![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
128 Cards in this Set
- Front
- Back
|
what is an internal abdominal hernia?
|
Organ herniation through a ring of tissue confined within the abdominal cavity, such as a diaphragmatic hernia or organ displacement through a mesenteric rent
|
|
|
define true, false, and aquired hernias
|
True: the ring may be confined within a normal aperture in the abdominal wall
False: may occur in other areas Aquired: as a result of trauma or through a disrupted surgical approach |
|
|
what is peritonealization?
|
Whereas in developmental (congenital) hernias, the hernial sac is a mesothelial membrane (peritoneum) covering the contents, in acute traumatic or incisional hernias, no sac is present. Over time, a peritoneal sac may form over the contents of chronic traumatic or incisional hernias; this process is termed peritonealization.
|
|
|
what is an auto-penetrating hernia?
|
When a traumatic abdominal hernia caused by a fractured rib penetrating through the paracostal musculature results in organ herniation,
|
|
|
what muscles make up the linea alba?
|
the tendinous aponeuroses of the external abdominal oblique, internal abdominal oblique, and transverse abdominal muscles converge and join on midline to form a thick white band, termed the linea alba, which is located between the rectus abdominis muscle
|
|
|
what is the prepubic tendon?
|
The linea alba narrows considerably before it attaches to the pubis by the prepubic tendon (sometimes termed the cranial pubic ligament)
|
|
|
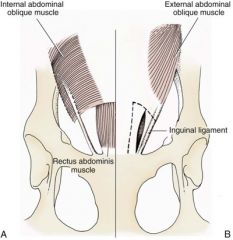
where does external abd oblique originate?
|
fibers of the external abdominal oblique muscles originate from the fourth or fifth to the twelfth rib and from the last rib and thoracodorsal fascia and extend in a caudoventral direction before giving rise to their broad aponeurosis.
|
|
|
where does int abd oblique originate?
|
arise from the thoracolumbar fascia caudal to the last rib and from the tuber coxae
|
|
|
where does transversus abdominus arise?
|
comes from two parts:
the lumbar portion arises from the transverse processes of the lumbar vertebrae and the thoracolumbar fascia and the costal portion arises from the medial sides of the twelfth and thirteenth ribs and from the eighth to eleventh costal cartilages. Fibers from this muscle extend in a dorsoventral direction. |
|
|
name and describe the components of an abdominal hernia
|
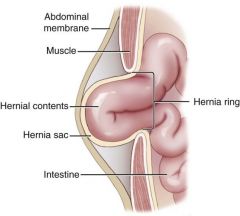
|
|
|
what are the locations of abdominal hernias, and is each usually congenital or traumatic?
|
cranial ventral midline: congenital
-umbilical -substernal (ventral) lateral: trauma -paracostal defects just off caudal rib' -ventral to lumbar transverse processes caudal: -scrotal, inguinal (congenital) -prepubic, femoral (trauma) |
|
|
what is another term for space occupying effects?
|
loss of domain
occurs when the abdominal wall has become accustomed to a relatively small intraabdominal volume because of organ displacement outside the cavity (usually through a large defect). Manual reduction of the hernia contents and primary closure of the defect is difficult or impossible in this situation |
|
|
what are consequences of organ reduction with los of domain?
|
excessive tension on repair
pulmonary complications restriction of diaphragm fxn poor organ perfusion abdominal compartment syndrome Conzemius et al. Clinical determination of preoperative and postoperative intra-abdominal pressures in dogs. Vet Surg. 24, 1995 |
|
|
what are some techniques that can be used to aid in reduction of organs through large defects to avoid loss of domain?
|
Progressive pneumoperitoneum
tissue expansion with inflatable Silastic expanders gradually stretch the abdominal wall in much the same way as pregnancy. Staged reduction of open congenital abdominal defects with a Silastic sac has achieved excellent results with little mortality in infants. Most adult human patients with loss of domain are repaired using prosthetic materials (e.g., mesh) |
|
|
describe the muscles of the abdominal wall and the orientation of the fibers
|

|
|
|
what do Strangulated umbilical, inguinal, femoral, and prepubic hernias most often contain?
|
falciform ligament or omentum, uterus, prostatic fat, and urinary bladder, respectively
|
|
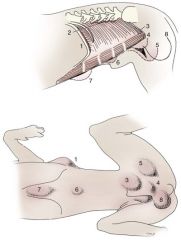
label each number
|
1, Paracostal hernia;
2, dorsal lateral hernia; 3, inguinal hernia; 4, cranial pubic ligament rupture; 5, femoral hernia; 6, umbilical hernia; 7, ventral hernia (subxiphoid); 8, scrotal hernia |
|
|
what is a mojor risk of surgery for patients with strangulated organs
|
compromised patients often decompensate and die under anesthesia during attempts at surgical reduction and repair of strangulated hernias;
this is thought to be caused by rapid release of vasoactive substances into the circulation from necrotic strangulated organs during surgical reduction. En bloc resection of the devitalized herniated tissue, with release of the constricting ring only after the vascular supply is occluded, may help reduce this fatal complication. |
|
|
with an external abdominal hernia, should an abdominal incision be made, or should the hernia be incised over?
|
when strangulation of hernia contents is expected, a midline approach is recommended to isolate the abdominal cavity from the necrotic, often highly contaminated, local hernia environment.
In uncomplicated hernias without evidence of obstruction or strangulation, an approach over the hernia rings is considered |
|
|
what is the umbilical aperture?
|
serves as a passageway for the contents of the cord (umbilical blood vessels, small vitelline duct, and stalk of the allantois),
|
|
|
what structures attach to the umbilicus?
|
the falciform ligament (the remnant of the umbilical vein) and middle umbilical ligament of the bladder (the remnant of the urachus) are attached to the internal aspect of the umbilicus.
|
|
|
what diseases have umbilical hernias been linked to?
|
Umbilical hernias have been associated with fucosidosis, an inherited, autosomal recessive, neurovisceral lysosomal storage disease.
Of 31 English Springer spaniels with fucosidosis, 10 had umbilical hernias, and one had a scrotal hernia. This hernia has also been associated with a congenital, sex-linked, recessive disorder in dogs called ectodermal dysplasia. |
|
|
what pattern of genetic transmission do abdominal hernias usually display?
|
Successive breedings of a Labrador retriever and an American foxhound with these defects created ratios of affected offspring suggestive of an autosomal recessive mechanism.
|
|
|
what is an omphalocele?
|
Omphaloceles are large midline umbilical and skin defects that permit abdominal organs to protrude from the body.
Herniated contents are initially covered by a transparent membrane (amniotic tissue) attached to the edges of the umbilical defect until minor trauma ruptures the membrane, exposing the prolapsed contents to contamination |
|
|
what are the most common abdominal hernias in small animals?
|
umbilical hernias
In an epidemiologic study involving congenital abnormalities found in pet store dogs over a 2-year period, umbilical hernias were found in 0.6% (10 of 1679) of animals. |
|
|
what breeds are predisposed to umbilical hernias?
cats or dogs more predisposed? |
Airedale terriers, basenjis, Pekingese, pointers, and Weimaraners are at greater risk.
The incidence of umbilical hernia is about the same in cats and dogs when the aforementioned dog breeds at risk are excluded. A high incidence of umbilical hernia was noted in one family of Cornish rex cats. There is no sex predilection in the general population; however, females of predisposed dog breeds have a greater incidence of umbilical hernia for unknown reasons. |
|
|
how should small <3mm umb hernias be treated in puppies?
|
Initially, healthy puppies with small (<2 to 3 mm) hernias are treated conservatively because spontaneous closure has been reported as late as 6 months of age.97 Affected animals are neutered because of genetic predisposition to this disease.
|
|
|
what umbilical hernias should be fixed?
|
Hernias with inelastic rings that approximate the size of intestine (one finger size in a small to medium-size dog) may be at greater risk for strangulation
|
|
|
name 3 ways to deal with tension on umbilical hernia repair
|
releasing incisions in external rectus fascia
mesh mayo mattress (vest over pants) is controversial |
|
|
what are the 3 types of caudal abdominal hernias?
|
inguinal
scrotal femoral |
|
|
how are inguinal hernias classified?
|
direct: the abdominal viscera enter the cavity of the vaginal process
indirect: the less common form in humans and small animals, organs pass through the inguinal rings adjacent to the normal evagination of the vaginal process. |
|
|
what is the difference between direct and indirect hernias? which are worse?
|
Direct hernias are usually large, and most do not cause incarceration or strangulation.
In contrast, indirect inguinal hernias in male dogs (scrotal hernias) more often cause organ dysfunction because the vaginal process narrows considerably at the relatively inelastic inguinal ring. |
|
|
inguinal hernia classification in dogs (direct and indirect)
|
Inguinal hernia generally denotes direct and indirect hernias in females and direct hernias in males. Indirect hernias in males are considered separately as scrotal hernias.
|
|
|
are congenital inguinal hernias common in dogs?
predisposed breeds? |
No--but often coexist with umbilical hernias
Basenji, Pekingese, poodle, basset hound, Cairn terrier, Cavalier King Charles spaniel, Chihuahua, cocker spaniel, dachshund, Pomeranian, Maltese, and West Highland white terrier |
|
|
what is Gastroschisis?
|
grossly appears like an omphalocele, but the defect is paramedian. This anomaly has been reported in cats and often results in early neonatal death
|
|
|
sex predisposition for UH?
|
develop more often in male dogs than in females, possibly because of delayed inguinal ring narrowing from late testicular descent.
|
|
|
what signalment is predisposed to aquired inguinal hernias?
|
middle aged intact bitches
toy breeds and sharpeis may be predisposed |
|
|
describe indirect vs. direct inguinal hernia
|
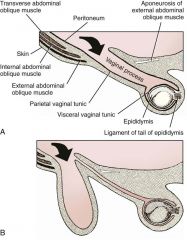
|
|
|
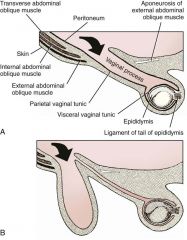
wwhat does the vaginal process contain in males and females?
|
males: spermatic cord
females: round ligament |
|
|
what structures pass through the inguinal canal?
|
the genital branch of the genitofemoral nerve, artery, and vein and the external pudendal vessels pass through the caudomedial aspect of the canal.
|
|
|
what is the inguinal canal?
|
The sagittal slit between the abdominal muscles that connects the external and internal inguinal rings is termed the inguinal canal
|
|
|
what is the internal inguinal ring bordered by?
|
medially by the rectus abdominis muscle
cranially by the caudal edge of the internal abdominal oblique muscle laterally and caudally by the inguinal ligament. |
|
|
what is The external inguinal ring
|
a longitudinal slit in the aponeurosis of the external abdominal oblique muscle
|
|
|
what is an interstitial hernia?
|
forms when a structure passes through the internal ring alone without continuing past outer wall layers. This condition is described in humans but has not been reported in small animals because of differences in anatomy of the inguinal canal
|
|
|
what breeds are predisposed to inguinal hernias?
|
golden retrievers, cocker spaniels, and dachshunds
|
|
|
what factors are involved in inguinal hernia formation?
|
anatomic,
hormonal, metabolic |
|
|
which is the most common cause of inguinal hernia in animals?
|
Enlargement of the entrance to the vaginal process
|
|
|
why are bitches predisposed to inguinal hernias?
|
because the inguinal canal is shorter and of larger diameter than in males.
|
|
|
can congenital inguinal hernias disappear?
|
may disappear spontaneously at 12 weeks of age because of a decrease in the relative size of the inguinal rings.
|
|
|
are inguinal hernias hormonally influenced
|
YES
most appear during estrus or pregnant bitches less frequent in neutered bitches estrogen involved in pathogenesis Sex hormones may change the strength and character of the connective tissue, weakening or enlarging the inguinal rings. Experimentally, a sex hormone imbalance has been directly linked to formation of inguinal hernia in male and female mice. |
|
|
what was found in: A possible association between acquired inguinal and perineal hernia in adult male dogs. Can Vet J. 37, 1996
|
Among male dogs older than 4 years with acquired, nontraumatic inguinal hernias, four of the nine dogs described in the literature and all five dogs at one institution had concurrent unilateral or bilateral perineal hernias
In two other studies, three of 11 and two of 16 males with nontraumatic inguinal hernias had concurrent perineal hemias |
|
|
how is obesity linked to inguinal hernias?
|
Obesity increases intraabdominal pressure, forcing abdominal fat through the inguinal canals.83 Furthermore, accumulation of fat around the round ligament may dilate the vaginal process and inguinal canal, allowing hemiation.
|
|
|
what % of Inguinal hernias are in male dogs?
|
In two case series, males accounted for only 8% to 11% of dogs with inguinal hernias.84,113 Of dogs with nontraumatic inguinal hernias, 37% were male.120 Males with inguinal hernias were younger than females and accounted for five of eight dogs younger than 2 years.120
|
|
|
what side is more common for unilateral IH?
|
more unilateral inguinal hernias occur on the left side than on the right
|
|
|
what is a hysterocele?
|
Large hernias may contain a gravid uterus
|
|
|
what can inguinal hernias be confused with in female dogs? in male dogs?
|
Large inguinal hernias in bitches that extend caudally following the round ligament to the vulva may resemble a pendulous perineal hemia.
Direct inguinal hernias in male dogs may be confused with scrotal hernias because of venous or lymphatic obstruction at the inguinal ring and subsequent swelling and edema of the testicle and spermatic cord. |
|
|
what is The risk of strangulated intestine in dogs with long-standing inguinal hernia?
|
less than 5%.
|
|
|
what are some ddx for inguinal hernia?
|
mammary tumors and cysts, lipomas, enlarged lymph nodes, abscesses, and hematomas
|
|
|
In children with inguinal hernias, what imaging modality has been used to detect occult hernias on the contralateral side?
|
pneumoperitoneography
|
|
|
is FNA indicated for diagnosis of inguinal hernia?
|
may help differentiate an inguinal mass from an incarcerated hernia but is rarely used because accidental puncture of a loop of intestine or pyometra could cause leakage and gross contamination
|
|
|
how are inguinal hernias approached?
|
Uncomplicated unilateral inguinal hernias are approached over the inguinal rings.
In more complicated hernias (incarcerated or strangulated contents, concurrent serious intraabdominal trauma), the approach is first through the ventral midline for exploration; hernia repair is subsequently performed extraabdominally. Some surgeons repair inguinal hernia through the abdominal cavity.9 With this approach, sutures are placed through the parietal peritoneum, the aponeurosis of the transversalis muscle, and the rectus abdominis and internal abdominal oblique Laparoscopic repair of inguinal hernia in affected beagle dogs by direct sac ligation or prosthesis onlay has been described |
|
|
what direction is the inguinal ring extended if necessary?
|
craniomedial
|
|
|
how is the inguinal ring repaired?
|
enlarged external inguinal ring and any incisions in the abdominal wall are closed with prolonged absorbable or nonabsorbable sutures.
In traumatic inguinal hernias or when the external inguinal ring is weak, sutures can be placed between the inguinal ligament, external rectus fascia, and internal oblique abdominal muscle to aid in hernia closure |
|
|
what are some reasons to prefer a midline abd incision for inguinal herniorrhaphy?
|
avoids incising through mammary tissue, an advantage especially in a lactating animal.
It also permits exploration of both inguinal rings, which is recommended by the author because small hernias are frequently missed on palpation |
|
|
what should you do if gravid uterus is within hernia?
|
ovariohysterectomy, which is the simplest option for treatment of a herniated gravid uterus. Successful primary repair of the hernia and replacement of the incarcerated uterus can be performed up to the seventh week of gestation if a valuable litter is expected. After 7 weeks, an ovariohysterectomy or hysterotomy may be recommended
|
|
|
what are some options for repair of inguinal hernias when primary repair is not possible?
|
prosthetic materials.
Inguinal hernias in three intact, small female dogs were successfully repaired by an onlay polyethylene mesh technique. A cranial sartorius muscle flap has been suggested for reconstruction of large inguinal hernias when primary repair is not possible. this was used in conjunction with synthetic implants to repair large chronic caudal abdominal hernias in two young cats |
|
|
what is the prognosis asstd with inguinal hernia repair?
VET SURG (1993) |
In a large series of inguinal hernia repairs in dogs, the overall prevalence of postoperative complications was 17%, and the mortality rate was 3%.
Incisional infection, peritonitis and sepsis, and hernia recurrence were responsible for most postoperative complications. One dog died of intestinal dehiscence after resection of an entrapped, nonviable intestinal segment within the hernia. In one study, all but one of 61 dogs with inguinal hernias survived |
|
|
what are scrotal hernias?
|
Scrotal hernias are indirect hernias that result from a defect in the vaginal ring, allowing abdominal contents to protrude into the vaginal process alongside spermatic cord contents
Herniated organs within the vaginal process do not necessarily have to extend as far distally as the scrotum for the condition to be considered a scrotal hernia |
|
|
who gets scrotal hernias?
|
young male dogs, larger
|
|
|
risk of strangulation in dogs with scrotal hernias?
|
is greater than in females with inguinal hernias.
In a study of 35 dogs with inguinal hernias, five had strangulated bowel, and four were young male dogs |
|
|
are scrotal hernias heritable?
|
heritability is unclear
Ectopic testes have been reported in 19% to 33% of male dogs with inguinal hemias. An increased risk for inguinal hernias was found in dogs with cryptorchidism. |
|
|
the cremaster muscle
|
The cremaster muscle in males is a continuation of the free caudal border of the internal oblique abdominal muscle.
|
|
|
scrotal hernia usually unilateral?
|
yes, though bilat has been reported.
|
|
|
whats a hydrocele?
|
collection of serous fluid within the vaginal process
|
|
|
describe the surgical approach to a REDUCIBLE (or one in which contents are expected to be viable) scrotal hernia?
|
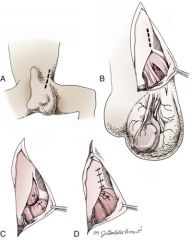
incision of the skin over or lateral to the inguinal rings parallel to the flank fold.
The hernial sac is exposed and opened if necessary, and the abdominal contents are replace |
|
|
how is herniorraphy performed If the testicle is to be preserved
|
If the testicle is to be preserved the enlarged neck of the hernial sac (parietal vaginal tunic) is reduced in size by a transfixing ligature or several horizontal mattress sutures.
These sutures are placed as close to the internal inguinal ring as possible. The external inguinal ring is closed with interrupted sutures, leaving the caudal aspect open just wide enough to allow unconstricted passage of the spermatic cord, external pudendal vessels, and nerve branches. |
|
|
Is castration recommended along with scrotal herniorrhaphy? why or why not?
|
Bilateral castration is currently recommended with repair of scrotal hernia for several reasons.
1.Recurrence of scrotal hernia may be more common if castration is not performed. 2.an increased incidence of testicular tumors in dogs has been associated with scrotal hemias. 3. Because scrotal hernias may be inherited, castration is recommended until convincing evidence to the contrary is found. |
|
|
how do you do castration along with herniorraphy?
|
|
|
|
how are scrotal hernias approached when they contain strangulated tissue?
|
Strangulated viscera within scrotal hernias are approached by a ventral midline incision. Irreversibly damaged visceral tissues are resected/repaired
severely contaminated vaginal processes are resected en bloc repair of hernia is performed extra-abdominally consider scrotal ablation to reduce the risk of sac perforation during dissection |
|
|
what are femoral hernias?
|
protrusion of fat or abdominal contents through a defect in the femoral canal
|
|
|
what is the femoral canal?
|
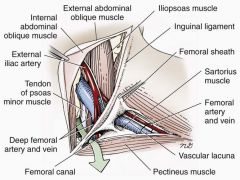
is in the caudal abdominal wall just lateral to the inguinal ligament.
composed of two separate areas contained within the limits of the inguinal ligament and pelvis The muscular lacuna contains the femoral nerve within the substance of the iliopsoas muscle. The vascular lacuna lies craniomedial to the muscular lacuna and contains the femoral artery and vein and the saphenous nerve. The iliopectineal arch, composed of iliac and transverse fascia, separates each lacuna. The transverse fascia also surrounds the femoral vessels, forming the funnel-shaped femoral sheath. Herniation may occur anywhere in this region but likely occurs in a potential space caudomedial to the femoral vessels known as the femoral canal |
|
|
how can femoral hernias be created iatrogenically?
|
by transection of the origin of the pectineus muscle directly off the pubis during subtotal pectineal myectomy or by misdirected dissection during an approach to the ventral coxofemoral joint
|
|
|
how do femoral hernias most often occur?
|
blunt trauma, causing avulsion of the cranial pubic and inguinal ligaments.
Severe inguinal ligament avulsion and separation create a large lateral defect from the sartorius to the pectineus muscle and a swelling along the proximal medial thigh region |
|
|
how can you differentiate inguinal from femoral hernias on palpation?
|
Whereas inguinal hernias are palpated medially and cranially to the pelvic brim, femoral hernias are caudal to the inguinal ligament and ventrolateral to the pelvic brim
|
|
|
how is an uncomplicated femoral hernia repaired?
|
The approach is made parallel to the inguinal ligament. The hernial sac is exposed, and its contents are reduced into the abdomen. The hernial sac is ligated as high in the femoral canal as possible. In hernias with intact inguinal ligaments, the femoral canal is usually closed by placing sutures between the inguinal ligament and pectineal fascia
|
|
|
incidence of traumatic abdominal wall hernias?
|
low.
In a study of 600 small animals injured by motor vehicles, only two abdominal hernias were recognized. Similarly, only two of 132 cats with injuries resulting from falls from high-rise buildings developed abdominal hernias |
|
|
most abdominal hernias are caused by what?
where are most located? |
blunt trauma, such as automobile accidents, kicks, or falls.
Of 21 consecutively studied traumatic abdominal hernias, 17 were caused by blunt trauma (automobile accidents) and four by penetrating trauma (dog fights). the most common areas of herniation caused by blunt trauma are the ventrolateral caudal abdominal (inguinal or prepubic areas) and paracostal regions. |
|
|
Common hernias resulting from avulsion forces include?
|
prepubic (ruptured cranial pubic ligament),
inguinal, dorsolateral (muscle avulsion from transverse processes of lumbar vertebrae) hernias Rupture of the cranial pubic ligament is often associated with concurrent inguinal ligament damage, |
|
|
how do Paracostal hernias develop?
|
when the origin of the external oblique abdominal and transverse abdominal muscles separate from their rib or costal cartilage origin, resulting in herniation of abdominal viscera laterally into the subcutaneous tissues
|
|
|
describe the CT. whats your diagnosis?
|

separation of ventral abdominal wall and mottled soft tissue between abdominal wall edges. A chronic cranial-ventral abdominal hernia filled with falciform fat was found during exploration
|
|
|
better to repair traumatic hernias acutely or wait?
|
controversial
most prefer to wait for several days if patient stabilize. can support large hernias with bandaging wait to allow acutely traumatized tissue time to revascularize, thereby reducing risk of infection. The surgery site will have less inflammation and hemorrhage, permitting better exposure of structures and stronger tissue for suture placement. Delay past this time is not recommended because further wound contraction and adhesion formation may complicate repair |
|
|
how are Cranial pubic ligament avulsions repaired?
|
(“prepubic hernias”) are usually repaired by passing sutures through the avulsed ligament and preplaced holes in the pubis.
Shredded avulsed cranial pubic ligaments or other muscle fascia may be augmented with a mesh cuff or double-layer mesh technique |
|
|
when do acute and chronic incisional hernias occur
|
acute incisional hernias generally occur within the first 7 days after surgery, chronic hernias are noted weeks to years postoperatively
|
|
|
most common cause of chronic incisional hernias?
|
Local wound complications, especially deep infection, are the most important predisposing causes of chronic incisional hernia
|
|
|
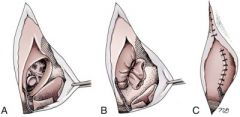
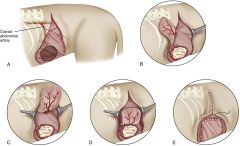
describe cuff mesh repair of prepic tendon rupture
|
Cuff mesh reinforcement of prepubic hernia. A, Ventral view showing damage and shredding of prepubic ligament. B, Interrupted vertical mattress suture fixation of mesh to the abdominal wall with interrupted sutures placed between reinforced prepubic tendon and pubic bone. C, Completed prepubic repair. D, Double-layer mesh technique to help prevent suture pull-out caused by weak hernia tissue edges.
|
|
|
how many throws are required for most suture types to be secure. what are the exceptions?
|
An in vitro knot-testing study found that suture materials placed in an interrupted pattern, with the exception of polydioxanone and monofilament nylon, were secure with three square throws.
Square knots used to begin or end a continuous pattern require an additional one or two square throws, respectively, to be secure. Granny knots, loose asymmetric square knots, and loosely tied square knots were not as secure as tight square knots for most suture materials tested |
|
|
why did many human acute incisonal hernia repairs fail?
|
Of 52 human patients with acute incisional hernia, 88% of the disruptions contained intact sutures that had pulled through tissue; only 12% had broken sutures. The problem with most of the closures was inclusion of too little rather than of too much tissue.
|
|
|
what are some signs of impending incisional hernia?
|
an impending incisional hernia is strongly suspected in an animal that has a serosanguineous discharge from its incision and incisional swelling within the first 5 days of surgery.
horse study where incisional hernias were almost 18 times more likely to develop in wounds with incisional drainage than in those without drainage |
|
|
should wound edges be debrided in repair of acute incisional hernias?
|
Debridement is contraindicated during repair of acute incisional hernias unless wound edges are nonviable or necrotizing infected fascial tissue is present.
Removal of healthy wound edges creates excessive unnecessary tissue trauma and spreads contamination into normally sterile areas. Debridement of this actively healing tissue sets the wound back to the substrate phase, delaying the onset of rapid strength gain. |
|
|
what are the causes, and what is the prognosis asstd with evisceration
|
Abdominal evisceration was secondary to trauma in four animals and to postsurgical dehiscence in eight in a retrospective case series.
All animals had intestinal evisceration and gross contamination of the peritoneum. Despite these daunting issues, all animals survived to discharge from the hospital |
|
|
what are some benefits of mesh herniorrhaphy?
|
Nonautologous methods are usually more simple, because there is less mobilization and exposure necessary to obtain muscle for transfer, resulting in less donor site morbidity.
Besides material strength, mesh herniorrhaphy also increases abdominal wall elastic properties, which is postulated as a major factor in reducing hernia recurrence after repair. |
|
|
describe rectus advancement techniques
|

external oblique release
lateral sheath release Releasing and shifting muscles and fascia generally is not a good choice when large (>7 to 10 cm) hernias are present. |
|
|
what muscle flaps have been described to repair large abdominal wall defects in dogs?
|
cranial sartorius
external abdominal oblique occassionally latissimus dorsi flap |
|
|
what areas can the sarorius flap cover?
|
The approximate areas covered by this muscle flap include:
the caudal 30% of the abdomen if the flap is positioned transversely along the pubis or about 80% of the length between the pubis and ribs on the ipsilateral side if the flap is positioned parallel to midline |
|
|
potential applications of cranial sartorius flap
|
prepubic tendon rupture
inguinal hernia femoral hernias |
|
|
Cranial sartorius muscle flap reconstruction of an inguinal defect. A, The cranial sartorius muscle is elevated from its distal insertion. B, Mobilization of the muscle to the level of the vascular pedicle. C, Transposition of the cranial sartorius muscle to the caudal abdominal wall region so that its external surface is in contact with the external abdominal oblique muscle.
|
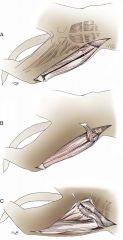
|
|
|
should mesh be placed directly over abdominal organs?
|
the intraabdominal structures should be protected from prosthetic materials with the interposition of omentum
seal the defect, bring blood supply and healing cells to the area, and avoid the risk of visceral adhesions |
|
|
The most widely used materials for abdominal wall replacement and reinforcement during hernia repair in human and veterinary medicine is:?
|
polypropylene mesh (Marlex
More recently, composite meshes (a combination of absorbable and nonabsorbable materials) have become available for human hernia repair. This combination gives acute strength during the first few weeks after implantation. Although the absorbable residue of the mesh is replaced by collagen fiber, a low-weight, nonabsorbable material remains, ensuring permanent strength in combination with low patient morbidity. |
|
|
what is the external abdominal oblique myofascial flap?
what is the blood supply? what defects can it cover? |
The external abdominal oblique muscle, is a myofascial island flap based on the lumbar component,
The cranial branch of the cranial abdominal artery supplies the middle zone of the lateral abdominal wall and is accompanied by the cranial hypogastric nerve and satellite vein. This island flap can be used successfully for treatment of ventral, cranial to mid-abdominal wall defects (e.g., subxiphoid, paracostal) along its arc of rotation. In a pilot study, the flap was more than adequate for coverage beyond 10 × 10-cm full-thickness abdominal wall defects in middle-size dogs. |
|
|
What are some other materials for hernia repair?
what are some advantages? |
absorbable material, such as polyglactin 910 mesh, or a permanent microporous material, such as Gore-Tex (Teflon) mesh,
these facilitates removal with minimal bowel adherence. Gore-Tex mesh is separated easily from tissues. After the patient has been stabilized, the Gore-Tex mesh can be removed from the granulated soft tissues and replaced with porous mesh such as polypropylene. In humans, use of an absorbable mesh alone may result in a hernia defect; therefore, it must be replaced with a permanent mesh. |
|
|
External abdominal oblique myofascial island flap. A, Location of lumbar component of the muscle. B, Three edges of the flap are severed and reflected to show location of neurovascular pedicle. C, Completely severed flap tethered by pedicle. D, Inner surface of flap is sutured to dorsal edge of defect. E, Flap is sutured over defect to complete reconstruction.
|
|
|
what are some biologic tissue grafts used for herniorrhaphy?
|
small intestinal submucosa
dermis pericardium |
|
|
what are the results with biologic tissue grafts in dogs?
|
In a pilot study comparing porcine small intestine submucosa and polypropylene mesh in partial- and full-thickness 10-cm abdominal wall defects in dogs, no evidence of implant breakdown was found with either implant.18 The SIS implants were completely replaced by well-organized, dense, collagenous connective tissue at 4 months. The polypropylene implants had more firm omental attachments.
In dogs, biologic grafts have been used successfully clinically to repair perineal hernias and experimentally for abdominal wall replacement. |
|
|
what are the 3 techniques by which mesh can be applied?
|
onlay,
inlay, underlay |
|
|
what is onlay and what are the associated complications
|
Wound complications such as hematoma, seroma, extrusion, and infection are more common (≤69%) in onlay repairs in humans,
the method now is rarely used to bridge defects. With onlay repairs, mesh is implanted more superficially and with more undermining of adjacent skin and subcutaneous tissues than with the other methods |
|
|
what is the issue with the inlay technique?
|
there is minimal contact area between the mesh and adjacent hernia ring tissue.
Because the weakest point of a mesh repair is the interface between the native fascia and the synthetic material, this technique results in an unacceptably high reherniation rate because of insufficient anchorage |
|
|
what is the preferred method for bridging fascial defects.?why?
|
The underlay technique has the lowest rate of reherniation and wound complications
It provides a large contact area between the mesh and abdominal wall, particularly with abdominal pressure, which creates optimal anchorage of the mesh to adjacent fascia. |
|
|
what addition to an underlay repair has helped with decreasing failure rates in humans?
|
Sliding myofascial flaps or adjacent adipodermal turnover flaps (soft tissue buttresses) placed over underlay mesh provide another layer for mechanical buttress effect.
The soft tissue also serves as a barrier against mesh exposure and contamination from any breach in superficial wound integrity |
|
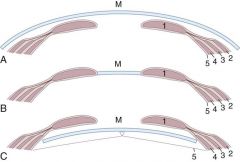
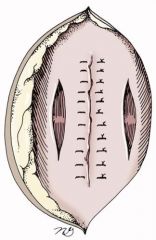
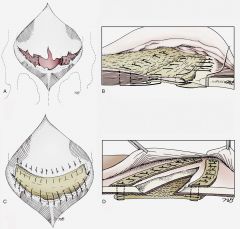
what does each image describe?
|
Reconstruction of a large incisional hernia using the onlay (A) inlay (B) and underlay (C) techniques. 1, Rectus abdominus. 2, External abdominal oblique. 3, Internal abdominal oblique. 4, Transversus abdominus. 5, Peritoneum. M, Mesh.
|
|
|
what is one of the major comps of the inlay technique?
|
Adhesions and enterocutaneous fistulas are complications associated with underlay mesh technique in humans. Omental adhesions were reported in experimental dogs with full-thickness abdominal wall defects replaced with porcine SIS; these adhesions were mild and easily detached.
|
|
|
how is an underlay mesh placed? describe the surgical technique.
|
Soft tissue around the entire abdominal wall defect is undermined directly off the fascia for 2 cm or more until healthy wall is visible.
Adhesions around the hernial ring and within 2 cm of the defect in the peritoneal cavity are lysed to prepare a bed for the mesh. Using the muscle defect as a template, mesh is cut 2 cm larger than the defect in all directions. Healthy omentum is mobilized, folded on itself to make multiple layers, and spread out over the abdominal viscera directly under the defect. The mesh is laid on the omentum, and it is sutured so the edges of the mesh are folded inward to make a double thickness. Monofilament nonabsorbable sutures are preplaced in horizontal mattress fashion around the defect in the following manner: (1) A full-thickness needle bite is taken through healthy abdominal wall at least 1 cm away from the ring; (2) a bite is taken through the middle of a 1-cm fold in the mesh parallel to the margin, with the rough cut edge of the mesh facing outwards toward the surgeon (not the viscera); (3) a 1-cm bite of omentum is taken just underneath the mesh; (4) the needle is passed back through the mesh 1.0 to 1.5 cm away from the first mesh bite and parallel to the defect edge; and (5) a final bite is taken through the full-thickness abdominal wall parallel to the defect, exiting at about 1.0 to 1.5 cm away from the entrance site If sutured properly, the mesh should be covered with omentum on the deep |
|
|
describe the steps involved with placing an underlay technique.
|
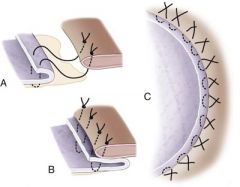
Preplaced horizontal mattress suture catching omentum deep to the folded edge of the mesh. B, Rough edge of overlapped mesh faces away from abdominal viscera. C, Series of preplaced mattress sutures around the defect.
|
|
|
can you use a drain with mesh implants?
|
If excessive subcutaneous dead space remains despite attempts at closure, a closed suction drain may be placed for several days. The drain should be removed as soon as possible to reduce bacterial seeding of the mesh from ascending contamination at the tube exit site.
|
|
|
what is the success rate reported in the vet literature?
Complications associated with the implantation of polypropylene mesh in dogs and cats: a retrospective study of 21 cases (1984–1996). J Am Anim Hosp Assoc. 34, 1998 |
In five reported abdominal hernias (one chronic incisional hernia; four defects from tumor resection) repaired with polypropylene mesh, there were no hernia recurrences, and the only local complication was seroma in two animals.
|
|
|
what was found in:
Radical lateral body-wall resection for fibrosarcoma with reconstruction using polypropylene mesh and a caudal superficial axial pattern flap: a prospective clinical study of the technique and results in 6 cats. Vet Surg. 31, 2002 |
Six cats undergoing radical body wall resection with reconstruction using polypropylene mesh and an axial pattern skin flap did not have evidence of local tumor recurrence or implant failure in another case series; two had minor skin flap dehiscence that healed without incident.
|
|
|
list the surgical complications asstd with abd herniorraphy
|
Anesthesia complications
Hemorrhage Visceral injury Strangulated hernia Gross contamination at the surgical site Inability to close the abdominal wall without tension “Loss of domain” Poor tissue strength at hernia margins |
|
|
list the early post op comps asstd with abd herniorrhaphy
|
Seroma
Hematoma Dermatitis Infection Wound dehiscence and evisceration Pain |
|
|
list the late post op comps asstd with abd herniorrhaphy
|
Skin sinus
Hernia recurrence |

