![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
191 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Temporary or permanent opening produced by a force that pushes body tissues laterally away from the tract of a projectile |
Cavitation |
|
|
|
When does axial loading occur? |
The head strikes the front windshield |
|
|
|
Deformity bilaterally to the hips and bruising to the knees suggests |
Down-and-under injury pathway |
|
|
|
Knives and arrows cause |
Low-energy, low-velocity wounds |
|
|
|
The anticipation of injury to a body region, organ, or structure based on analysis of the MOI |
Index of suspicion |
|
|
|
When analyzing an MVC, remember to examine |
Both the interior and exterior of the vehicle to identify forces expressed to the patient |
|
|
|
If an object is impaled in a pt, the provider stabilizes it with bulky dressing in order to |
Prevent motion of the object and further internal injuries |
|
|
|
Layer of skin that contains nerve endings |
Dermis |
|
|
|
Painful open injuries with a high risk for infection |
Abrasions |
|
|
|
Why is an occlusive dressing used for lacerations and/or wounds of the neck? |
The risk of an air embolus |
|
|
|
If an appendage is amputated, how should it be appropriately handled? |
Wrap it in sterile dressing
|
|
|
|
What is a typical finding with developing compartment syndrome? |
Pain seemingly out of proportion to the injury |
|
|
|
One difference between a hematoma and a contusion is that a hematoma is |
More severe and results in greater blood loss
|
|
|
|
How would a provider describe a 2" linear wound to the top of the head in which the skull can be seen? |
Laceration |
|
|
|
What is the biggest concern with abrasions? |
Infection |
|
|
|
The external layer of skin |
Epidermis |
|
|
|
Middle layer of skin |
Subcutaneous |
|
|
|
Innermost layer of skin |
Dermis |
|
|
|
Assessment of a 2-3 day old wound reveals warmth and lymphangitis. This is indicative of |
Infection |
|
|
|
Red streaks stemming from the site of injury |
Lymphangitis |
|
|
|
During the inflammation phase of wound healing, blood flow to the injured area |
Increases to meet the metabolic demands of the injured tissue |
|
|
|
Loose flap of skin torn from the body |
Avulsion |
|
|
|
When internal bleeding is suspected on an extremity, the provider should include what in treatment? |
Immobilization of the extremity |
|
|
|
On scene of a pt that has "tons of building material compressing her stomach and legs." Extrication will be lengthy. What drug might the provider give to treat this patient? |
Intravenous sodium bicarbonate |
|
|
|
PMS should continually be checked when bandaging a soft-tissue injury. The bandage may fit at first, but then become too tight due to the |
Damaged tissue swelling
|
|
|
|
After wrapping an amputated part in sterile dressing, the next step is to |
Seal the part in a bag, and place it in cool water |
|
|
|
If a pt removes an impaled object prior to arrival, what is the primary concern for pt care? |
Assessing for internal blood loss or shock |
|
|
|
What is the proper treatment for avulsions? |
Return tissue to its normal position and bandage |
|
|
|
What structures prepare an open wound for healing by clearing foreign bodies and dead tissues? |
White blood cells |
|
|
|
Compromised arterial blood flow leads to _______ and can occur when an area of the body is trapped for longer than 4 hours |
Crush syndrome |
|
|
|
An open wound with smooth edges and no flaps of tissue |
Incision |
|
|
|
Heavy bleeding from around an impaled object should be treated by first |
Applying direct pressure around the object |
|
|
|
Once a pt has been trapped for a long amount of time, what can be expected when the pt is freed? |
The pt may deteriorate rapidly due to myoglobin and potassium release from the damaged cells |
|
|
|
The step in the clotting process in which the smooth blood vessel contracts, reducing the vessel lumen |
Vascular phase |
|
|
|
If direct pressure of a wound to an extremity does not stop the bleeding, what is the next appropriate step? |
Applying a tourniquet |
|
|
|
Late decompensated shock is indicated by |
Slowing respiration rate |
|
|
|
A contraindication to the application of the PASG (MAST) is |
Pulmonary edema |
|
|
|
In an otherwise healthy 70kg adult, hypotension is typically noted after how much blood loss? |
More than 1,500mL |
|
|
|
When treating a patient with suspected internal hemorrhage and hypotension, what is most important? |
Rapid transport to a trauma facility |
|
|
|
What are the basic causes of shock? (4) |
1. Pump failure 2. Poor vessel function 3. Low fluid volume 4. Respiratory insufficiency |
|
|
|
Signs of shock are delayed in a pregnant pt due to |
Blood volume being increased in pregnant women |
|
|
|
Neurogenic shock due to head or spinal cord injury creates |
Bradycardia |
|
|
|
The best early indication of possible internal hemorrhage |
A significant mechanism of injury |
|
|
|
Compared to an adult, the blood volume of an infant or young child is proportionately about |
20% greater |
|
|
|
Hypotension, tachycardia, tachypnea, rales, and increased work of breathing in decompensated shock is indicative of what type of shock? |
Cardiogenic shock |
|
|
|
What type of shock does cardiac failure cause? |
Cardiogenic shock |
|
|
|
A pt that is unresponsive, tachycardic, tachypneic, and severely hypotensive is in what stage of shock? |
Decompensated |
|
|
|
What is the first treatment rendered to a pt with suspected shock? |
Airway and ventilatory support |
|
|
|
What happens as shock progresses from compensated to decompensated? |
The precapillary sphincters relax and the postcapillary sphincters remain closed |
|
|
|
As the body compensates for shock with peripheral vasoconstriction, oxygen delivery to the peripheral capillaries decreases, causing |
Increased carbon dioxide and lactic acid production |
|
|
|
A pt that has lost 1L of blood with a BP of 74/56 needs ________ to increase perfusion to the cells |
Increased number of RBCs and plasma |
|
|
|
What are two possible complications of PASG (MAST) |
It pressurizes the abdomen and may reduce chest excursion |
|
|
|
What would you expect to see from a healthy 20YOM that has lost 350mL of blood? |
Slight tachycardia |
|
|
|
Cell death, tissue, dysfunction, and permanent organ damage occur during which stage of shock? |
Irreversible |
|
|
|
The step in clotting where enzymes are released from platelets and surrounding tissues, resulting in fibrin production |
Coagulation phase |
|
|
|
When using a tourniquet, remember that _______ can accumulate. (3) |
1. Lactic acid
2. Potassium 3. Anaerobic metabolites |
|
|
|
If a trauma pt has signs of shock, but no external signs of injury, what should be suspected? |
Retroperitoneal hemorrhage |
|
|
|
How does IV therapy help a pt with massive hemorrhage and hypoperfusion? |
Increases preload |
|
|
|
Your pt has lost about 20% of total blood volume. He is anxious, restless, tachycardic, and has pale, cool, clammy skin. Which phase of hemorrhage is he in? |
Phase 2 |
|
|
|
When tissue perfusion declines, the body reacts immediately to restore and maintain blood flow through |
Sympathetic nervous system stimulation |
|
|
|
How is epistaxis treated? |
Tilt the head forward and pinch the nostrils together |
|
|
|
The goal of of fluid resuscitation in a pt with uncontrolled hemorrhage is to |
Maintain peripheral perfusion
|
|
|
|
A 45YOM is conscious and screaming in pain with bright red blood spurting from his thigh. What is the first step in treatment? |
Control the bleeding |
|
|
|
A serious systemic bacterial infection most commonly causes |
Septic shock |
|
|
|
Trauma center that is research based and has full services available at all times |
Level I Trauma Center |
MCV |
|
|
Trauma center that has most services available at all times; not research based |
Level II Trauma Center |
LGH |
|
|
Trauma center that provides operative intervention for stabilization |
Level III Trauma Center |
DRMC |
|
|
Trauma center that provides initial, non-operative stabilization |
Level IV Trauma Center |
GED |
|
|
Single most important factor in trauma prognosis
|
Time |
|
|
|
Trauma pts need to be from scene to OR within about 60 minutes. The term for this is called |
The Golden Hour |
|
|
|
A body at rest or in motion will stay at rest or in motion until acted on by an outside force |
Newton's first law of motion (inertia) |
|
|
|
Energy cannot be created or destroyed; it can only change form |
Conservation of energy |
|
|
|
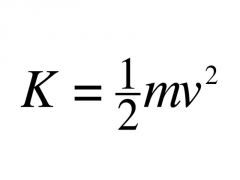
Formula for kinetic energy |
|
|
|
|
Most important factor in determining kinetic energy |
Velocity |
|
|
|
Process of predicting injury patterns based on certain MOIs |
Kinematics |
|
|
|
When one organ moves slower/faster in relation to others |
Shear |
|
|
|
Force directly applied to organ/body part |
Compression |
|
|
|
Spidering to the windshield and steering wheel deformity suggests what type of injury pathway? |
Up-and-over |
|
|
|
What type of injuries would a provider expect to see in up-and over-injuries? |
Head, chest, and abdominal injuries |
|
|
|
What type of collision can lead to C1(Atlas) and C2 (Axis) fx, due to torsion? |
Lateral impact |
|
|
|
What type of collision can lead to hyperextension of the neck, resulting in whiplash? (These pts can be seen with their lipstick on their shirt if bad enough) |
Rear-end impact |
|
|
|
What types of collisions can cause cerebral contusions, brainstem stretch or shear, and skull fx? (2) |
Rotational impact
Rollover impact |
|
|
|
The body stops, but the brain continues to move. It hits the anterior wall of the skull, then bounces back and hits the posterior wall, possibly several times before stopping |
Coup countercoup injury |
|
|
|
Aorta twists and tears due to deceleration |
Aortic shear |
|
|
|
In pedestrian vs. motor vehicle collisions, what injuries would a provider expect to see in an adult pt? (6) |
1. Pelvis 2. Femur 3. Thorax 4. Spine 5. Head 6. Neck |
|
|
|
When an adult pedestrian is hit in pedestrian vs. motor vehicle collisions, where is the pt normally thrown? |
Up and over |
|
|
|
When a pediatric pedestrian is hit in pedestrian vs. motor vehicle collisions, where is the pt normally thrown? |
Down and under |
|
|
|
In pedestrian vs. motor vehicle collisions, what injuries would a provider expect to see in an pediatric pt? |
Any injury superior to the hips |
|
|
|
Fx femur, intra-abdominal or intrathoracic injury, and head injury comprise |
Waddell's Triad |
|
|
|
Explosives that produce supersonic over-pressurization shockwave |
High-order explosives |
|
|
|
Explosives that produce a subsonic explosion |
Low-order explosives |
|
|
|
Blast injury caused by initial shockwave |
Primary blast injury |
|
|
|
Blast injury caused by flying debris |
Secondary blast injury |
|
|
|
Blast injury caused by pt striking a stationary object |
Tertiary blast injury |
|
|
|
Blast injury caused by environmental effects of explosion, such as structural fires or building collapse |
Quaternary blast injury |
|
|
|
Knives, arrows, pencils, and other pointy things deliver what type of wound? |
Low velocity |
|
|
|
Small caliber bullets that tumble and bounce deliver what type of wound? |
Medium velocity |
|
|
|
Higher caliber bullets deliver what type of wound? |
High velocity |
|
|
|
In assessing a GSW pt, the provider notices burn marks around a circular bullet wound. How close would the provider assume the assailant was to the pt? |
Close range, if not point-blank |
|
|
|
If a lap belt is worn above the hips, the pt is more susceptible to severe injuries of the |
Abdomen |
|
|
|
According to the CDC, what is the leading cause of death in children aged 1-9? |
MVC |
|
|
|
When deceleration forces are applied to the body, the ligamentum arteriosum often causes fatal injury to |
The liver |
|
|
|
Compression injuries to the thorax that rupture the lungs |
Paper bag effect |
|
|
|
Physical injury or wound caused by an external force |
Trauma |
|
|
|
The most lethal explosions are those |
In confined spaces |
|
|
|
The most common and serious injury associated with explosions |
Lung injuries |
|
|
|
The drainage of blood to the point life cannot be sustained |
Exsanguination |
|
|
|
The five types of vehicle impact |
1. Frontal 2. Lateral 3. Rotational 4. Rear-end 5. Rollover |
|
|
|
The application of the forces of trauma along the axis of the spine |
Axial loading |
|
|
|
The region of a vehicle designed to absorb the energy of impact |
Crumple zone |
|
|
|
The five events of motor vehicle collision |
1. Vehicle collision (car hits object) 2. Body collision (Person hits interior) 3. Organ collision (Organs hit person) 4. Secondary collision (Stuff in the car hits person) 5. Additional impacts (If car hits anything else) |
|
|
|
Size and shape of a projectile as it contacts a target. |
Profile |
|
|
|
Path a projectile follows |
Trajectory |
|
|
|
Forces acting on a projectile in motion to slow its progress |
Drag |
|
|
|
The damage pathway that a high-velocity projectile inflicts results from: (3) |
1. Direct injury 2. Pressure shockwave 3. Cavitation |
|
|
|
The filling of the pericardial sac with fluid |
Pericardial tamponade |
|
|
|
Largest body cavity; contains most of the internal organs
|
Abdominal cavity |
|
|
|
Surgical incision to provide an emergency airway |
Cricothyrotomy |
|
|
|
Introduction of a needle to provide an emergency airway |
Cricothyrostomy |
|
|
|
Largest organ of the body |
Skin |
|
|
|
Glands in the dermis that excrete oil |
Sebaceous glands |
|
|
|
Connective tissue that connects bones to other bones |
Ligaments |
|
|
|
Connective tissue that connects muscles to bones or other muscles |
Tendons |
|
|
|
Stage of wound healing that generates fibrin and forms a plug in the damaged vessel |
Coagulation |
|
|
|
If wounds have significant devitalized tissue are considered |
High-risk wounds |
|
|
|
Excessive accumulation of scar tissue that extends beyond original wound borders |
Keloid scar |
|
|
|
Excessive accumulation of scar tissue that stays within original wound borders (more common) |
Hypertrophic scar
|
|
|
|
Rupture of small blood vessels and damage to cells within dermis; causes ecchymosis |
Contusion |
|
|
|
Large amounts of tissue damaged or large veins/arteries damaged; can have blood loss >1L |
Hematoma |
|
|
|
Ligaments are stretched |
Sprain |
|
|
|
Muscle or tendons are stretched |
Strain |
|
|
|
Linear open wound with jagged edges |
Laceration |
|
|
|
Linear open wound with smooth edges |
Incision |
|
|
|
Wound in which a flap of tissue is torn from skin; may still be partially intact or completely torn off the body |
Avulsion
|
|
|
|
Complete removal of extremity or appendages |
Amputation |
|
|
|
Intestines protruding from abdominal cavity |
Evisceration |
|
|
|
Toxins rush back into the body following crush injury or compartment syndrome |
Rhabdomyolysis |
|
|
|
Circumferential burns, thermal injuries, or frostbite can lead to |
Compartment syndrome
|
|
|
|
"Six Ps" to diagnose compartment syndrome |
1. Pain out of proportion to injury 2. Paresthesia (Pins and needles) 3. Paralysis 4. Puffiness 5. Pallor 6. Pulselessness (late sign, if a sign at all) |
|
|
|
Infected hair follicle |
Folliculitis |
|
|
|
Spread of folliculitis |
Furuncles |
|
|
|
Several furuncles; usual caused by Staphylococcus aureus bacteria |
Carbuncles |
|
|
|
Life-threatening Clostridium infection |
Gas gangrene |
|
|
|
Most common serious complication involved with human and animal bites |
Infection
|
|
|
|
Stepping on a rusty nail increases a pt's exposure to |
Tetanus |
|
|
|
Outermost layer of a blood vessel (except capillaries) |
Tunica adventitia |
|
|
|
Middle layer of a blood vessel (except capillaries) |
Tunica media |
|
|
|
Innermost layer of a blood vessel (except capillaries) |
Tunica intima |
|
|
|
Thick, fibrous, inflexible membranes surrounding muscle that help bind muscle groups together |
Fascia |
|
|
|
How tightly should a tourniquet be applied? |
Until distal pulses are lost |
|
|
|
Impaled objects should not be removed unless the object is impaled |
In the central chest of a pt that needs CPR |
|
|
|
Fatty secretion that keeps skin pliable and waterproof |
Sebum |
|
|
|
General reddening of the skin due to dilation of the superficial capillaries |
Erythema |
|
|
|
Tough, strong protein that comprises most of the body's connective tissue |
Collagen |
|
|
|
New growth of capillaries in response to healing |
Neovascularization |
|
|
|
First sign of hemothorax |
Signs of shock |
|
|
|
Back pressure into the the esophageal veins that produce a bloody mess. |
Esophageal varices |
|
|
|
Phase in the clotting process in which vasoconstriction and vessel retraction occurs |
Vascular phase |
|
|
|
Phase in the clotting process in which turbulent blood flow causes friction damage to platelets, resulting in formation of an unstable clot |
Platelet phase |
|
|
|
Phase in the clotting process in which fibrin is produced, forming a durable clot |
Coagulation phase |
|
|
|
Platelets stick to collagen, tunica intima, and other injured tissue |
Agglutination |
|
|
|
Collection of platelets to each other to form initial clot |
Aggregation |
|
|
|
Bright red blood that may spurt from the wound |
Arterial bleeding |
|
|
|
Dark red blood that flows slowly and steadily |
Venous bleeding |
|
|
|
Blood that is bright to medium red and oozes slowly |
Capillary bleeding |
|
|
|
How often should a person get a tetanus booster? |
Every 10 years |
|
|
|
How should a provider control the bleeding of a gaping wound, provided it is not on the head or neck? |
Pack it to give more uniform pressure |
|
|
|
Medical term for a nosebleed |
Epistaxis |
|
|
|
Cavity that houses the kidneys, aorta, vena cava, and most of the pancreas in which 2-3L of blood can be lost without any signs or symptoms (other than shock) |
Retroperitoneal cavity |
|
|
|
Medical term for coughing up blood |
Hemoptysis |
|
|
|
Medical term for throwing up blood |
Hematemesis |
|
|
|
Medical term for bright red stool |
Hematochezia |
|
|
|
Medical term for dark, tarry stool |
Melena |
|
|
|
Inadequate tissue perfusion caused by insufficient vascular volume |
Hypovolemic shock |
|
|
|
3 stages of shock |
1. Compensated 2. Decompensated 3. Irreversible |
|
|
|
Stage of hemorrhage in which there is <15% loss of CBV |
Stage 1 |
|
|
|
Stage of hemorrhage in which there is 15-30% loss of CBV; compensation occurs in this stage |
Stage 2 |
|
|
|
Stage of hemorrhage in which there is 30-45% loss of CBV; the body is decompensating in this stage |
Stage 3 |
|
|
|
Stage of hemorrhage in which there is >45% loss of CBV; the body enters irreversible shock at this point |
Stage 4 |
|
|
|
What are the eight shock treatments? |
1. Establish patent airway 2. Ensure proper ventilation 3. Oxygen 4. Control bleeding 5. Maintain body temperature 6. Proper positioning (NOT Trendelenburg) 7. Transport 8. IV Access |
|
|
|
What is hypoperfusion caused by an impaired pump (decreased cardiac output, increased tissue perfusion) |
Cardiogenic shock |
|
|
|
In cardiogenic shock, a pt must present with at least one of two signs. What are the two signs? |
1. Hypotension 2. Altered mental status |
|
|
|
What are the three legs of Beck's Triad for cardiogenic shock? |
1. JVD 2. Hypotension 3. Muffled heart sounds |
|
|
|
Shock caused by something putting pressure on the chest, preventing blood return |
Obstructive shock
|
|
|
|
What are the four main causes of obstructive shock? |
1. Cardiac tamponade 2. Tension pneumothorax 3. Massive pulmonary embolism 4. Obstruction of blood flow to the heart |
|
|
|
Ventilation and perfusion are not equal due to pulmonary embolus |
V/Q Mismatch |
|
|
|
Hypoperfusion due to vasodilation |
Distributive shock |
|
|
|
Distributive shock caused by a bacterial infection |
Septic shock |
|
|
|
Distributive shock caused by disruption in the autonomic nervous system |
Neurogenic shock |
|
|
|
Distributive shock caused by allergic reaction |
Anaphylactic shock |
|
|
|
Shock in which the heart, volume, and container are all intact, but O2 cannot reach cells |
Dissociative shock |
|

