![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
101 Cards in this Set
- Front
- Back
|
Carolina Jessamine
|

Name this plant.
|
|
|
Carolina Jessamine
|

Name this plant.
|
|
|
Carolina Jessamine
|

Name this plant.
|
|
|
Carolina Jessamine
|

Name this plant.
|
|
|
Carolina Jessamine
|

Name this plant.
|
|
|
Carolina Jessamine
|

Name this plant.
|
|
|
Carolina Jessamine
|

Name this plant.
|
|
|
Jimson Weed
|

Name this plant.
|
|
|
Jimson Weed
|

Name this plant.
|
|
|
Jimson Weed
|

Name this plant.
|
|
|
Jimson Weed
|

Name this plant.
|
|
|
Jimson Weed
|

Name this plant.
|
|
|
Jimson Weed
|

Name this plant.
|
|
|
Lantana
|

Name this plant.
|
|
|
Lantana
|

Name this plant.
|
|
|
Lantana
|

Name this plant.
|
|
|
Lantana
|

Name this plant.
|
|
|
Lantana
|
Name this plant.
|
|
|
Lobelia
|

Name this plant.
|
|
|
Lobelia
|

Name this plant.
|
|
|
Poison Hemlock
|

Name this plant.
|
|
|
Poison Hemlock
|

Name this plant.
|
|
|
Poison Hemlock
|

Name this plant.
|
|
|
Poison Hemlock
|

Name this plant.
|
|
|
Tobacco
|

Name this plant.
|
|
|
Tobacco
|

Name this plant.
|
|
|
Tobacco
|

Name this plant.
|
|
|
Tobacco
|

Name this plant.
|
|
|
Tobacco
|

Name this plant.
|
|
|
Tobacco
|

Name this plant.
|
|
|
Tobacco
|

Name this plant.
|
|
|
Tobacco
|

Name this plant.
|
|
|
Tobacco
|

Name this plant.
|
|
|
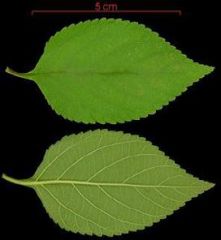
Water Hemlock
|

Name this plant.
|
|
|
Water Hemlock
|

Name this plant.
|
|
|
Water Hemlock
|

Name this plant.
|
|
|
Water Hemlock
|

Name this plant.
|
|
|
Water Hemlock
|

Name this plant.
|
|
|
Water Hemlock
|
Name this plant.
|
|
|
Water Hemlock
|

Name this plant.
|
|
|
Water Hemlock
|

Name this plant.
|
|
|
Water Hemlock
|

Name this plant.
|
|
|
Poison Hemlock
|

Name this plant.
|
|
|
Lantana
a. toxic principle b. conditions of poisoning c. species most often affected |
a. lantanin (a triterpenoid: alcohol derivative), & other GI irritating compounds
b. many poisoning occur when clippings are thrown into pastures c. cattle |
|
|
Lantana
a. signs of acute toxicosis b. signs of chronic toxicosis c. tx |
a. uncommon (would have to eat A LOT at once)
- usually occurs w/in 24 hrs of ingestions - signs: gastroenteritis w/ bloody, watery feces, severe weakness, paralysis, death in 3-4 days b. more common d/t long term grazing --> hepatobiliary necrosis - signs: icterus, photosensitization (2º to liver damage), ulcerations of mm of nose & oral cavity c. prevent exposure: herbicides - symptomatic tx in livestock - gastric decontamination if acute exposure |
|
|
Pyrrolizidine Alkaloids
a. common species of plants b. mechanism of action |
a. Senecio sp. (tansy ragwort), Heliotropium europaeum, Crotalaria sp. (often grows w/ grains; small: could be mixed into bread)
b. induce irreversible liver damage - metabolized into reactive intermediates: can bind to DNA, proteins, etc. (DNA alkylating agent) - most metabolism occurs in liver & most metabolites remain in liver --> multinucleated hepatocytes (megalocytes) |
|
|
Pyrrolizidine Alkaloids
a. signs b. prevention |
a. acute poisoning uncommon in animals
veno-occlusive dz: recognized in children in 1950s (source: contaminated grain or bread) - abdominal distension, hepatomegaly, ascites, edema, jaundice - lesions: centrilobular hepatic congestion & necrosis --> hepatic failure - acute, subacute, or chronic syndrome - recovery can occur w/in 1-2 mos. - chronic form: cirrhosis may persist b. good management techniques |
|
|
What are the toxic principles & mechanisms of action for Amanita?
|
bicyclic octapeptide amatoxins: small peptides
- primarily a liver toxin, but cause intestinal damage d/t enterohepatic recirculation - binds to RNA polymerase-B --> prevents formation of phosphodiesterase bond & subsequent RNA, DNA, & protein synthesis --> liver failure bicyclic heptapeptides phallotoxins - bind to actin-like protein in cell mems of hepatocytes --> loss of mem integrity --> release of intracellular enzymes & potassium |
|
|
Amanita
a. clinical signs b. dx c. tx |
a. 6-24 hrs after ingestion: severe abdominal pain, vomiting, blood diarrhea (often resolves w/in 24 hrs)
- hepatorenal phase (3-4 days after ingestion): icterus, hypoglycemia, delirium, coma - high mortality rate: 10% b. fecal float: can look for tiny seeds from 'shrooms c. acute exposure: emetic + AC - tx for liver failure |
|
|
Aflatoxin
a. toxicity b. mechanisms of action |
a. 2º mold metabolite produced by some strains of Aspergillus flavus & A. parasiticus
- produced at high moisture conc. & warm temps: peanuts, corn, walnuts, pecans, almonds, cottonseed & grain sorghum b. potent hepatotoxins & hepatocarcinogens, interfere w/ RNA transcription, inhibit RNA polymerase, alter lysosomal membranes, stimulate RNA alkylation, impair protein synthesis |
|
|
Aflatoxin
a. factors affecting animals' sensitivity b. clinical signs c. lesions |
a. - young animals more sensitive than adults
- ducklings (most sensitive), trout, dogs, pigs, cattle, sheep, chickens b. early: ↓ feed efficiency & growth rate, ↓ feed intake, unthriftiness, dull hair coat, ↑ prevalence of infectious dz (d/t immunosuppression) - chronic exposure: hepatic failure --> ascites, hemorrhage (lack of clotting factors), icterus, seizures (hepatic encephalopathy) c. histopath: biliary hyperplasia, hepatocellular swelling, hepatic lipidosis --> vacuolization, tumors - gross: icterus, ascites +/- fibrin, intestinal hemorrhage, SQ & muscular hemorrhage |
|
|
Aflatoxin
a. dx b. tx |
a. if you see stunted growth, immunosuppression, & liver damage: think AFLATOXIN
- appearance of corn does NOT help in dx - black light screening of corn: many false positive, but few false negatives: fluoresces d/t presence of a derivative of kojic acid - follow up positives w/ lab analysis for aflatoxins - ELISA: field test - herds: epidemic of liver failure b. change to aflatoxin free ration - ↑ dietary protein: may bind aflatoxin -could use AC - vitamin B12 (B12 dependent enzymes in liver), vitamin K, selenium supplementation: all support liver function |
|
|
Phenol
a. mechanisms of action b. species most often affected c. sources |
a. phenols are protoplasmic poisons causing coagulation necrosis of many tissues
- capillary damage, hepatorenal necrosis, & neurotoxicity may occur - corrosive b. swine, small animals - cat: more sensitive b/c phenol metabolism heavily driven by glutathione transformation c. household disinfectants, coal tar, clay pigeons, solvent, chemical peels |
|
|
Phenol
a. clinical signs b. lesions |
a. dermal exposure: white discoloration of skin or mm, stimulation of respiratory center --> respiratory alkalosis
- inhalation: ataxia, muscle fasciculations - VERY hepatotoxic when ingested - seizures, coma, death: less common - icterus, +/- hemolysis, +/- methemoglobinemia, renal failure b. enlarged, mottle, friable liver & abdominal l.n. - centrilobular hyperemia, fatty degeneration, & necrosis of liver - generalized icterus - corrosive effects in oral cavity & upper GI tract - histo: renal tubular degeneration & necrosis |
|
|
Phenol
a. dx b. tx |
a. clinical signs, lesions, hx of exposure
- serum, urine, or kidney can be analyzed for presence of phenol b. emetics &/or gastric lavage, AC + saline cathartic: emesis indicated despite fact that phenol is a corrosive: most cleaners contain a low conc. (2-5%) which is not labeled as corrosive - oral exposure: demulcents (ex. milk, egg) to protect mm from further damage - dermal exposure: bathe animal w/ mild liquid dish detergent - respiratory support & control of shock & metabolic acidosis - fluids - manage methemoglobinemia |
|
|
Formaldehyde
a. clinical course similar to ________ b. tx |
a. phenol
b. aggressive tx required: gastrotomy to remove material (doesn’t digest well) |
|
|
Delphinium
a. toxic principle & mechanism of action b. conditions of toxicity c. species most commonly affected |
a. methyllycaconitine: polycyclic diterpene alkaloid
- neuromuscular blocking agent: acts at postsynaptic nicotinic receptors in CNS & at NM junctions b. most poisoning occur in Western US: causes more cattle loses than any other plant on western ranges - horses & sheep rarely affected - poisoning rare after flowering & generally occur in spring & fall - dried plant remains poisonous c. cattle |
|
|
Delphinium
a. clinical signs b. lesions |
a. most common sign in cattle: sudden death
- hyperirritability, confusion, mild muscle tremors, stiffness, weakness, collapse, prostration, seizures - inhalation pneumonia common in recumbent animals as a result of vomiting - may see constipation, bloat, oral irritation, regurgitation, salivation - death results from respiratory paralysis or bloat, as animals often fall into recumbency w/ head downhill: usually occurs w/in 3-4 hrs. of ingestion b. ruminal bloat, venous congestion, aspiration pneumonia, GI inflammation |
|
|
Delphinium
a. tx b. prevention c. px |
a. AC + saline cathartic
- physostigmine IV: best if given early, repeated injections generally necessary - turn so head is uphill - relieve bloat - ABs for aspiration pneumonia - move animals to new pasture b. spot spraying of delphinium w/ herbicides, followed by attempts to revegetate w/ other types of plants (ex. grass) c. guarded, even if mildly affected |
|
|
Sweet Pea
a. conditions of poisoning b. toxic principle |
a. grows well in poor soil & under extreme drought conditions: India, Africa
- horses consuming exclusive diet of sweet pea seeds would show signs in ~10 days - if ingesting 1-2 quarts of seeds/day, signs delayed for 2-3 mo. - signs may appear a month or more after withdrawal of seeds from diet b. β-N-oxalyl-L-α-β-di-aminopropionic acid: mainly in pea or seed - converted in vivo to β-aminoproprionitrile - heat labile: can be destroyed by cooking |
|
|
Sweet Pea
a. clinical signs b. lesions c. tx d. px |
a. assoc. w/ neurolathyrism in humans & other animals & osteolathyrism in livestock
- cattle: lameness after 3-5 d. of consumption - other animals: paralysis, slow, weak pulse, depression, weak respiration, convulsions - horse: hopping gait, stiffness in hindquarters, head held low, “roaring” d/t paralysis of recurrent laryngeal n. b. horse: neuronal degeneration in spinal cord & nerves to hind legs c. gastric lavage, AC + saline cathartic, supportive therapy d. some animals make full recovery, others are chronically affected |
|
|
Sorghum
a. toxic principle b. conditions of poisoning c. species most commonly affected |
a. β-cyanoalanine --> ataxia, may also contain cyanogenic glycosides, nitrate
- nitrate accumulation --> methemoglobinemia in cattle (NOT horses) b. assoc. w/ chronic grazing of hybrid Sudan pastures: poisoning develops w/in 1 wk – 6 mo. - more toxic when high rainfall - hay must be freshly cut to be poisonous c. horses |
|
|
Sorghum
a. clinical signs b. teratogenesis c. lesions |
a. posterior ataxia, +/- flaccid paralysis of hind limbs (ddx: equine wobblers)
- winking, urinary incontinence, urine scalding, mares may appear to be in constant estrus 2º to urethral & vaginal irritation, cystitis - males may constantly dribble urine b. mares that graze hybrid sudans during gestation days 20-50 --> dystocia, abortion, foals may be born w/ extreme joint flexion or ankylosis c. cystitis, hyperemic bladder mucosa, ureter, & vagina, +/- bladder mucosal ulceration, pyelonephritis - neuronal degeneration & mild myelomalacia - foals: arthrogryposis |
|
|
Sorghum
a. clin path findings b. tx c. px |
a. leukocytosis, lymphocytosis, proteinuria, calcium carbonate crystalluria (d/t urine pooling in bladder, hyaline & granular casts, urine culture (E. coli, Corynebacterium, Staph, Proteus vulgaris &/or Pseudomonoas aeruginosa)
b. change diet from hay to grain - +/- ABs for cystitis: signs generally recur in 1-2 wks after therapy is stopped c. once animal exhibits ataxia or dribbling of urine, complete recovery seldom if ever occurs |
|
|
Tobacco
a. toxic principle b. clinical signs of acute ingestion c. teratogenesis d. tx |
a. nicotine-like pyridine alkaloids in all parts of plant (nicotine receptor agonists)
b. nicotinic signs: muscle twitching, weakness, diarrhea, vomiting, abdominal pain, dyspnea, death d/t resp. paralysis c. teratogenic agent: anabasine - pigs: consumption b’twn gestation days 10-35: arthrogryposis, cleft palate - cows: cleft palate d. emetic + AC if recent exposure - resp. paralysis NOT permanent: could put on ventilator if needed |
|
|
Lobelia
a. toxic principle b. species most commonly affected |
a. pyridine alkaloids similar to nicotine (lobeline, lobelidine)
- stimulate carotid body chemoreceptor - nicotinic receptor agonist - initially respiratory stimulant, then respiratory depressant b. sheep, cattle, goats |
|
|
Lobelia
a. clinical signs b. lesions c. tx |
a. sluggishness, salivation, diarrhea, anorexia, nasal secretion or hemorrhage, oral ulcers, dilation of pupils, coma
b. widely distributed hemorrhage, mild gastroenteritis - L. berlandieri: SQ hemorrhage, subdural edema, brain congestion c. - emetics/gastric or rumen lavage + AC & cathartic - respiratory support if needed - tx seizures w/ diazepam |
|
|
Poison Hemlock
a. toxic principle b. species most commonly affected |
a. piperidine alkaloids (coniine): mode of action similar to nicotine
b. cows > horses > sheep; also poultry, swine |
|
|
Poison Hemlock
a. clinical signs b. teratogenesis c. tx |
a. tremors, ataxia, mydriasis, coma, death, cardiac arrhythmias
b. limb deformities, hydrocephalus, cleft palate (pigs) c. emetic + AC, supportive care |
|
|
Carolina Jessamine
a. toxic principle b. clinical signs c. lesions |
a. alkaloids gelsemine & gelsemicine
b. progressive weakness, convulsions, seizures, hind limb paresis, muscle tremors, ataxia c. mild diffuse neuronal degeneration, cerebellar Purkinje cell loss, multifocal vacuolation of brain stem & cerebral white matter |
|
|
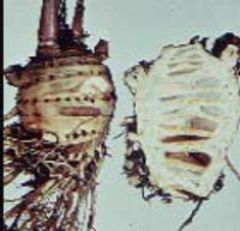
How can poison hemlock & water hemlock be distinguished by appearance?
|
Poison Hemlock: spotted root w/ open chamber, white flower, 3-4’ when full grown
Water Hemlock: spotted stem, multi-chambered root, found in swampy areas & marshes (one of most poisonous plants in US) |
|
|
Water Hemlock
a. toxic principle b. clinical signs c. tx d. px |
a. cicutoxin (unsaturated alcohol)
b. rapid onset: 30 min. – 2 hrs - salivation, abdominal pain, muscle tremors, seizures, death d/t resp. failure c. control seizures d. if animal survives for 2 hr. after onset, generally good px |
|
|
Jimson Weed
a. toxic principle b. conditions of poisoning c. clinical signs d. tx e. px |
a. belladonna alkaloids (ex. atropine): muscarinic receptor blockade
b. seed contamination of grain, plant contamination of forage c. atropine-like effects: tachycardia, dry skin, ↓ salivation, mydriasis (can occur from topical contact & could be unilateral), blurred vision, hyperthermia; ↓ feed consumption d. physostigmine: short acting - signs likely to resolve w/in 24 hrs w/o tx e. no long term effects |
|
|
Atropine
a. effects in horses b. clinical signs of OD in small animals c. tx of OD in small animals |
a. gut stasis, colic
b. muscle tremors, hyperthermia (d/t muscle tremors), hyperactivity c. cage rest 18-24 hrs: no meds - don’t give phenothiazine tranquilizers: ↓ seizure threshold - if tranquilization required: valium |
|
|
Yellow Star Thistle
a. toxic principle b. species most commonly affected c. conditions of poisoning |
a. unknown
b. horses c. primarily in western US - fresh plant usually not toxic: must be dried - most horses develop signs after 30-90 days grazing on contaminated pastures - signs begin after consumption of several hundred pounds of these weeds |
|
|
Yellow Star Thistle
a. clinical signs b. lesions c. tx d. px |
a. wt. loss (may be 1st sign noticed), hypertonicity of facial muscles, tongue lolling, unable to prehend or swallow food, mouth open w/ tongue protruding, head tossing, anorexia, may immerse head in water to drink, death 2º to starvation
b. nigropallidoencephalomalacia (substantia nigra, globus pallidus): usually bilaterally symmetrical c. none d. poor |
|
|
Locoweeds
a. species of plants b. species most commonly affected c. tx |
a. Astragalus spp, Oxytropis sericea
b. cattle, sheep, horses c. none |
|
|
Describe the 3 toxic principles & 3 related syndromes caused by locoweeds.
|
nitro-containing compounds: miserotoxin
- miserotoxin broken down in rumen into organic nitrite - nitrite + Hg --> methemoglobin --> dyspnea - clinical signs occur w/in 24 hrs: weakness, knuckling at fetlocks, interference b’twn hind limbs as animal moves (“cracker heels”), cyanosis, collapse, death selenium: naturally occurring essential metalloid (anti-oxidant) - deficiency: cardiomyopathy (white muscle dz), bleeding disorder in poultry - toxicity: problem in areas w/ high selenium levels in soil (western US) --> selenium accumulation in plants - acute selenosis: rarely occurs d/t plants, may occur w/ contaminated water - subacute selenosis (“blind staggers”) - chronic selenosis (alkali dz): most common - hair loss, initially from mane & tail - deformation & cracking of hoof walls --> sloughing of hoof - cracking & ridging of horns in cattle - teratogenicity in birds: impairs beak formation swainsonine (alkaloid): causes typical signs of “locoism” - livestock must graze plant for long periods before signs occur - inhibits α-D-mannosidase --> vacuoles in neurons that contain abnormal amts. of mannose rich oligosaccharides - clinical signs: CNS depression, slow staggering gait, rough hair coat, dull eyes w/ a staring look, emaciation, ataxia, nervousness - teratogenesis: ↓ fertility, abortion, skeletal deformities (cattle, sheep) |
|
|
Avocado
a. toxic principle b. clinical signs c. syndrome in caged birds |
a. unknown
b. severe mastitis in many species, incl. rabbits, cattle, goats, horses, birds, fish - high doses can cause edema & cardiomyopathy c. signs occur w/in 24 hrs of ingestion - respiratory distress, hydropericardium, generalized edema - some birds get cerebral edema --> neuro signs |
|
|
Fumonisins
a. mechanism of action b. factors that affect toxin production c. susceptible species |
a. inhibits sphingosine N-acyltransferase --> ↑ sphingosine conc. in tissues --> cytotoxicity (neurons, hepatocytes, etc.), damage to hepatocyte membranes
- sphingosine is an important 2nd messenger b. mycotoxins produced by fungus Fusarium moniliforme - fumonisin B1: dominant toxin - stressors on plant promote production of mycotoxin by fungus: doesn’t always produce toxin - risk factors: midsummer drought, wet fall, fluctuating warm & cold temps, early frost, delayed harvests - corn may appear grossly normal c. horses, donkeys, swine, rabbits (renal failure) |
|
|
Fumonisins
a. clinical signs in horses b. lesions in horses c. clinical signs in pigs d. lesions in pigs |
a. onset of signs: usually 14-21 days after new batch of corn is 1st fed (may be as early as 7 d. or as last as 90 d.)
- multiple horse outbreak: morbidity < 25%, but mortality approaches 100% in affected animals leukoencephalomalacia - early: anorexia - CNS depression, ataxia, blindness (usually unilateral), “hysteria”, convulsions - head held low, reluctance to move, paralysis of lips & tongue, inability to prehend & chew food, head pressing (d/t cerebral edema), marked stupor, hyperesthesia - death may occur w/o any signs hepatotoxic syndrome - usually 5-10 d. b’twn onset & death - icterus, hepatic degeneration, facial edema, oral petechia, hepatic encephalopathy, ↑ bilirubin, ↑ liver enzymes b. liquefactive necrosis in white matter, 1º hepatocellular dz w/ 2º hepatic encephalopathy c. ↓ feed consumption, +/- acute pulmonary edema (may be delayed for up to 7 d.), +/- slowly progressive liver dz, death d. severe pulmonary edema & hydrothorax |
|
|
Fumonisins
a. dx b. tx c. px |
a. presence of F. moniliforme on corn is NOT diagnostic: only supportive
- multiple animals affected - hx of ingestion of corn, signs & lesions - ELISA: detection of ~10 ppm fumonisin in horse feed or 50 ppm in swine feed b. careful: horse may be dangerous (crazed) - no known effective therapy - thiamine: general supportive tx for neuro conditions, not specific - AC: usually not used - change of diet: avoid corn - supportive care, quiet surroundings c. poor |
|
|
Organophosphates/Carbamates
a. mechanism of action b. clinical signs c. examples of OPs d. example of a carbamate |
a. acetylcholinesterase inhibitors
- carbamate: carbamylation of acetylcholinesterase (reversible) - OPs: phosphorylation of acetylcholinesterase (“aging”): irreversible - aging occurs over a 12-24 hr. period - buildup of Ach in synaptic cleft --> overstimulation of muscarinic & nicotinic receptors b. related to excessive stimulation of nicotinic & muscarinic receptors - muscarinic effects: salivation, lacrimation, urination, defecation (SLUD: appears w/in minutes & dissipates quickly), CNS signs, bronchospasm, ↑ bronchial secretions - nicotinic effects: muscle tremors, CNS signs, respiratory paralysis - additional signs: colic (horses), diarrhea, +/- miosis, bradycardia c. parathion, chlorpyrifos d. carbaryl |
|
|
How would one diagnosis OP/carbamate toxicosis?
|
hx of exposure, clinical signs
evaluation of acetylcholinesterase activity: brain, retina, blood, plasma, or serum - inhibition > 50%: indicative of poisoning - inhibition > 75% & compatible signs: diagnostic - normals are very species specific: submit sample from patient & “control” (non-affected) animal - cats: prone to develop reduced whole blood acetylcholinesterase activity following exposure, blood also higher in pseudocholinesterase: less prognostic than in other species - long incubation time may result in reversal of activity for carbamates atropine test dose - give a pre-anesthetic dose of atropine (0.02 mg/kg) - if muscarinic signs diminish, then OP/carbamate poisoning is UNLIKELY chemical analysis: brain, liver, kidney, stomach contents, skin (dermal exposure), suspected sources (feed, water) |
|
|
What is the tx & px for OP/carbamate toxicosis?
|
aggressive therapy needed in many cases
stabilize 1st antagonists atropine: reverse muscarinic signs (0.1-0.2 mg/kg IV, SQ, or IM) - evaluate animals for miosis, bradycardia, dyspnea - can cause GI stasis in horses! - be sure of dx before treating: this dose of atropine in non-affected animals can cause atropine toxicosis antidotes pralidoximine chloride (2-PAM) - regenerates acetylcholinesterase by allowing its release from OP - only effective if aging (ex. covalent phosphorylation) has NOT occurred - not effective w/ carbamates: can actually make toxic syndrome worse - given IV IM q 4-6 hrs: discontinue if no benefit observed after 36 hrs - should see improved mental status, ↓ muscle tremors following stabilization - GI decontamination: AC, gastric/rumen lavage - bathe animal if dermal exposure: mild detergent shampoo px: long term recovery following OP exposure depends on resynthesis of acetylcholinesterase: requires 2-4 wks - depends on agent: chlorpyrifos assoc. w/ long-term effects: delayed neuropathy seen rarely in cats, water buffalo, chickens |
|
|
Nightshade
a. toxic principle b. clinical signs c. tx for neuro signs |
a. solanine (alkaloid), plus several other alkaloids: weak acetycholinesterase inhibitor
b. GI irritation --> bloat, anorexia, vomiting, abdominal pain, diarrhea, pyrexia - acetylcholinesterase inhibition --> SLUD, muscle tremors c. atropine (NOT 2-PAM), supportive care |
|
|
Pyrethrin & Pyrethroids
a. source of pyrethrin b. species commonly affected c. toxicity d. mechanism of action |
a. naturally derived from chrysanthemums; relatively safe: don't last long in environment
b. cats more sensitive than dogs - reptiles & fish very sensitive - sensitivity varies greatly b’twn individual animals c. low oral toxicity: rapidly hydrolyzed in GI tract, metabolized in liver - metabolites are generally non-toxic - formulated w/ synergists to ↑ potency: microsomal enzyme inhibitors (ex. piperonyl butoxide, N-octyl-bicycloheptene dicarboximide (MGK 264)) d. interfere w/ Na channels --> enhanced sodium ion conductance - blocks post-synaptic GABA receptor-chloride ionophores complex --> CNS excitation |
|
|
Pyrethrin & Pyrethroids
a. clinical signs b. dx |
a. CANNOT distinguish from OP/carbamate toxicosis on basis of signs alone
- muscle tremors, mixed CNS effects (depression, excitation, seizures), ↑ salivation, vomiting, ataxia, dyspnea, hypothermia or hyperthermia (d/t muscle tremors: may be severe (105-106º)) b. hx of exposure atropine test dose - give a pre-anesthetic dose of atropine (0.02 mg/kg) - muscarinic signs will likely diminish if signs d/t pyrethrin/pyrethroid toxicosis |
|
|
Pyrethrin & Pyrethroids
a. tx b. px |
a. GI decontamination: AC
- bathe animal w/ mild detergent shampoo if dermal exposure - atropine: 0.04 mg/kg: mixed effectiveness: will reduce some signs - seizure control: valium preferred (promotes GABA) b. many cases will resolve w/ minimal tx w/in 48-72 hrs - aggressive therapy rarely needed: more problems in very young animals |
|
|
Strychnine
a. mechanism of action b. clinical signs c. dx d. tx |
a. competitive glycine receptor inhibitor --> CNS excitation
b. develop w/in 1-4 hrs - stiffness, tonic extensor rigidity, seizures (sound & light induced), opisthotonus, respiratory paralysis c. hx of exposure, clinical signs, chemical analysis of stomach contents, liver, kidney, or urine (renal excretion occurs) d. ↓ GI absorption: AC: emetics are CONTRAINDICATED d/t seizures - control of seizures: valium, barbiturates often ineffective, may need gas anesthetic - muscle relaxants: methocarboamol IV |
|
|
Zinc Phosphide
a. mechanism of action b. clinical signs c. dx d. tx e. px |
a. converted to phosphine gas in acid environment of stomach --> CNS excitation, pulmonary edema
b. develop w/in 1-4 hrs - vomiting (almost always: POTENT emetic), seizures, pulmonary edema, hepatic & renal injury (may be delayed) c. hx of exposure, clinical signs, chemical analysis of stomach contents (can detect phosphine odor) d. ↓ GI absorption - AC not effective - gastric lavage w/ 5% sodium bicarbonate: emetics are CONTRAINDICATED d/t seizures - control of seizures: valium, barbiturates e. if animal survives for 24-36 hrs, will likely recover |
|
|
Bromethalin Rodenticides
a. mechanism of action b. toxicokinetics c. dx |
a. desmethylbromethalin (active form) --> mitochondria --> uncoupling of oxidative phosphorylation --> ↓ ATP --> altered ionic homeostasis --> myelin injury (white matter vacuolation, cerebral edema)
- desmethylbromethalin --> enhanced lipid peroxidation --> myelin injury b. rapid GI absorption - liver metabolism to active form (desmethylbromethalin): hepatic P450s - biliary excretion: enterohepatic recirculation -relay toxicosis is an issue c. hx of exposure, white matter edema (other causes: hexachlorophene, trialkyl tins), detection of bromethalin or metabolites in fat, brain, or liver |
|
|
Bromethalin Rodenticides
a. clinical signs b. lesions c. tx |
a. acute high dose exposure (≥ LD50): onset of signs 1-6 hrs after exposure (uncommon)
- tremors, seizures (noise & light induced), SEVERE hyperthermia, death (rigor mortis w/in 10 min.) low dose exposure (< LD50): onset of signs 12-72 hrs after exposure - many animals die - CNS depression --> semicoma (respond to painful stimuli) --> coma, hind limb ataxia, paralysis, extensor rigidity, decerbrate posture (laying on side: front legs in “prayer” position, roll on back: extension of legs – almost pathognomonic), tremors, anisocoria b. white matter vacuolization thru out nervous system; edema w/in myelin (difficult to tx) c. tx aggressively if > 10% of LD50 ingested - GI decontamination: emetics, repeated AC (d/t enterohepatic recirculation): q 4-6 hrs for 48-72 hrs - AC may just delay signs if high dose exposure - control of cerebral edema: mannitol, dexamethasone, furosemide - gingko biloba: helped experimentally in rats |
|
|
Marijuana
a. toxic principle b. clinical signs c. tx |
a. tetrahydrocannabinol
b. CNS depression, ataxia, vomiting (d/t GI irritation), diarrhea, drooling, tachycardia, seizures, coma c. give an emetic, but may not be very effective: marijuana is a potent anti-emetic - AC + cathartic - symptomatic tx |
|
|
What are some plants that induce paresis or paralysis?
|
Delphinium (larkspur), Sorghum spp. (hybrid sudan), Nicotiana spp., Sweet Pea
typically affects hind limbs 1st: longer nerve tracts |
|
|
What are some toxic agents found in plants that also affect skeletal muscle tone?
|
nicotine (Nicotiania spp.), anabasine (tree tobacco), coniine (poison hemlock), lobeline (cardinal flower: Lobelia spp.)
|
|
|
What are some plants w/ mixed CNS effects?
|
yellow star thistle, locoweeds, avocado
|
|
|
What are some neurotoxic rodenticides?
|
strychnine, bromethalin, zinc phosphide
|
|
|
What are some plants that cause seizures?
|
Delphinium
Lobelia Yellow Jessamine Water Hemlock Marijuana Aflatoxin (d/t hepatic encephalopathy) |
|
|
What are some nicotinic effects?
|
sympathetic overactivity & neuromuscular dysfunction
tachycardia, hypertension, dilated pupils, muscle fasciculation and muscle weakness |
|
|
What are some muscarinic effects?
|
parasympathetic overactivity
SLUD, bradycardia, miosis, sweating, blurred vision, excessive lacrimation, excessive bronchial secretions, wheezing, dyspnoea, coughing, vomiting, abdominal cramping, diarrhea, and urinary and fecal incontinence |

