![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
52 Cards in this Set
- Front
- Back
|
what is the leading causes of traumatic death and disability?
|
Traumatic brain injury (TBI) and traumatic spinal cord injury (TSCI)
|
|
|
TBI conditions for which emergency neurosurgery is needed
|
penetrating wounds
intracerebral hemorrhage with mass effect including subdural and epidural blood, bony injury such as displaced fracture, and vertebral subluxation |
|
|
TBI conditions for which emergency neurosurgery is NOT needed
|
focal
hypoxic-anoxic diffuse axonal and diffuse microvascular injuries |
|
|
The initial goals in TBI care are
|
ABCs of airway, breathing, and circulation. Next is D for disability (neurologic).
|
|
|
Every TBI patient should undergo a detailed
|
neurologic examination to ascertain the level of neurologic disability.
|
|
|
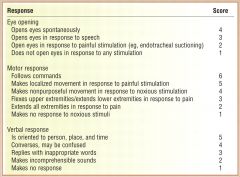
An initial ___________________should be assigned to each TBI patient.
|
Glasgow Coma Score (GCS)
|
|
|
Glasgow Coma Score (GCS) usefulness with TBI patients
|
categorizes TBI patients and provides a quantifiable measure of impairment.
|
|
|
Glasgow Coma Score (GCS)
|
|
|
|
In the early stage of TBI management, it is important to determine ___________
|
the duration of amnesia or loss of consciousness a patient may have experienced
Longer periods of abnormal sensorium are associated with higher grades. Higher grades necessitate longer periods of convalescence. |
|
|
second impact syndrome
|
It is essential that patients have adequate recovery even from mild TBI. A subsequent head injury before full recovery may be catastrophic as it could result in "second impact syndrome" (SIS), which leads to worse clinical outcome including death.
|
|
|
Severe TBI is defined as an injury that results in a GCS score of
|
eight or less
|
|
|
Severe TBI medical management
|
An important early intervention is airway protection, usually by endotracheal intubation.
If elevated intracranial pressure (ICP) is suspected or if GCS < 8, the ICP should be monitored. patient's head should be elevated to 30 degrees and kept midline, with a rigid neck collar used (until the cervical spine can be evaluated for stability). Mannitol should be given intravenously at a dose of 0.5 to 1.0 g/kg. A head CT without contrast should be done as soon as possible both to identify lesions that will require surgery and to determine the extent of injury. |
|
|
postconcussive syndrome
|
A complication of TBI
The most common symptoms are headache, difficulty concentrating, appetite changes, sleep abnormalities, and irritability. In general, this condition lasts only a few weeks after injury. However, uncommonly, it can persist beyond a year or more. Therapies are focused on managing symptoms. For headache, nonsteroidal anti-inflammatory agents, migraine drugs, and biofeedback can be effective. For cognitive dysfunction, neuropsychologic testing may be helpful in determining appropriate intervention. |
|
|
Traumatic Spinal Cord Injury Management begins with
|
therapy begins with the ABCs of airway, breathing, and circulation
|
|
|
For patients with high cervical lesions what will be lost?
|
spontaneous ventilation
|
|
|
Lesions lower than C5 may also be associated with what?
|
insufficient ventilatory capability.
|
|
|
Maintaining adequate ____________ is of particular importance in the spinal cord-injured patient.
|
intravascular volume
Hypotension may result from either neurogenic shock or hypovolemia |
|
|
Neurogenic shock in spinal cord-injured patient management
|
For neurogenic shock, vasopressive pharmacologic agents such as phenylephrine may be needed. If tachycardia is present, then hypovolemia is the more likely cause, and fluid administration is the appropriate initial management.
As with TBI, normal saline is the preferred fluid. |
|
|
Up to 50% of TSCI patients have an associated _____
|
TBI
|
|
|
complaints of pain over the spine or of numbness, tingling, or weakness should raise the suspicion of__________
|
spinal cord injury
|
|
|
complaint of burning hands suggests
|
cervical spinal cord injury
|
|
|
The level of the spinal cord injury is defined as .....
|
the lowest spinal cord segment with intact motor and sensory function.
|
|
|
The prognosis for neurologic improvement is better if the lesion is ________
|
incomplete than if it is complete.
|
|
|
suspected spinal cord injury management
|
patient should be immediately and appropriately immobilized, that is, with a rigid collar or back board or both.
Radiologic evaluation should begin with plain x-ray films of the bony spine. Abnormalities on x-ray films should lead to further neuroimaging. Bony vertebrae should be examined with computed tomography (CT), and the spinal cord with magnetic resonance imaging (MRI). Intervertebral and paravertebral soft tissue are best studied with MRI. A chest radiograph should also be obtained in order to visualize the lower cervical and thoracic vertebrae. Presence of a pleural effusion in the setting of a possible thoracic spine injury suggests a hemothorax. |
|
|
If the C-spine radiograph is normal but the patient complains of neck pain
|
ligamentous injury may be present.
Ligamentous injury is evaluated by flexion-extension C-spine x-ray studies. However, in the acute period, pain may prevent an adequate study. Such patients should be kept in a rigid cervical collar for at least 24 to 48 hours until the pain and neck muscle spasm resolve. At that time, the study may be performed. If abnormal, the patient will need surgical evaluation. |
|
|
Confirmed spinal cord injury management
|
methylprednisolone should be given at an initial dose of 30 mg/kg intravenous bolus followed by a continuous infusion of 5.4 mg/kg/hr.
The infusion should be for 23 hours if it is started within 3 hours of injury. If beyond 3 hours but still within 8 hours, then methylprednisolone should be given for 48 hours. this therapy is reserved only for closed compartment injury (NOT PENETRATING). This is the only indication for steroid use in TSCI. At this time, the decision for surgical intervention should be made, based on the stability of the vertebral column. |
|
|
SPINAL CORD SYNDROMES: Anterior cord syndrome
|
associated with deficits referable to bilateral anterior and lateral spinal cord columns.
There is loss of touch, pain, and temperature sensations and motor function below the level of the lesion. The posterior column functions of proprioception and vibratory sensation remain intact. |
|
|
SPINAL CORD SYNDROMES: Brown-Séquard syndrome
|
the deficits are caused by injury to a lateral half of the cord.
There is functional loss of ipsilateral motor function, touch, proprioception, and vibration sensations, and contralateral pain and temperature sensations. |
|
|
SPINAL CORD SYNDROMES: Central cord syndrome
|
syndrome manifests as motor paralysis of both upper extremities while the lower extremities are spared.
Weakness is greater proximally than distally. Pain and temperature sensations are generally reduced, but proprioception and vibration are spared. |
|
|
SPINAL SHOCK
|
After acute injury, spinal shock may occur, causing a temporary loss of spinal reflexes below the level of injury.
Neurologic examination will reveal loss of deep tendon reflexes, bulbocavernosus reflex, and the anal wink. In high cervical injuries, the lower reflexes (bulbocavernosus and anal wink) may be preserved. there will likely be loss of autonomic reflexes, leading to neurogenic shock, bowel ileus, and urinary retention. |
|
|
"Schiff-Sherrington" phenomenon
|
in which reflexes are affected above the level of injury.
sometimes seen in spinal shock |
|
|
Patients with spinal cord injury are at risk for
|
neurogenic shock and dysautonomia
|
|
|
neurogenic shock and dysautonomia can lead to
|
peripheral vasodilation and hypotension
|
|
|
If spinal cord lesion is at T3 or above then ________ is compromised
|
then sympathetic tone to the heart is compromised.
In this setting, hypotension is accompanied by bradycardia: the classic neurogenic shock triad of bradycardia, hypotension, and peripheral vasodilation. |
|
|
classic neurogenic shock triad
|
bradycardia, hypotension, and peripheral vasodilation.
|
|
|
Therapy for dysautonomia
|
begins by ensuring adequate circulating volume.
The goal is to administer fluids to restore a euvolemic state. Blood should be transfused if the patient is anemic-that is, if the hematocrit is less than 30. If blood is not required, then either colloid (e.g., albumin solutions) or crystalloid (e.g., normal saline) may be used to maintain a central venous pressure (CVP) of 4 to 6 mm Hg. Hypervolemia should be avoided, as this will exacerbate peripheral edema. Once an adequate circulating volume has been achieved, a vasopressive agent such as phenylephrine, norepinephrine, or dopamine can be used. The goal MAP is 85 mm Hg or greater. Symptomatic bradycardia can be treated with atropine. |
|
|
Spinal cord patients are at risk for
|
ventilatory compromise
|
|
|
Patients whose injuries are at C5 or higher typically require
|
mechanical ventilation with an appropriate tidal volume (6 to 10 ml/kg) and Fio2 and mandatory machine-driven rate.
The Fio2 should be set at a value that gives a Po2 of 80 to 100 mm Hg. The rate should be set to give a Pco2 of 40 mm Hg. Positive end-expiratory pressure (PEEP) should also be used to minimize atelectasis. If the patient does not show signs of ventilatory recovery within 2 weeks of intubation, a tracheostomy should be considered. |
|
|
Lesions below C5 may also be associated with
|
with inadequate spontaneous ventilation
|
|
|
Patients with cervical lesions at C6 and below, including the thoracic cord, are generally
|
not mechanical ventilator-dependent.
However, their ventilatory effort may be inadequate, as the thoracic cord innervates intercostal muscles, which are accessory muscles of respiration. Such patients have decreased cough and inability to increase ventilation when needed. This leads to atelectasis and comprised ability to clear secretions, which may lead to pneumonia. These patients may benefit from chest physical therapy. |
|
|
TRAUMATIC SPINAL CORD INJURY MANAGEMENT ISSUES
|
cardiovascular, ventilatory, genitourinary, bowel, infectious disease, nutrition, skin and prophylaxis against skin ulcers, and DVT formation.
|
|
|
TRAUMATIC SPINAL CORD INJURY MANAGEMENT ISSUES: DVT
|
Therefore all patients with TSCI should receive both anticoagulation and leg mechanical compression devices.
As soon as possible, sequential compression devices (SCDs) or compression stockings should be placed on patients. Then, as soon as hemostasis is ensured, low-molecular-weight heparin (LMWH) should be initiated. Unfractionated heparin may also be used in conjunction with SCD, but LMWH is preferred. An inferior vena cava filter may be placed in those patients in whom anticoagulation therapy is contraindicated but should not be the primary means of preventing DVT. |
|
|
TRAUMATIC SPINAL CORD INJURY MANAGEMENT ISSUES: ILEUS
|
A nasogastric tube should be placed to decompress the stomach.
Parenteral nutrition should be started as soon as possible. Enteral feeding should be delayed until gastrointestinal motility returns. This normally takes about 2 to 3 weeks. The pharmacologic agents metoclopramide, erythromycin, and cisapride may promote gastrointestinal motility. |
|
|
TRAUMATIC SPINAL CORD INJURY MANAGEMENT ISSUES: Gastrointestinal
|
Gastric ulcer prophylaxis needs to be administered: H2-receptor antagonists, proton pump inhibitors, antacids, or sucralfate.
Pancreatitis and trauma-related perforated bowel are potential problems. Loss of abdominal muscle tone and visceral sensation may mask clinical signs such as pain, guarding, or rigidity. |
|
|
TRAUMATIC SPINAL CORD INJURY MANAGEMENT ISSUES: GENITOURINARY
|
Bladder tone may be lost because of spinal shock. A Foley catheter should be placed and maintained for a minimum of 5 to 7 days to help drain the bladder and to evaluate circulatory volume and renal function.
After spinal shock has resolved, autonomic dysreflexia may occur from bladder distention. |
|
|
autonomic dysreflexia
|
After spinal shock has resolved, autonomic dysreflexia may occur from bladder distention.
Clinical signs such as sweating, skin flushing, and hypertension may be present. Clinical examination using palpation and percussion will reveal a distended bladder, which can be treated with bladder training or intermittent catheterization. Phenoxybenzamine may be helpful in this condition. |
|
|
TRAUMATIC SPINAL CORD INJURY MANAGEMENT ISSUES: NUTRITION
|
Until enteral feeding can begin, parenteral nutrition should be used.
A caloric level of 80% of the Harris-Benedict prediction, which approximates a patient's total daily energy expenditures, should be used for quadriplegic patients. This is an approximation of a patient's total daily energy expenditure and is based on the patient's basal metabolic rate and activity level. The full Harris-Benedict predicted amount should be used for patients with thoracic spine injuries and below. |
|
|
TRAUMATIC SPINAL CORD INJURY MANAGEMENT ISSUES: DECUBITUS ULCERS
|
There is a propensity for decubitus ulcers from pressure to develop in patients with TSCI.
Mechanical kinetic beds, regular log rolling (every 2 hours), and padded orthotics are all useful in minimizing this complication. |
|
|
TRAUMATIC SPINAL CORD INJURY MANAGEMENT ISSUES: REHABILITATION
|
Orthotics, physical therapy, and occupational therapy (for cervical cord injury) are also important.
Therapy should begin as soon as the spine is stabilized. This will serve to minimize contractures and to begin the rehabilitation process. It should be remembered that once therapy begins, energy expenditures will increase, and consequently additional nutrition will be needed. Also, as intermittent compression devices will need to be removed during therapy, the heparin dose may need to be increased. |
|
|
The most useful prognostic indicator after TBI is
|
the neurologic examination at presentation.
Clearly, the better the neurologic examination findings, the higher the likelihood of improved recovery. |
|
|
Usefulness of GCS as prognostic indicator after TBI
|
The initial GCS is a very reliable prognostic indicator. The lower the initial GCS, the less likely a patient will have meaningful neurologic or functional recovery.
|
|
|
the most useful prognosticator for TSCI
|
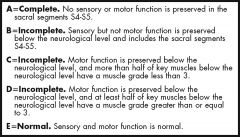
the completeness of the injury
The American Spine Injury Association Impairment Scale grades spinal cord injury on the basis of completeness (Table 125-3). A grade A or complete motor and sensory deficit below the lesion is associated with the most ominous prognosis. If this status persists for longer than 24 hours, there is little reasonable likelihood of meaningful recovery. On the other hand, partial injuries, even severe, have substantial probability of recovery. |

