![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
26 Cards in this Set
- Front
- Back
|
Define the pre embryonic, embryonic and fetal perioids of human development:
|
A pregnancy usually lasts 38 weeks. In order to measure pregnancy you use the last known menstral cycle as it is more accurate than conception date. ( so term is 40 weeks)
38 WEEK TERM: Pre embryonic period - is the first 2 weeks after fertilisation and its function is to establish a pregnancy. The period comprises of many stages: cleavage, compaction, hatching and implantation. Pre-implantation stages are the most hazardous with up to 30% of zygotes failing to develop to the Blastocyst stage. Embryonic period 3 – 8 weeks is the period of greatest change. During this period all major structures and systems are formed and it is the most perilous period for the developing child as prone to interference from outside. Gastrulation and neurulation occur in weeks 3 and 4. Fetal period 9-38 weeks is the maturation of tissues and organs and rapid growth of the body. |
|
|
Discuss the changes taking place as the fertilised human ovum travels down the fallopian tube to the uterus
|
An oocyte is released from the ovary and enters the fallopian tube. Fertilisation by the sperm usually occurs in the ampulla of the fallopian tube after 12-24hrs, and becomes a zygote. The zona pellucida surrounding the zygote prevents further fertilisation by sperm. Sperm are viable for up to 3 days whereas oocytes are only viable for a day. The cilia lining the simple columnar epithelial walls, waft the fluid containing the oocyte towards the uterus, which takes about 4 days. 30 hrs after fertilisation has occurred, the zygote undergoes undergoes multiple divisions, a process called cleavage. 3 days after fertilisation, Cleavage produces the morulla , a ball of identical totipotent cells . By day 4 compaction starts where the cells within the morulla begin to merge to form one large central space converting the morulla into a hollow sphere of cells, the Blastocyst. The Blastocyst is formed by day 5 and cells within differentiate to form 2 cell groups with different fates and functions. The embryoblast becomes the embryo itself and the trophoblast forms the fetal membranes, especially the placenta, which surrounds and sustains the developing embryo and fetus until birth. The trophoblast forms the syncytiotrophoblast which sticks to and invades the endometrium during implantation, day 6. By 8-9 days the embryoblast differentiates into 2 layers, the epiblast and the hypoblast which form the bilaminar disc. It now has dorsal (epiblast) and ventral (hypoblast) surface but not anterior or posterior arientation.
|
|
|
Describe the meaning of the following terms: zygote, cleavage, zona pellucida ,morula, ovary, fallopian tube, uterus.
|
Zygote: the fertilised ovum. Fertilisation should take place at ampulla of fallopian tube to avoid problems.
Cleavage : the zygote undergoes multiple divisions 30 hrs after fertilisation. The first division produces two blastomers. Cleavage forms a ball of identical, totipotent cells called the morula. Zona pellucida: the glycoprotein shell that surrounds zygote during cleavage and compaction but is broken down by the Blastocyst hatching through prior to implantation. Its role is to prevent further fertilisation by sperm. Morula: ball of identical, totipotent cells formed by cleavage of the zygote. Ovary: one of a pair of female gonads where oogenesis occurs to produce the oocyte, one released every month from one organ. Also the ovary is an endocrine organ secreting oestrogen and progesterone when the signal is received for female body characteristic development and control of the menstral cycle and pregnancy. Fallopian tube: carries the egg from the ovary to the uterus by cilia wafting the fluid containing the egg. The ampula of the fallopian tube is the site of fertilisation. |
|
|
Discuss the formation of the Blastocyst and the initial stages of implantation.
|
During compaction, the cells in the morulla merge to form one central space converting the morula into a hollow sphere of cells called the Blastocyst, the first cavity. Cavities are very important as they provide the space for the embryo to grow into. The Blastocyst undergoes first differentiation to produce 2 cell groups with different fates and functions. The trophoblast is the outer mass of cells surrounding the cavity and will form the fetal membranes, especially the placenta, which will support and sustain the embryo and fetus until birth. The embryoblast is the inner cell mass at the top of the cavity and forms the embryo. The Blastocyst breaks through the zona pellucida so that it is free to enlarge and is in contact with the endometrium. The trophoblast differentiates into the syncytiotrophoblast which becomes an outer cell layer and the cytoptrophoblast is the cell layer around the Blastocyst cavity. The synchytiotrophoblast sticks to and invades the endometrium, establishing maternal blood flow within the placenta so support of embryo changes from histiotrophic to haemotrophic. This process is called implantation and usually takes place on the posterior uterine wall.
|
|
|
Describe the meaning of the following terms: Blastocyst, trophoblast, inner cell mass, implantation, cytotrophoblast, syncytiotrophoblast.
|
Blastocyst: a hollow sphere of cells made from the merging of the cells of the morula, with localised thickening – the inner cell mass. The Blastocyst cells differentiate to form the outer cell mass, trophoblast and the inner cell mass, embryoblast.
Trophoblast: formed from the first differentiation in the pre-embyonic period from Blastocyst cells along with the inner cell mass. It is the outer cell mass that surrounds the Blastocyst cavity and will make up the fetal membranes, especially the placenta, which will support and sustain the development of the fetus and embryo. The trophoblast differentiates into the syncytiotrophoblast and the cytotrophoblast. Inner cell mass: the embryoblast formed from the first differentiation in the pre-embryonic period from blastocyst cells. It later differentiates further into the epiblast and the hypoblast. Implantation: the syncytiotrophoblast sticks to and invades the endometrium, establishing the maternal blood flow within the placenta. Support of embryo changes from histiotrophic to haemotrophic. Cytotrophoblast: layer of cells around Blastocyst cavity, differentiation of trophoblast. Syncytiotrophoblast: layer of cells outside the Blastocyst which sticks to and invades the endometrium, establishing uteroplacental circulation where maternal sinusoids, invaded by syncytiotrophoblasts, become continuous with lacunae. |
|
|
Describe the formation of the embryonic disc in the inner cell mass and initial cell differentiation within it
|
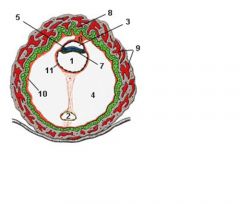
During week 2, The embryoblast, inner cell mass, differentiates to form the bilaminar disc comprising of the epiblast and hypoblast layers. A small cavity appears within the epiblast and develops to form the amniotic cavity. Cells originating from the hypoblast form the exocoelomic membrane which lines the inner surface of the cytotrophoblast. The hypoblast and the exocoelomic membrane together form the lining of the primitive yolk sac. The extraembryonic mesoderm is loose connective tissue, derived from the yolk sac cells and develops between the exocoelomic membrane and the cytotrophoblast layer. Eventually, the extraembryonic mesoderm fills the space between the trophoblast and the embryo except where it is connected to the trophoblast by the mesoderm connecting stalk. The connecting stalk eventually becomes the umbilical cord. Spaces within the extraembyonic mesoderm merge to form the chorionic cavity. A new cavity forms within the yolk sac called the secondary yolk sac which is much smaller than the primitive yolk sac. During its formation large portions of yolk sac are pinched of and form the exocoelomic cysts found in chorionic cavity.
|
|
|
Describe some implantation defects and explain the consequences.
|
Implantation defects occur during pre-embryonic period when implantation occurs at site other than posterior uterine wall.
Ectopic pregnancy: implantation is not in uterus, most commonly fallopian tube but also peritoneum or ovary. This is a life threatening emergency. Placenta praevia: implantation occurs in the lower uterine segment and can cause haemorrhage during pregnancy. C section is required. |
|
|
Describe some assisted reproductive techniques
|
IVF- in vitro fertilisation of oocytes takes place and a morulla of 4-8 cells is achieved. The morulla is then transferred into the uterus.
PGD-pre genetic diagnosis – a cell can be safely removed from the morula and tested for serious heritable conditions prior to transfer of the embryo into the mother. All the cells are identical to the zygote. |
|
|
Define the terms: bilaminar disc, germ layer, ectoderm, endoderm, dorsal and ventral surfaces
|
Bilaminar disc: 2 germ layered disc comprising of epiblast and hypoblast layers. The bilaminar disc is developed in the pre-embryonic period where it is bilaterally symmetrical. The disc is converted to the tri laminar disc via gastrulation in the embryonic period where.
Germ layer: the 3 primary tissue layers, ectoderm, mesoderm, endoderm formed by gastrulation which gives rise to all tissues of the body. Ectoderm: the top layer of cells in the tri-laminar germ disc. It is formed by epiblast cells displacing hypoblast during gastrulation. The major derivatives of ectoderm are organs and structures that maintain contact with outside world eg surface ectoderm: skin and skin derivatice eg hair, nails, lens and cornea of eye, linings of the mouth and anus. Neural ectoderm eg brain, spinal cord, peripheral nerves, retina and iris of eye Endoderm: the bottom layer of cells in the tri laminar germ disc formed by gastrulation. The major derivatives of ectoderm are internal structures eg epithelial lining of GI tract, respiratory tract, parenchyma of glands associated with digestion eg liver and pancreas and other gut derivatives such as lungs. Dorsal: are surfaces towards the back of the foetus Ventral: are surfaces towards the front of the foetus |
|
|
Define the terms: mesoderm, primitive streak, gastrulation, trilaminar embryonic disc.
|
Mesoderm: middle germ layer which has 2 gaps one which will form future mouth and one future anus. Its major derivatives are supporting tissues such as muscle, cartilage, connective tissue, bone, cartilage, vascular system.
Primitive streak: forms at the caudal epiblast at the beginning of gastrulation and is a narrow grove with slightly bulging regions on either side. The primitive node is at the cranial end is slightly elevated to surround the primitive pit Trilaminar embryonic disc: 3 germ layers of slight differentiation: ectoderm, mesoderm, endoderm which are rudimentary lineages from which all tissues will arise in the developing embryo and foetus. Gastrulation: the process establishing the three germ layers and so the origin of all tissues of the body. The three germ layers form the trilaminar disc. Gastrulation also sets the axes observed in the adult, dorsal –back, ventral – front and anterior/posterior, right/lift. |
|
|
List the most important ectodermal, mesodermal and endodermal derivatives.
|
Ectoderm: CNS, epidermis
Mesoderm: CVS, dermis, urogenital system, bone, cartilage, muscle, notochord, mesenchyme Endoderm: GI tract, respiratory tract, endocrine glands |
|
|
Describe the migration of mesoderm through the primitive streak.
|
At the beginning of gastrulation the primitive streak develops from the caudal end of the epiblast layer. The primitive node at the cranial end is the signal centre and releases chemicals. These molecular signals ensure correct dorsoventral and left-right development. The action of cililated cells at the node result in leftward flow of signalling molecules, which initiates side specific signalling cascades. The epiblast cells migrate towards the primitive streak, where they become flask shaped, separate from the epiblast surface and slip beneath by invagination. The position of invagination of epiblast cells along the streak, decides their fate. If the epiblast cells displace the hypoblast they become the endoderm layer, if they sit on top of the endoderm they become the mesoderm and if they remain on the epiblast surface they form the ectoderm. As more and more cells invaginate through the streak they spread laterally and towards the head (cephalad). The primitive streak regresses to the caudal position .
|
|
|
Describe gastrulation
|
Gastrulation begins with the formation of the primitive streak in the caudal epiblast. The primitive streak is a narrow groove with slightly bulging regions on either side. The primitive node is at the cephalic(cranial) end of the streak and is a slightly elevated area surrounding the primitive pit. Cells of the epiblast migrate to the primitive streak and invaginate at the streak. Cells which displace the hypoblast form the endoderm. Cells which lie between the endoderm and epiblast form the mesoderm and the cells remaining in the epiblast form the ectoderm. The ultimate fate of the epiplast cells depend on where along the primitive streak or node they invaginated. Molecular signals from the primitive node ensure correct dorsoventral and left-right development. The Action of ciliated cells at the node results in leftward flow of signalling molecules, which initiates side-specific signalling cascades. As more and more cell migrate through the streak they spread laterally and towards to head (cephalad). The primitive streak regresses to the caudal position. Development proceeds in a cranial to caudal direction. Gastrulation ensures the correct placement of precursor tissues to allow subsequent morphogenesis ( development of form and structure) to take place
|
|
|
Describe a notochord - its formation and function
|
Notochord:
Prenotochordal cells of epiblast invaginate in the primitive node and move forward cranially in the midline until they reach the precordal plate. The notochordal plate is formed from cells derived from the mesoderm, which proliferate and detach from the endoderm, to form a solid rod of cells. The notochord defines the midline, drives neurulation and the axial skeleton forms around it. |
|
|
Describe situs inversus.
|
Situs inversus is the complete mirror image viscera which commonly results from immotile cilia on the primitive node. There is only associated morbidity if there is both normal and mirror image disposition.
|
|
|
Describe how monozygotic twins are developed.
|
Monozygotic twins are developed from a single fertilised oocyte. Either the zygote splits after first cleavage and 2 embryos develop each with their own placenta. Or the inner cell mass is duplicated and 2 embryos share the same placenta.
|
|
|
How can conjoined twinning arise?
|
Splitting may occur very late with duplication of the primitive streak. Therefore the 2 embryos share the same placenta and amniotic sac. Sometimes separation is not complete and conjoined twins are formed.
|
|
|
Describe teratogenesis and agents which cause this.
|
Teratogenesis is the process by which normal embryonic development is disrupted by teratogens causing a birth defect. Terotogens are chemicals such as thalidomide (short limbs), rubella (alters brain development), alcohol (kills cells in development of face), certain therapeutic drug. Weeks 3-8, the embryonic period, are the most sensitive to teratogenic insult. Each organ system has a particularly sensitive window depending on when most of its development occurs. CNS is the first to begin development and the last to visit.
|
|
|
Describe the differentiation of mesoderm into the notochord, somites, intermediate mesoderm and lateral plate.
|
The notochord is a solid rod of cells in the midline formed from epiblast cells migrating through the primitive node and cranially towards the prechordal plate. At the prechordal mesoderm plate the cells intercalate with the endoderm forming the notochordal plate. Eventually the cells of the notochordal plate proliferate and separate from the endoderm forming the notochord. The notochord induces the overlying ectodermal cells to thicken and form the neural plate comprised of neuroectodermal cells. The neural plate becomes elevated to form neural folds at the cranial end and the depressed mid region of the plate forms the neural groove.
Somites are formed from the segmentation of the paraxial mesoderm on either side of the neural tube. The first pair of somites arises around day 20 on the occipital region and 3 arise every day from then on in the craniocaudal direction. At the end of the 5th week 42-44 pairs are present of which some disappear, leaving 31 somite pairs. Somite differentiate into sclerotome, myotome and dermatome. Intermediate mesoderm temporarily connects paraxial mesoderm to lateral mesoderm and then differentiates into urogenital structures eg kidneys, ureters, gonads. Lateral plate mesoderm splits into parietal (somatic) and visceral ( splanchnic) layers which line the intraembryonic cavity and surround the organs respectively. |
|
|
Describe the formation of the coelom
|
The ectoderm forms over the neural tube with the paraxial mesoderm on either side. Within the lateral plate mesoderm, holes begin to develop which merge to form the intraembryonic cavity which will develop into the pericardium, peritoneum and pleural cavity. The cavity divides the lateral plate mesoderm into 2 layers: the parietal mesoderm layer, which lines the intraembryonic cavity and the visceral mesoderm layer which surrounds the organs. The parietal mesoderm along with ectoderm form the lateral body folds. These lateral folds together with the cephalic and caudal folds close the ventral body wall. The parietal mesoderm layer then forms the dermis of the skin in the body wall and limbs, the bones and connective tissue of the limbs and the sternum. Along with migrating sclerotom and myotome cells the layer forms the costal cartilages, limb muscles and most of the body wall muscles. The visceral mesoderm layer with the endoderm forms the wall of the gut tube. Visceral mesodermal cells will form a thin serious membrane around each organ and the mesodermal cells of the parietal layer will form serous membranes that will line the peritoneal, pleural and pericardial cavites and secrete fluid.
|
|
|
|
|
|
List the derivative of each region of the mesoderm:
|
Mesoderm forms the notochord, the paraxial mesoderm, the lateral mesoderm, the intermediate mesoderm.
The paraxial medoderm: scleotomes – vertebrae and ribs, dermomyotomes – dermis for skin of the back and muscles for the back, body wall (intercostals muscles) and some limb muscles. Intermediate mesoderm: forms urogenital structures eg kidney, ureter, gonads Lateral plate mesoderm - differentiates into intraembryonic cavity, parietal mesoderm layer and visceral mesoderm layer. Intraembryonic cavity – pericardium, peritoneal and pleural cavities Parietal (somatic)mesoderm layer – forms the dermis of the skin in the body wall and limbs, will form the serous membrane that lines the body cavities and secretes fluid. Also combines with ectoderm to form lateral body folds and along with cephalic and caudal folds, closes the ventral body wall. Visceral (splanchnic)mesoderm layer - smooth musclculatur, connective tissue and vasculature of gut. It Combines with endoderm to form the wall of the gut tube. It will form the thin serous membrane that surrounds each organ. |
|
|
Describe the formation and fate of the neural plate.
|
The notochord in the midline induces overlying ectodermal cells to thicken and form the slipper shaped neural plate comprised of neuroectodermal cells. The neural plate becomes elevated at the cephalic end to form neural folds and the depressed middle region forms the neural groove.
|
|
|
Describe the formation of the head fold, tail fold and lateral body folds.
|
The embryonic disk is converted into a 3D cylindrical shape with ectoderm outside, endoderm inside and mesoderm sandwiched inbetween. The embryonic disc begins to bulge into the amniotic cavity and to fold cephalocaudally. Folding in the medial plane produces the head and tail folds. As a result of cephalocaudal folding, more and more endoderm is incorporated into the body of the embryo to form the gut tube. The tube is divided into the foregut, midgut and hindgut. The midgut maintains contact with the yolk sac via the umbilicus. The lateral folds are formed from the ectoderm along with the parietal mesodermal layer and move ventrally to assist in body wall closure, closing the embryo off from the yolk sac.
Folding draws together the margins of the disk, forming the ventral body wall. It also pulls amniotic membrane around the embryo, so that the embryo is suspended in the in the amnionic sac (which is within the chorionic cavity). the chorionic cavity eventually is obliterated as the amniotic sac enlarges. The connecting stalk is also pulled ventrally. |
|
|
Describe the differentiation of somites into dermatome, myotome and sclerotome and the fate of each of these in later development
|
Somites are formed from the segmentation of paraxial mesoderm on either side of the neural tube. A somite is a ball of mesodermal cells that undergo epithelisation and arrange themselves in a doughnut shape around a lumen. By the beginning of the forth week, cells in the ventral and medial walls of the somite lose their epithelial characteristics become mesenchymal and surround the neural tube and notochord. Collectively these cells are the sclerotome that will differentiate into the vertebrae and ribs. Cells at dorsal regions of the somite form dermomyotome. The dermatome forms an area of the dermis of the back and the myotome gives rise to a block of skeletal muscle. The myotomes become the muscles of the thoracic and abdominal walls. Each myotome and dermatome has its own segmental nerve component.
|
|
|
Explain the use of the terms dermatome and myotone in describing the innervations of skin and muscles in the adult
|
Developmentally, for a given body segment a dermatome is the part of a somite that gives rise to dermis and the myotome is the part which gives rise to muscle.
However, clinically speaking, dermatome is in reference to an area of skin, supplied by a single spinal nerve. A myotome, clinically speaking, is in reference to a muscle or a group of muscles which are supplied by a single spinal nerve. The spinal cord is described as having segments, each of which gives rise to a nerve root. |

