecuronium should be dosed on IBW |
|
|
(07-July) (08-April)
When a new diagnostic test is evaluated in a group of subjects in whom the diagnosis is known, the following results are obtained Disease known to be present Disease known to be absent New test result positive 2 4 New test result negative 6 8 The specificity of the new test is closest to A. 25% B. 33% C. 57% D. 67% E. 75% |
D
Specificity = TN rate (TN/TN + FP) = 8 / (8+4) = 66.6% |
|
|
(07-July) (08-April)
Which of the following statements regarding transient neurological syndrome (TNS) following spinal anaesthesia is FALSE? A. it is more common in patients placed in the lithotomy position B. it is more common following lignocaine C. it is unlikely to be due to neurotoxicity D. it may progress to cauda equina syndrome E. it resolves within 72 hours in the majority of patients |
D
Does not progress to cauda equina syndrome |
|
|
(07-July) (08-April)
Regarding spinal cord blood supply, the A. anterior spinal artery arises from the posterior inferior cerebellar arteries A. anterior spinal artery supplies 50% of the spinal cord, while the 2 posterior spinal arteries supply 25% each C. largest radicular artery is usually in the lumbar region D. posterior spinal arteries are only supplied by radicular arteries E. upper cervical segment of the spinal cord receives most of its blood flow from the vertebral arteries |
E
- A: False. Anterior spinal artery arises from vertebral artery - B: False. Anterior spinal artery supplies 2/3 (posterior supplies 1/3) - C: False. Largest radicular artery arises T9 and T11 - D: False. Posterior spinal arteries arise from posterior inferior cerebellar arteries - E: True. Anterior spinal artery arises from vertebral artery |
|
|
(08-April)
An 80-year-old male with peripheral vascular disease undergoes unilateral chemical lumbar sympathectomy. The most likely complication he will experience is: A. Genitor femoral neuralgia B. haematuria C. lumbar radiculopathy D. postural hypotension E. psoas haematoma |
A
Complications lumbar sympathectomy: - Genitofemoral nerve injury (5%) - Ileus - Ureteric injury - Major vessel injury - Bowel injury |
|
|
(08-April)
When obtaining an image using ultrasound, the most effective way to improve the spatial resolution is to increase the: A. 2D gain B. frame rate C. single scatter D. time gain compensation E. transducer frequency |
E
Increasing transducer frequency increases spatial resolution |
|
|
(08-April)
You are asked to review a patient on the day after an uneventful Caesarean section under spinal anaesthesia. She is complaining of pain and numbness on the upper, outer aspect of her right thigh which she first noticed on the night of the delivery. On further questioning you establish that she has not been incontinent. Review of the medical record reveals that the spinal anaesthesia was administered through a 27 gauge pencil-point needle at the L3/4 intervertebral space and was atraumatic. On examination she is moderately obese. You note some oedema of her hands and feet. The power and reflexes in her lower limbs are normal. She has an area of numbness to pin prick on the outer upper right thigh as shown in the illustration below. The most likely diagnosis is: A. A conus medullaris lesion B. a first lumbar (L1) nerve root lesion C. a second lumbar (L2) nerve root lesion D. a third lumbar (L3) nerve root lesion E. meralgia paraesthetica |
E
Meralgia paraesthetica = painful mononeuropathy of lateral femoral cutaneous nerve |
|
|
(08-April) (08-August)
Number needed to treat (NNT) is the number of patients who need to be treated to prevent one additional bad outcome. The NNT (of a treatment) is the reciprocal of the: A. absolute odds of the bad outcome B. absolute risk of the bad outcome C. absolute risk reduction in the bad outcome (due to the treatment) D. odds ratio of the bad outcome (due to the treatment) E. relative risk of the bad outcome (due to the treatment) |
C
NNT = reciprocal of ARR in bad outcome |
|
|
(08-April)
You are performing an awake fibreoptic intubation, through the nose, on an adult patient. In order, the fibrescope will encounter structures with sensory innervation from the following nerves: A. facial, trigeminal, glossopharyngeal B. facial, trigeminal, vagus C. glossopharyngeal, trigeminal, vagus D. trigeminal, glossopharyngeal, vagus E. trigeminal, vagus, glossopharyngeal |
D
Trigeminal, glossopharyngeal, vagus |
|
|
(08-April-BANK)
(Shown image of neck ultrasound with arrow pointing to the carotid artery) Regarding what the arrow is pointing to: A. This will collapse with pressure B. With colour doppler we see red if the probe is directed caudally C. Is part of the brachial plexus D. Will get smaller with Valsalva E. Should centre image over this for CVC insertion |
B
Red = towards scan head, Blue = away from scan head |
|
|
(08-April-BANK)
Retrobulbar block is least likely to block which muscle? A. Lateral rectus B. Superior oblique C. Levator palpebrae superioris D. Inferior rectus E. Medial rectus |
B
Least likely to block Superior oblique with retrobulbar block |
|
|
(05-April) (07-July)
The muscles of the larynx which separate the vocal cords are the A. thyro-arytenoids B. lateral crico-arytenoids C. oblique arytenoids D. posterior crico-arytenoids |
D
- The posterior cricoarytenoid muscles are the only muscles which abduct the vocal cords - Does this by external rotation of the arytenoid resulting in opening of the glottis |
|
|
(05-April) (06-July) (07-April) (07-July)
Sensation from the lobule of the external ear is mediated mostly by A. the auriculo-temporal nerve B. the great auricular nerve C. the lesser occipital nerve D. the greater occipital nerve E. none of the above |
B
Greater auricular has 3 terminal branches - Auricular = lower 2/3 medial external ear and lateral lobule - Mastoid = skin over mastoid process - Facial = skin over masseter and parotid |
|
|
(05-April) (07-July)
Which of the following statements is INCORRECT? Recombinant Factor VIIa A. directly activates Factors IX and X on the surface of activated platelets, leading to thrombin formation B. has a half-life of three and a half hours C. has been used "off-label" for bleeding in trauma patients D. is best monitored by the prothrombin time, which is shortened in a dose-dependent manner at therapeutic doses E. was developed for patients with haemophilia A and B who have inhibitors to Factors VIII and IX respectively |
D
- A: True. Novoseven directly activates VIII and IX on platelet surface - B: True. Novoseven T1/2 = 2-6 hours - C: True. Novoseven has been used extensively in trauma - D: False. Improvement in coags do not correlate with level of haemostasis achieved - E: True. Novoseven was developed for patients with haemophilia A&B (where inhibitors to VIII are developed secondary to frequent blood transfusions) |
|
|
(06-March) (07-April) (07-July)
Fondaparinux sodium (Arixtra) A. activates platelets B. cross reacts with sera from patients with heparin induced thrombocytopaenia C. has a mechanism of action that is antithrombin (ATIII) dependent D. is associated with thrombocytopenia E. can be safely used in patients with severe renal impairment |
C
- A: False. No effect on platelet aggregation. - B: False. Does not cross react with HITS positive sera - C: True. Binds ATIII → potentiates (300x inhibition of Xa) - D: False. Not associated with HITS - E: False. Completely excreted by kidney unchanged ∴ contraindicated in renal failure Dabigatran and Hirudin are direct thrombin inhibitors (factor II) Fondaparinux and Rivaroxaban are direct Xa inhibitors Heparins act via potentiation of antithrombin III - LMWH potentiates inhibition of Xa more than IIa - Whereas unfractionated heparin potentiates inhibition of both Xa and IIa equally |
|
|
(07-April) (07-July)
Forty patients are randomly divided into two groups – one to receive induction agent A and another to receive induction agent B. The next day they are asked to rate their anaesthetic experience on a scale of 1 (very bad) to 5 (very good). The most appropriate test to compare the anaesthetic experience of the two groups is the A. unpaired t-test B. Mann-Whitney test C. Chi-square test D. Kruskal-Wallis test E. paired t-test |
B
Ordinal data (non-parametric) hence use Mann-Whitney U Mann-Whitney U test is the “t-test” for non-parametric data |
|
|
(07-July)
An 80 year-old man is undergoing bilateral orchidectomy. You have administered spinal anaesthesia using heavy bupivacaine with the patient in the sitting position. The minimum adequate block for this procedure can be presumed when you can demonstrate a loss of skin sensation at the A. symphysis pubis B. midpoint between the symphysis pubis and the umbilicus C. umbilicus D. xiphisternum E. nipple |
C
Need block to T9/10 (umbilicus) |
|
|
(07-July)
An 85-year-old woman requires an emergency repair of an obstructed inguinal hernia. She has recently suffered a pulmonary embolus and is taking warfarin. You elect to perform an inguinal field block. Which of the following nerves does NOT need to be blocked? A. iliohypogastric B. ilioinguinal C. ilioinguinal of the contralateral side D. femoral E. subcostal |
D
Femoral not required Nerves required for inguinal field block - Ilioinguinal - Iliohypogastric - Genitofermal - Subcostal & thoracic - Also, all of above on contralateral side |
|
|
(05-April) (07-April)
In a patient with myasthenia gravis undergoing a laparotomy for large bowel obstruction, the need for postoperative ventilation is significantly increased by a A. daily dose of pyridostigmine > 180 mg B. known history of resistance to suxamethonium C. known history of sensitivity to non-depolarising muscle relaxants D. past history of prednisolone treatment >10 mg.day-1 E. recent history of dysphagia |
E
A recent history of dysphagia indicates bulbar palsy which is predictive requiring post operative ventilation |
|
|
(06-March) (06-July) (07-April)
When a new diagnostic test is evaluated in a population of subjects in whom the diagnosis is known, the following results are obtained Disease known Disease known To be present to be absent New test result positive 80 40 New test result negative 20 180 In this population the POSITIVE predictive value of this test is closest to A. 10% B. 33% C. 67% D. 80% E. 90% |
E
NPV = TN/(TN+FN) = 180/200 = 90% |
|
|
(06-July) (07-April)
At the wrist joint A. the median nerve lies between the tendons of palmaris longus and flexor carpi radialis B. the median nerve lies medial to the tendon of flexor carpi ulnaris C. the radial artery is usually palpable just medial to the tendon of flexor carpi radialis D. the ulnar artery and nerve enter the hand by passing deep to the flexor retinaculum |
A
Median nerve lies between flexor retinaculum and palmaris longus tendon |
|
|
(06-July) (07-April)
The largest and most direct branch of the internal carotid artery is the A. ophthalmic B. anterior cerebral C. middle cerebral D. posterior cerebral E. choroidal |
C
Middle cerebral is the largest & most direct branch of the internal carotid |
|
|
(06-July) (07-April)
A 50 year old patient is admitted with acute chest pain. An ECG shows tall R waves in lead V1. The most likely diagnosis is A. occlusion of the anterior descending coronary artery B. a lateral myocardial infarction C. pulmonary infarction D. posterior myocardial infarction E. occlusion of the circumflex artery |
D
Tall V1 (R/S ratio > 1) most commonly due to posterior MI |
|
|
Sensitivity Specificity table?
|
|
|
|
(06-July) (07-April)
A new test has been developed to diagnose a disease. To determine the SPECIFICITY of this new test it should be administered to A. a mixed series of patients i.e. some known to be suffering from the disease and some known to NOT be suffering from it B. a series of patients known to NOT be suffering from the disease C. a series of patients known to NOT be suffering from the disease and an estimate of the prevalence of the disease in the population obtained D. a series of patients known to be suffering from the disease E. a series of patients known to be suffering from the disease and an estimate of the prevalence of the disease in the population obtained |
B
Specificity = TN/(FP+TN), hence need to do test on population known not to have the disease and look for false positives |
|
|
(07-April)
Block of the maxillary nerve in the pterygo-palatine fossa provides ipsilateral analgesia of the A. hard palate B. nasal septum C. posterior part of the lateral wall of the nose D. upper incisor teeth E. upper molar teeth |
B
Block of the maxillary nerve in the pterygo-palatine fossa provides ipsilateral analgesia of the nasal septum |
|
|
(07-April)
A 70-year-old diabetic requires forefoot amputation. You wish to block the most peripheral nerves possible to provide complete anaesthesia for this procedure. Nerves which you would need to block include the A. medial and lateral plantar B. sciatic and saphenous C. sural and deep peroneal D. superficial and deep peroneal E. tibial and common peroneal |
C
- Sciatic (blocks branches sural, tibial, deep & superficial peroneal) and saphenous - (Ankle block ideal for forefoot surgery) |
|
|
(05-April) (06-March) (06-July)
The median nerve A. can be blocked at the elbow immediately lateral to the brachial artery B. can be blocked at the wrist between palmaris longus and flexor carpi ulnaris C. can be blocked at the wrist medial to flexor carpi ulnaris D. is formed from the lateral, medial, and posterior cords of the brachial plexus E. provides sensation to the radial half of the palm |
E
- A: False. Median nerve lies medial to brachial artery at elbow - B: False. Median nerve lies between FCR and PL at wrist - C: False. Median nerve lies between FCR and PL at wrist - D: False. Median nerve formed from lateral and medial cords of brachial plexus (not posterior) - E: True. Median nerve supplies sensation to radial 3.5 digits and radial palm NB: there is an alternate version in 2010 |
|
|
(05-April) (06-March) (06-July)
The most correct statement regarding the Child-Pugh score for liver disease is that A. high-risk score is not possible with normal aminotransferase levels B. a high-risk score is possible without encephalopathy C. a prothrombin time greater than 10 seconds above normal confers extra points to the raw score D. it has not been validated for non-shunt and nontransplant laparotomies E. it was originally developed for patients undergoing hepatic transplantation |
B
- Can still score 13/15 without encephalopathy (i.e. Grade C) Child Pugh: - Encephalopathy (none = 1, confused = 3) - Ascites (none = 1, moderate = 3) - Bilirubin (<2 = 1, >3 = 3) - Albumin (>3.5 = 1, <2.8 = 3) - INR (<1.7 = 1, >2.3 = 3) Min = 5, Max = 15 - A = 5-6 - B = 7-9 - C = 10-15 |
|
|
(06-March) (06-July)
The segmental nerve supply to the renal pelvis and the ureter gives an anatomical basis for the surface representation of the pain of renal colic. The segments concerned are A. T11 and T12 B. L1 C. L1 and L2 D. T11, T12, L1 and L2 E. T12 and L1 |
D
Ureter = T11-L2 (felt in loin to groin + anterior thigh) |
|
|
(06-March) (06-July)
The power of a statistical test can be expected to decrease, if there is an increase in A. the sample size B. the size of the treatment effect C. the chance of making a Type 1 error D. the variability of the population E. none of the above |
D
- Power = likelihood of detecting a specified difference if it exists - Power is equal to 1 - β - Increased sample size → ↑power - Increased effect size → smaller sample size required → ↑power with same n - Increased variability in population → ↓power |
|
|
(06-March) (06-July)
Complications of an intra-orbital local anaesthetic block are minimised if A. the eye is oriented in a supero-medial direction for an infero-lateral injection B. the anaesthetic solution is placed posteriorly where the nerves are close together C. a shallow bevel (Atkinson -type) rather than a sharp intravenous-type needle is used D. the injection site is medial rather than supero-medial E. retro-bulbar needle placement is used for all myopic patients |
D
Medial approach is preferred to supero-medial approach due to less risk of globe perforation |
|
|
(06-July)
Fibres contained in the recurrent laryngeal nerve include A. motor supply to the crico-thyroid muscles B. motor supply to the crico-arytenoid muscles C. sensory fibres from the epiglottis D. sensory fibres from the crico-thyroid joint E. sensory fibres from the supra-glottic mucosa |
B
Nerve supply to larynx: 1. Recurrent laryngeal - Motor supply to all muscles except cricothyroid muscle - Sensation below vocal cords and interior surface of cords 2. Superior laryngeal - Internal laryngeal supplies sensory to mucosa above vocal cords - External laryngeal supplies motor to cricothyroid muscle and inferior constrictor of pharynx (outside larynx) |
|
|
(06-July)
During an epidural block, an indication that all sympathetic cardio-accelerator fibres have been blocked would be an upper sensory level at the A. tip of the xiphoid B. nipple line C. apex of the axilla D. inner aspect of the upper arm E. little finger |
E
- Little finger = C8 - Medial aspect of upper arm = T2 (i.e. may not cover T1-4) |
|
|
(06-July)
Intra-nasal topical cocaine used in nasal surgery A. has a duration of action of the order of 6 hours B. is metabolised more quickly by the liver if the patient is using ecothiopate eye drops C. is typically used in a dose of approximately 5 ml of 5% solution in an adult D. may be metabolised more slowly in patients with liver disease E. reaches a peak plasma concentration in 3 hours |
D
- A: False. Peak 2-5min, duration 30-45min. - B: False. Echothiophate = cholinesterase inhibiting effect - C: False. Usual dose 2mg/kg (5ml 5% = 250mg) - D: True. Metabolised by plasma and liver cholinesterases - E: False. Peak plasma concentration at 3 hours |
|
|
(06-July)
One hundred vomiting patients receive ondansetron. If 25 patients, who would not have stopped vomiting had they received a placebo, stop vomiting, then the number needed to treat (NNT) for ondansetron to stop vomiting is A. 1.3 B. 4 C. 25 D. 100 E. cannot be calculated without information on placebo success rate |
B
- Risk reduction = 100-75/100 = 25% - NNT = 1/ARR = 4 |
|
|
(06-July)
The diagram below represents a transgastric short axis view of the heart obtained using transoesphageal echocardiography. The structure labelled A is the A. anterolateral papillary muscle B. non-coronary leaflet of the aortic valve C. posterior mitral valve commissure D. posterolateral papillary muscle E. posteromedial papillary muscle |
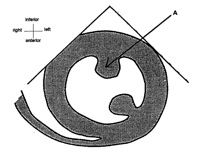
E
- Posteromedial papillary muscle - (other bulge is anterolateral papillary muscle) |
|
|
(06-July)
Regarding thoracic anatomy, the A. aorta passes through the diaphragm posteriorly at T10 B. carina most commonly lies at T4 in the adult C. lungs comprise 16 bronchopulmonary segments in total D. oblique fissure runs along the 6th rib on both sides E. right main bronchus runs 45° to the vertical |
B
Trachea bifurcates at T4 (angle of louis) |
|
|
(06-July)
Ebstein's abnormality describes a congenital defect of the A. aortic valve B. mitral valve C. pulmonary valve D. pulmonary veins E. tricuspid valve |
E
Ebstein’s = tricuspid valve malformation (partly attached to valve annulus and to RV endocardium) |
|
|
(05-April) (06-March)
Hoarseness following a total thyroidectomy may be due to damage to the A. deep cervical plexus B. external branch of the superior laryngeal nerve C. hypoglossal nerve D. internal branch of the superior laryngeal nerve E. superficial cervical plexus |
None?
Recurrent laryngeal nerve - Supplies all muscles of the larynx except cricothyroid muscle - Injury results in hoarseness Superior laryngeal nerve injury - Internal supplies sensory to larynx and is not normally at risk in OT - External supplies motor to cricothyroid muscle which lengthens cords - Injury results in inability to make high pitched sounds Hypoglossal controls the tongue - Injury can result in slurring of speech |
|
|
(05-July) (06-March)
The second cervical nerve root A. passes between the transverse process of the axis (C2) and C3, to emerge and divide into anterior and posterior primary rami B. contributes fibres through the anterior primary ramus, which go on to form the greater occipital nerve C. can be blocked near the occipital artery at the nuchal line D. can be blocked 1 cm caudad to the mastoid process and 1cm posterior to the line joining the tip of the mastoid to the anterior tubercle of C6 |
D
- 1st cervical nerve root exits superiorly to the 1st cervical vertebral body - 2nd cervical nerve root exits the intervertebral foramina (between bodies of C1 & C2) - Deep cervical block achieved by small volume LA near transverse process of C2-4 Block: - Supine patient with head turned away - Identify mastoid process - Identify transverse process of C6 (at level of cricoid cartilage = the most prominent cervical transverse process) - Draw line between (roots of cervical plexus are beneath this line) - Transverse process of C2 is 1.5-2cm distal to tip of mastoid process - C4 is midway between clavicle and mastoid process - C3 is midway between C2 and C4 |
|
|
(05-July) (06-March)
The standard error of the mean is A. dependent for its validity on a normal distribution in the population B. an indication of the likelihood of making a type II error C. about 2, if the standard deviation is 15 and the sample size 50 D. not necessary for calculating the confidence interval for the mean E. the variance of the population of sample means |
C
- SEM = SD/√n - SEM = 15/√50 = 2 |
|
|
(05-July) (06-March)
Correct statements regarding trigeminal neuralgia include A. associated sensory loss is common. B. it most frequently occurs in the second or third division of the nerve (V2 or V3) C. oedema of the trigeminal ganglion is usually seen on a cranial CAT scan D. the pain is often bilateral E. the pain is usually described as an intense deep ache |
B
- A: False. Sensory loss not common - B: True. Mostly involves both mandibular and maxillary divisions - C: False. - D: False. Pain is usually unilateral - E: False. Pain is shooting, sharp and has pain-free intervals |
|
|
(05-July) (06-March)
Regional anaesthesia for modified radical mastoidectomy requires blockade of the following nerves EXCEPT A. greater auricular B. auriculotemporal C. auricular branch of the vagus D. facial E. tympanic branch of the glossopharyngeal |
D
Facial nerve block not required - Anaesthesia of facial nerve not required - Need to block 4 nerves which supply sensation to the ear 1. Auriculotemporal = external auditory meatus 2. Greater auricular = medial-lower aspect of auricle 3. Auricular branch of vagus = concha and external auditory meatus 4. Tympanic = tympanic cavity - Also, surgeons will need to test facial nerve function (close to operative site and vulnerable to damage) |
|
|
(05-July) (06-March)
Anatomical features of the spinal cord do NOT include A. an anterior median fissure and a posterior median septum B. thirty-two pairs of spinal nerves C. a flilum terminale ending at the coccyx D. four to six spinal arteries arising from the posterior inferior cerebellar arteries E. the anterior spinal artery arising from the vertebral arteries |
B
- A: True. Cord has anterior median fissure and posterior median sulcus from which a glial posterior median septum extends halfway into substance of the cord - B: False. 31 pairs of nerves (C8, T12, L5, S5 + 1 coccygeal) formed from an anterior and posterior spinal root - C: True. Filium terminale connects conus medullaris to coccyx - D: True. Each posterior spinal artery arises from the posterior inferior cerebellar artery (PICA) at the same level - E: True. Anterior spinal artery arises from the two vertebral arteries - Spinal cord supplied by vertebral arteries in the neck descending from the base of skull - 1 anterior spinal artery (supplies the anterior 2/3 of the spinal cord) - 2 posterior spinal arteries supply the dorsal columns (posterior 1/3) - Various radicular arteries branch off the thoracic and abdominal aorta to provide additional blood supply - Artery of Adamkiewicz = the largest of these at T9-T11, and supplies the lower thoracic and upper lumbar parts of the cord, hence in spinal injury or aortic surgery may compromise blood supply of lower part of cord |
|
|
(05-July) (06-March)
The most correct statement describing the effect of the antithrombotic agents on the coagulation cascade is that A. low molecular weight heparin directly inhibits activated factor X B. low molecular weight heparin directly inhibits thrombin C. unfractionated heparin directly inhibits activated factor X D. unfractionated heparin directly inhibits thrombin E. ximelagatran directly inhibits thrombin |
E
Ximelagatran (Dabigatran is the current drug) and Hirudin are direct thrombin inhibitors (factor II) Fondaparinux and Rivaroxaban are direct Xa inhibitors Heparins act via potentiation of antithrombin III - LMWH potentiates inhibition of Xa more than IIa - Whereas unfractionated heparin potentiates inhibition of both Xa and IIa equally |
|
|
(05-July) (06-March)
Regarding sampling blood for elevated histamine and mast cell tryptase (β-tryptase) levels to confirm a possible anaphylactic reaction, which of the following statements is INCORRECT? A. a sample for histamine can be taken up to two hours after the event B. a sample for tryptase can be taken up to six hours after the event C. a sample for tryptase can be taken up to two days after fatal anaphylaxis D. tryptase levels can be elevated after amniotic fluid embolism E. tryptase levels can be normal after clinical anaphylaxis |
A
Histamine: - Peaks 5-15 mins (return to baseline at 30 mins) - Hence need to take sample within 30 minutes Tryptase: - Peaks within 1 hour (remains elevated 4-6 hours) - Hence need to take sample within 1-6 hours - Additional sample at least 24 hours after all symptoms have resolved (to provide a baseline and exclude mastocytosis) |
|
|
(05-July) (06-March)
Muscles which abduct the vocal cords include the A. aryepiglottic B. cricothyroid C. lateral cricoarytenoid D. posterior cricoarytenoid E. thyroarytenoid |
D
Posterior cricoarytenoid muscle abducts the cords |
|
|
(06-March)
The sural nerve A. is a branch of the posterior tibial nerve B. supplies the skin of the anterior two thirds of the sole of the foot C. lies anterior to the lateral malleolus at the ankle D. reaches the foot in contact with the short saphenous vein E. supplies the small muscles of the foot |
D
The sural nerve runs with the short saphenous vein Sural nerve and posterior tibial are branches of the tibial nerve |
|
|
(06-March)
During anaesthesia for Magnetic Resonance Imaging, A. any ferromagnetic items outside the 30 Gauss line will not be strongly attracted to the magnetic core B. any battery-powered monitor of non-ferromagnetic construction can be safely placed close to the magnetic core without risk of attraction to the magnet C. the most commonly used MRI contrast medium, gadopentetate dimeglumide (Magnevist) induces a similar incidence of side effects as does the iodinated contrast media used in radiology D. it is essential to limit the use of halogenated agents as halogen atoms exhibit the property of nuclear magnetic resonance and may interfere with image quality E. permanant pacemakers can only be permitted if they have been completely disabled prior to the MRI |
A
A: True. - 30 gauss line is where metal objects can become deadly projectiles - 5 gauss line is where medical devices can malfunction (e.g. infusion pumps) B: False. Batteries are strongly ferromagnetic hence not MRI safe C: False. Magnevist has higher therapeutic index than iodine contrast D: False. E: False. Pacemakers are contraindication to MRI (but some low ferrous ones have been OK) |
|
|
(06-March)
Post partum foot drop is most frequently caused by A. compression of the lumbosacral trunk by the foetal head or forceps B. damage to the common peroneal nerve from lithotomy position C. damage to the conus medullaris by misplaced spinal anaesthesia D. L4 Nerve root damage from epidural analgesia E. the excessive lumbar lordosis of pregnancy stretching nerve roots |
A
- Foot drop occurs most commonly from lumbosacral trunk compression (from baby’s head or forceps compressing nerve against sacrum) - Less commonly can occur with common peroneal nerve palsy from prolonged lithotomy |
|
|
(06-March)
In a group of subjects, the proportion vomiting is 80%. With treatment, this can be reduced to 60%. For this group of subjects, the number needed to treat (NNT) with this treatment is A . 3 B . 4 C . 5 D . 6 E . 7 |
C
ARR = 20% (80% minus 60%) NNT = 1 / ARR = 1 / 0.2 = 5 |
|
|
(05-April) (05-July)
In the hand the median nerve supplies A. abductor pollicis brevis B. adductor pollicis C. the first dorsal interosseous D. abductor pollicis longus E. extensor indicis |
A
- Median nerve supplies the LOAF muscles of the hand (rest supplied by ulnar) - (Meat) LOAF: - Lateral two lumbricals - Opponens pollicis - Abductor pollicis brevis - Flexor pollicis brevis |
|
|
(05-April) (05-July)
If a patient experiences paresthesia in the little finger during supraclavicular brachial plexus block, the needle is in proximity to the A. posterior cord B. middle trunk C. ulnar nerve D. lower trunk E. medial cord |
E
- Supraclavicular & Infraclavicular blocks are at the level of cords (brachial plexus) - Medial cord contributes to ulnar nerve only, hence needle in proximity to this - Interscalene block is at the level of trunks - If this question regarded Interscalene block answer would be D (lower trunk) |
|
|
(05-April) (05-July)
Clinical information about the likelihood of awareness during general anaesthesia CANNOT be usefully obtained using A. somatosensory evoked spinal cord potentials B. electroencephalogram frequency C. lower oesophageal contractility D. the isolated forearm technique E. electroencephalogram latency and amplitude of evoked potentials |
A – SSEP of spinal cord does not measure cortical activity (hence does not monitor for awareness)
|
|
|
(05-April) (05-July)
Radiation from X-rays A. has a non-cumulative effect on the bone marrow B. affects the thyroid gland more in patients over 16 years old C. has a recommended maximum whole body dose for the general population of 1,000 μSv.year-1 D. should be limited to less than 100 μSv.year-1 in pregnancy E. h as a recommended maximum whole body dose for occupational exposure of 500,000 μSv.year-1 |
C
- A: False. Radiation has a cumulative effect on bone marrow - B: False. More effect in under 16 year olds - C: True. Recommended MAX for general population = 1000 micro-Sieverts per year - Skull X-ray = 40 micro-Sieverts - CXR (2 view) = 250 micro-Sieverts - Foetal exposure from maternal CXR = 1/360th (0.7 micro-Sieverts) - D: False. Recommended dose in pregnancy same as for general population - E: False. Recommended MAX for occupational exposure = 50,000 micro-Sieverts per year |
|
|
(05-April) (05-July)
The sciatic nerve A. can be readily identified during neural blockade by the production of paraesthesia on contact with a needle B. has no sympathetic fibres C. is formed from the dorsal branches of the anterior rami of L5 and Sl to S4 D. provides motor innervation to the psoas muscle E. provides sensory innervation to the knee joint |
E
- Sciatic arises L4-S3 - Contains sensory, motor and sympathetic fibres - Provides motor to posterior thigh and muscles below knee via divisions (tibial and common peroneal nerves) - Genicular branches of tibial nerve supply most of knee joint (as well as femoral and obturator receiving sensory information from knee joint) |
|
|
(05-July)
The second lumbar nerve root (L2) normally contributes to each of the following nerves EXCEPT A. femoral nerve B. obturator nerve C. genito-femoral nerve D. lateral cutaneous nerve of the thigh E. ilio-inguinal nerve |
E
- Ilioinguinal nerve derived from L1 only, others all have derivation from L2 |
|
|
(05-July)
Which of the following alternatives is correct regarding the range of values that odds ratios (OR) and relative risks (RR) can take? A. OR (0 to positive infinity); RR (0 to positive infinity) B. OR (negative infinity to positive infinity); RR (negative infinity to positive infinity) C. OR (0 to 1); RR (0 to 1) D. OR (0 to positive infinity); RR (negative infinity to positive infinity) E. OR (negative 1 to positive 1); RR (negative 1 to positive 1) |
A
- 1 = both groups have same probability - 3 = 3x more likely to occur - Odds ratios overestimate risk (Relative risk should be used in preference) - Can always calculate odds ratio but cant calculate relative risk unless have information about total population |
|
|
(05-July)
A placebo should be used in a clinical trial when A. observer bias is possible B. a type one error is probable C. an acceptable standard treatment is not known to exist D. a placebo effect is anticipated E. human patients are used as subjects |
C
- Use placebo where acceptable standard treatment not known - Otherwise compare study intervention with gold standard rather than placebo |
|
|
(05-July)
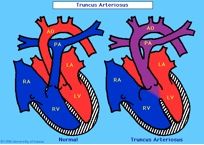
During controlled ventilation of a neonate prior to repair of a truncus arteriosus which of the following is MOST likely to be deleterious? A. controlled hypoventilation B. ventilation with air C. ventilation with an FiO2 of 0.18 D. ventilation with nitric oxide E. ventilation with PEEP of 3 cmH2O |
D
Truncus arteriosus = Embryological structure known as truncus arteriosus fails to properly divide into the pulmonary trunk and aorta - Results in complete mixing of blood at the level of the great vessel - Causes R-L shunt Sudden drop in PVR with nitric oxide can direct more blood towards PA rather than Aorta resulting in systemic hypotension & potentially coronary ischemia (aim to “keep status quo”) |
|
|
Truncus?
|
|
|
|
(05-April)
Each of the following statements regarding DVIR pacing is true EXCEPT A. atrial sensing inhibits atrial pacing B. pacing will usually provide AV (atrioventricular) synchrony C. the rate of pacing can be altered by patient activity D. ventricular sensing inhibits atrial pacing E. ventricular sensing inhibits ventricular pacing |
A is false (atria not sensed)
NBG Codes for pacing 1 = Chamber paced (A, V, D, O) 2 = Chamber sensed (A, V, D, O) 3 = Response to sensing - I = Sensed event causes inhibition of output pulse (until next cycle) - T = Sensed event causes triggering of output pulse - D = Dual modes of response - Sensed atrial event inhibits atrial output but triggers ventricular output pulse - Programmable delay to mimic normal PR interval - If ventricular event sensed during that cycle then ventricular output inhibited (i.e. full native rhythm) 4 = Functions - R = Sensed patient activity causes increase in paced HR 5 = Position of multisite pacing (rarely used) E.g. DOO = Dual pacing ignoring any intrinsic rhythm E.g. DVIR = Sensed ventricular event causes inhibition of atrial and ventricular output (but if no ventricular event sensed then output will be to atria and ventricles) PLUS rate modulation |
|
|
(05-April)
The recommended concentration of hyaluronidase as an aid for local anaesthesia in peribulbar injection for ophthalmic surgery is A. 25 IU (International Units).ml-1 of local anaesthetic solution B. 50 IU.ml-1 of local anaesthetic solution C. 100 IU.ml-1 of local anaesthetic solution D. 150 IU.ml-1 of local anaesthetic solution E. 1500 IU.ml-1 of local anaesthetic solution |
A
- Recommended concentration is 25IU hyaluronidase - Gives better diffusion, greater anaesthesia, more effective akinesia of orbicularis and extraocular muscles, and less ballooning of tissues - Typical dilution: - Take 1 ampule of 1500IU hyaluronidase - Dilute to 1ml (gives 150IU per 0.1ml) - Add 0.1ml to 6ml LA (gives 25IU hyaluronidase per ml LA) |
|
|
Crani Sensation?
|
|
|
|
Crani Sensation?
|
|

