![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
164 Cards in this Set
- Front
- Back
|
increase tissue extensibility, increase ROM,, induce relaxation, mobilize or manipulate soft tissue and its , modulate pain, reduce soft tissue swelling, or restriction |
what is manual PT? |
|
|
manual lymphatic drainage, manual traction, massage, mobilization/manipulation, and PROM |
what are the different manual proc. and modalities used in PT? |
|
|
synonymous terms |
what are manipulation and mobilization? |
|
|
"a skilled passive movement of a jt"- manual therapy technique of skilled passive movements to Joints and related soft tissue applied at varying speeds, amplitudes, including small amplitude/high velocity therapeutic mvmt. |
what is manipulation and mobilization? |
|
|
everything that relates to the joint .Neuromuscular skeletal system - skeletal, arthrodial, myofascial |
what is a somatic dysfunction? |
|
|
rolls , glides, spins motions |
what are component motions? |
|
|
involuntary control of a joint |
what is joint play? |
|
|
active and passive ROM and muscle function to end range |
what are classical (physiological ) movements? |
|
|
component and joint play necessary to complete classical movements |
what are accessory movements? |
|
|
non thrust, distraction, glides, thrust, muscle energy |
what are the different manipulation movements? |
|
|
to elongate non connective tissue , including adhesions, neurophysiologically to fire cutaneous muscular and joint receptor mechanisms |
what are (non thrust) techniques used for? |
|
|
when a sudden high velocity, short amplitude motion is delivered at the pathological limit of an accessory motion |
what are (thrust) techniques used for? |
|
|
one gets one done faster than the other |
What is the difference between thrust and non thrust techniques? |
|
|
muscle contraction technique to move , using reverse origin and insertion. The use of an isolated isometric contraction to alter positional relationships or to mobilize a joint. synonymous with contract relax |
what are muscle energy techniques? |
|
|
pt performs the mob |
what is self mobilization? |
|
|
mobilization with movement developed by brian mulligan. combination of active physiological mvmts by the pt and passive accessory movements by the therapist |
what is MWM? |
|
|
manipulation under anesthesia. medical procedure where the pt is manipulated while under anesthesia |
what is a MUA? |
|
|
to restore normal, pain free mvmt of the musculoskeletal system is postural balance -restoration of joint play and ROM |
what are the goals of manipulation? |
|
|
biomechanical, neuro, chemical, psychological |
what are the different effects of manipulation? |
|
|
improving the plasticity and elasticity of shortened or thickened soft tissue by : increase ROM, stretching tight capsules, snapping adhesions, alter positional relationships , improve fluid dynamics Ex: blood/synovial fluid, release synovial structures |
what are the effects of biomechanical manipulation? |
|
|
reduce muscle tone and pain by firing mechanoreceptors -type 1,2,3,4 |
what are the neurophysiological efx of manipulation? |
|
|
releases endorphins and lipoproteins |
what are the chemical effects of manipulation? |
|
|
touch-pts love touch, ability to find and reproduce a pts pain, thorough evaluation, people here a 'pop' and think something has happened |
what are the physiological effects of manipulation? |
|
|
malignancy , bone disease, unstable fx, excessive pain, hyper mobility in associated its, total jt replacements, newly formed connective tissue. Ex: RA - tissue is weakened |
What are precautions to manipulation? |
|
|
6-unstable 5-considerable hypermobility (stabilize) 4-slight hypermobilty (stabilize) 3-normal 2-slight hypomobility (mobilize) 1-considerable hypomobility (mobilize) 0- ankylosed |
what are the different grades of mobility? |
|
|
when jt surfaces have maximum contact with each other , are tightly compressed and difficult to seperate |
what is a congruent jt surface? |
|
|
when jt surfaces do not have maximum contact with each other and are easily seperated |
what is an incongruent jt surface? |
|
|
may cause increased pain and jt trauma. lever magnifies forces at the jt, excessive compression in the direction of the rolling bone , a roll without a glide does not replicate normal jt mechanics |
what is passive angular stretching? |
|
|
are safer and more selective , forces are applied close to the jt surface and are controlled at an intensity compatible with the pathology |
what are joint -glide stretching? |
|
|
grades 1 and 2 jt mobs because they do not stretch the capsule |
what does CAPTE say is "not inappropriate " to teach to SPTAS? |
|
|
cannot perform jt mobs |
what APTA says PTA s cannot do? |
|
|
loss of ROM |
Manual therapy techniques address what general type of dysfunction? |
|
|
brian mulligan |
Who developed the MWM mode of PT? |
|
|
type 2 |
what type of mechanoreceptors are stimulated by oscillation? |
|
|
type 3- they are stimulated by stretch, sustained pressure, thrust |
what type of mechanoreceptors in capsule and ligament are used to inhibit tone for relaxation? |
|
|
hypermobility, jt effusion, inflammation |
what are the contraindications for manipulation? |
|
|
open packed position |
what position do we mobilize joints in? |
|
|
Jeffrey maitland |
who created joint mobilization grades? |
|
|
small amp rhythmic oscillation at beginning of ROM |
what is grade 1 joint mob? |
|
|
large amp oscillations, performed in ROM, prior to tissue resistance |
what is grade 2 joint mob? |
|
|
take to end range with large amp oscillations |
what is grade 3 joint mob? |
|
|
small amp oscillations performed into the resistance of the joint capsule |
what is grade 4 joint mob? |
|
|
freddy kaltenborn |
who created the jt distraction grades? |
|
|
1-bunching up the skin 2-bunch skin and take to onset of resistance 3-stretching of the capsule for minimum of 6 sec, and gradually repeat |
what are the joint distraction grades? |
|
|
is idiopathic,meaning unknown |
what is the etiology of adhesive capsulitis? |
|
|
<3months chilling pain: with movement motion: limited ext. rot. |
what is stage 1 of a frozen shoulder? |
|
|
3-9 months freezing pain: with sitting motion: tightening down, ROM lost, P/AROM jt play |
what is stage 2 of a frozen shoulder? |
|
|
9-15 months frozen pain: going down motion: limited |
what is stage 3 of a frozen shoulder?
|
|
|
15-24 months thawing pain: decreased -no pain motion: restore some motion |
what is stage 4 of a frozen shoulder? |
|
|
within 18-24 months |
when does frozen shoulder usually resolve? |
|
|
1. AROM limited within capsule 2. PROM limited within capsule 3.Loss of jt play within capsule 4. capsular end feel limited |
what 4 conditions must be met for someone to have adhesive capsulitis? |
|
|
maximum protection, moderate protection and controlled motion, minimum protection or return to function |
what are the basic tx concept phases of rehab? |
|
|
PROM with grade 1 and 2 mobs to decrease pain and promote jt nutrition |
what is usually done within the max protection phase? |
|
|
AAROM and AROM with grade 3 and 4 mobs if jt play is not restored |
what is usually done within Moderate protection or controlled motion phase? |
|
|
continue jt mobs, progress activities to restore (necessary) function |
what is usually done within Minimum protection or return to function phase? |
|
|
synovial: glenohumeral, acromioclavicular, and sternoclavicular |
what are the its of the shoulder girdle complex? |
|
|
sup angle : T2 spine: T3 Inf angle: T7 |
what are the spinal levels of the scapula? |
|
|
2;1 ratio |
what is the scapulohumeral rhythm ratio? |
|
|
cervical spine: C4 and C5 nerve roots. C5 dermatome is lateral humeral region |
what are the common sources of referred pain in the shoulder region? |
|
|
diaphragm, gallbladder, heart (L or R shoulder,axilla and pec region), liver to R shoulder |
what are the related tissues/organs that can refer pain to the shoulder? |
|
|
brachial plexus in thoracic outlet, suprascapular nerve in notch , radial nerve in axilla |
what are some nerve disorders found in the shoulder girdle complex? |
|
|
rheumatoid atrhritis and osteoarhtritis, traumatic arthritis, post immobilization, idiopathic frozen shoulder |
what are some glenohumeral joint pathologies and symptoms for hypo mobility? |
|
|
ext rot, abduction, int. rot. |
what capsular pattern creates the greatest limited motion? |
|
|
decreased ROM, guarding, pain, decrease function, stiffness |
what are some glenohumeral hypo mobility clinical signs and symptoms? |
|
|
haircare, using atm, and drive thru |
what are some functional impairments of glenohumeral hypo mobility ? |
|
|
maintain soft tissue and jt integrity and mobility: PROM of involved its , grade 1 and 2 jt mobs(decrease pain and guarding, increase jt nutrition), mm setting ex, codmanns ex, scap mobs.- maintain integrity and function of associated regions |
what actions should be taken for glenohumeral hypo mobility during the management -protection phase? |
|
|
control pain, edema, and jt effusion. progressively increase jt and soft tissue mobility-can add AROM in pain free ROM, add grade III and IV mobs (not aggressively) stretching if any tightness.inhibit muscle spasm and correct faulty mechanics-no substitutions. improve jt tracking -mobs and ex.. improve mm performance. postural re-ed: cervical retraction |
what actions may be taken to glenohumeral jt hypo mobility during the management -controlled phase? |
|
|
progressively increase flexibility and strength - restore mm balance, postural re-ed , mm re-ed, jt mobs more aggressively if still needed. prepare for functional demands-progress to more functional complex tasks.HEP training |
what actions may be taken to glenohumeral jt hypo mobility during the return to function phase ? |
|
|
actually is considered surgery but is closed procedure (no cutting). performed when no progress is met. becomes acute lesion with inflammatory reaction. (critical) to maintain the motion met from the procedure |
what actions are taken during glenohumeral post manipulation under anesthesia ? |
|
|
overuse syndromes, sublaxations or dislocations, and or hypo mobility |
what are some related pathologies and etiologies of the AC and SC joints? |
|
|
pain at end range, elevation, cross body reaching |
what type of activities should be limited with AC and SC jt hypo mobility ? |
|
|
supraspinatus, infraspinatus, or bursa trapped between greater tubercle and acromian |
what is subacromial impingement? |
|
|
Type 2 and 3-curved and hooked. may cause tight posterior capsule and also bring the acromian tip closer |
what type of acromians are more likely to cause impingement ? |
|
|
removal of anterior , inferior surface of acromian |
what is acromioplasty? |
|
|
test: bicipital tendonitis lift: palpate bicipital groove, with shoulder flex, supination |

what is the Speeds Test? |
|
|
test: subscapularis weakness/ teres major lift: hands away from back |

what is the lift -off test? |
|
|
test: infraspinatus weakness lift: hold pts hand in ext. rot., watch for drop |
what is the ER lag test? |
|
|
test: supraspinatus/rotator cuff tear or impingement lift:hold them in 90* ABD, wait for drop |
what is the drop arm test? |
|
|
test : reproduce impingement pain lift: int rot. with ABD |

what is the empty can test? |
|
|
test: partial supraspinatus tear lift: thumbs up, lift to ABD |

what is the full can test? |
|
|
test: subacromial impingment lift: passive IR, pain around 90-120* elbow flexed |

what is the Neer test? |
|
|
test: subacromial impingment lift: passively flex shoulder, then IR |

what is the Hawkins-Kennedy test? |
|
|
test: integrity of the transverse humeral ligament lift: slight ABD, elbow 90*, forearm pronated, resist as they flex toward mouth |

what is the Yergasons test? |
|
|
test: labral tears lift: supine 160* ABD shoulder, look for clicking or reproduction of symptoms |

what is the crank test? |
|
|
test: reproduction of label tears at long head of biceps tendon lift: supine, shoulder 120* ABD, with elbow flexion 90*, forearm supinated. Reproduce pain |

what is the Biceps Load test for Slap Lesion? |
|
|
test: anterior glenohumeral instability lift: standing or supine, passive 90* ABD with elbow flexed .Slowly ER shoulder reproducing symptoms with guarding and pt feeling unstable |

what is the apprehension test? |
|
|
test: pain goes away with post. glide from acromian impingement lift: glide the glenohumeral jt posteriorly to release pain from apprehension test |

what is the relocation test? |
|
|
test: humerus displacement lift: move pts humerus in multi directions |

what is the load and shift test? |
|
|
standard alignment of GH jt with prosthetic components. Needs intact or repairable RTC |
what is a TSA? |
|
|
ball and socket components reversed . can be done with insufficient RTC |
what is a rTSA? |
|
|
higher in pts with deficient RTC and or osteoporosis.RTC tear, loosening, dislocation |
what are the complications of GJA? |
|
|
ER so capsule and subscapularisis can heal |
what motion must be limited initially after TSA? |
|
|
0-140* or 150* elevation and ER of 0-45 or 50* |
what are the ROM expectations of rTSA or TSA? |
|
|
50% |
how much tissue is healed in 2 weeks? |
|
|
80% |
how much tissue is healed in 6 weeks? |
|
|
100% |
how much tissue is healed in 12 weeks? |
|
|
age, disease, poor diet, lack of exercise |
what are some factors that can impede the healing process? |
|
|
doc creates an incision that goes into muscle also |
what is an "open" or traditional incision? |
|
|
scope used and small ports are used to access jt/ or tissue |
what is atrhoscopic surgery? |
|
|
both a small incision and cameras are used. allows less scar tissue build up |
what is a mini-open or minimally invasive surgery ? |
|
|
type I- normal type 2- curved type 3- hooked |
what are the 3 types of acromians? |
|
|
anteriorly |
what is the most common direction for glenohumeral dislocation? |
|
|
superior labrum anterior and posterior tear or impingement where the biceps tendon meets the labrum |

what is a SLAP lesion? |
|
|
ant. dislocation, post .aspect of head gets slammed against ant. glenoid and causes a fx on head of humerus |

what is a Hills Sachs lesion? |
|
|
x-ray |
how is a Hills sachs lesion identified? |
|
|
ant. inf. labrum peels away from glenoid and caused by ant. dislocation |

what is a Bankart lesion and what would most likely cause it? |
|
|
supraspinatus tendonitis |
what primary condition causes a painful arc? |
|
|
when tendons become irritated within the subacromial space as they pass through Ex: swimmers shoulder pain 60-120* flexion, no pain past 120* |
what is a painful arc? |
|
|
cause: superficial location makes it extremely susceptible to injury ( acute or chronic) direct blow signs: pain, swelling,and point tenderness. swelling will appear almost spontaneously and w/out usual pain and heat |
what is olecranon bursitis? |
|
|
cause: vulnerable area due to lack of padding. result of blow or direct blows
signs: swelling(rapidly after irritation of bursa or synovial membrane)
care: treat with RICE immediately for 24 hours. if severe , get x-ray |
what is a contusion? |
|
|
cause: elbow hyper extension or a valgus force
signs: pain along medial aspect of elbow. inability to grasp objects. point tenderness over MCL
care: RICE w/elbow fixed at 90* in a sling for at least 24 hours. should be concerned with gradually regaining elbow full ROM. Hyperextension will cause MCL tear |
what is a elbow sprain? |
|
|
aka: tennis elbow cause: repetitive microtrauma to insertion of extensor muscles of lateral epicondyle
signs: aching pain, pain worsens and weakness of wrist and hand develop, elbow has decreased ROM and pain w/ resistive wrist ext.
care: RICE, NSAIDS, and analgesics.ROM exercises and PRE, deep friction massage, hand grasping while in supinantion, avoidance of pronation |
what is lateral epicondylitis? |
|
|
cause: repeated forceful flexion of the wrist and extreme valgus torque of elbow
signs: pain produced w/ forceful flexion or ext. point tenderness and mild swelling. passive movement of wrist seldom elicits pain, but active movement does
care: sling, rest, cryotherapy or heat through ultrasound . analgesic and NSAID .Curvilinear brace below elbow to reduce elbow stressing. Severe cases ,may require splinting and complete rest for 7-10 days |
what is medial epicondylitis? |
|
|
cause: pronounced cubital valgus may cause deep friction problem. ulnar nerve dislocation. traction injury from valgus force, irregularities w/ tunnel, sub laxation of ulnar nerve due to lax impingement , or compression of ligament on the nerve
signs: generally respond with parathesia in 4th and 5th digits
care: avoid an aggravating condition. surgery is necessary if stress on nerve can not be avoided |
what are ulnar nerve injuries? |
|
|
cause: high incidence in sports caused by fall on outstretched hand w/elbow extended or severe twist while flexed.
signs: swelling, severe pain, disability. may be displaced backwards, forwards or laterally. complication w/ median and radial nerves and blood vessels. rupture and tearing of stabilizing ligaments will usually accompany the injury
care: immobilize. elbow should remain splinted in flexion for 3 weeks |
what is a dislocation of the elbow? |
|
|
cause: direct blow or FOOSH often fxs humerus above condyles or between condyles
signs: may result in visual deformity , hemorrhaging, swelling, muscle spasm
care: ice and sling for support and immobilization |
what are fractures of the elbow? |
|
|
cause: due to falls and direct blows fxing ulna or radius singularly is rarer than simultaneous fxs to both
signs: audible pop or crack followed by moderate to severe pain , swelling, and disability. Edema ecchymosis w/ possible crepitus |
what are forearm fxs? |
|
|
cause: occurs in lower end of radius or ulna. FOOSH forcing radius and ulna into hyperextension
signs: forward displacement of radius causing visible deformity ( silver fork). when no deformity is present injury may be passed off as a sprain , extensive bleeding and swelling, tendons may be torn/ avulsed and there may be median nerve damage
care: x ray and immobilization , treat with immobilization, treat associated its. |

what is a Colles FX? |
|
|
cause: abnormal forced movement . falling on hyperextended wrist , violent flexion or torsion
signs: pain, swelling, and difficulty with movement
care: RICE, splint and analgesics.treat according to phase |
what are wrist sprains?
|
|
|
cause:overuse of wrist, repetitive accelerations and decelerations.
signs: pain on active use or passive stretching. tenderness and swelling over involved tendon
care: acute pain and inflammation treated w/ ice massage 4x daily for first 48-72hours , NSAIDS and rest. protect injured tendon with wrist splint. PRE can be instituted once swelling and pain subsided (high rep, low resistance) |
what is wrist tendonitis? |
|
|
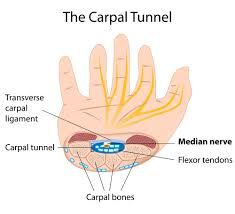
cause: compression of median nerve due to inflammation of tendons and sheaths of carpal tunnel. result of repeated wrist flexion, or direct trauma to ant aspect of wrist
signs: sensory and motor deficits( tingling, numbness, and parathesia) thumb atrophy,APE hand, thumb weakness
care: rest, immobilization, NSAIDS. if symptoms persist , corticosteroid injection may be necessary or surgical decompression of transverse carpal ligament |
what is carpal tunnel syndrome? |
|
|
cause: FOOSH , compressing scaphoid between radius and second row of carpal bones.
signs: swelling, severe pain in anatomical snuffbox
care: splinted and referred for x ray prior to casting . immobilization lasts 6 weeks and is followed by strengthening and stretching . Wrist requires protection against impact loading for 3 additional months. often fails to heal due to poor blood supply - avascular necrosis |
what is a scaphoid fx? |
|
|
cause: direct axial or compressive force . fxs of the 5th metacarpal are associated w/ boxing or martial arts.
signs: pain and swelling : possible angular or rotational deformity. palpable defect is possible .
care: RICE and immobilization, deformity is reduced , followed by splinting- 4 weeks |
what is a metacarpal fx? |
|
|
cause: blow that contacts tip of finger avulsing extensor tendon from insertion
signs: pain at DIP : X-ray shows avulsed bone on dorsal proximal distal phalanx. unable to extend distal end of finger. point tenderness at sight of injury.extensor digitorum communes
care: surgical repair or splinting |
what is mallet finger? |
|
|
cause : rupture of extensor tendon, dorsal to middle phalanx. forces DIP into ext. and PIP into flex.
signs: sever pain, obvious deformity and inability to extend DIP, swelling and point tenderness
care: cold, followed by splinting PIP for 5-8 weeks, pt is encouraged to flex distal phalanx |
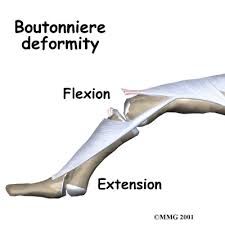
what is a Boutonniere deformity? |
|
|
cause: rupture of flexor digitorum profundus tendon from insertion on distal phalanx, ring finger
signs: DIP can not be flexed , finger remains extended , pain and point tenderness over dotal phalanx
care: must be surgically repaired . rehab requires 12weeks and there is often poor gliding of tendon, w/possibilty of re rupture |

what is the Jersey finger? |
|
|
cause : sprain of UCL of MCP jt of the thumb. Mechanism is forceful ABD of proximal phalanx occasionally combined with hyperextension
signs: pain over UCL in addition to painful weak pinch. tenderness and swelling over medial aspect of thumb.
care: thumb splint should be applied for 3 weeks or until pain free |

what is the gamekeepers / skiers thumb? |
|
|
cause: axial force to tip of the finger . produces "jammed" effect .
signs: severe pt tenderness at jt . lateral or medial jt instability
care: ice for acute stage . X-ray to rule out fx and splint for support |
what is a collateral ligament sprain? |
|
|
cause: blow to tip of the finger (directed upward from palmar side) - forces 1st and 2nd jt dorsally. results in tearing of supporting capsular tissue and hemorrhaging. possible rupture of tendons
care: 3 weeks in 30* flexion in splint with possible buddy tape |
what is a dislocation of the phalanges? |
|
|
cubital fossa, tunnel of Guyon, creates weak grasp, parasthesia of 4th and 5th digit |
where is the ulnar nerve most commonly injured? |
|
|
FDP to 4th and 5th , lumbricals, interossei, policies with ADD |
what muscles are involved in an ulnar nerve injury? |
|
|
tinels and froments |
what tests might be used to test ulnar nerve damage? |
|
|
claw hand |
what deformity might be present with ulnar nerve damage? |
|
|
after effects of immobilization |
with elbow dislocation, elbow fxs, wrist and forearm fxs, and hand fxs, what are we treating? |
|
|
jt mobs, restore gliding. Mobs 1 and 2 for pain and guarding, stretching |
what tx intervention s would a pta use for a elbow fx? |
|
|
ulnar nerve irritabilty, tapping at cubital tunnel and tunnel of Guyon, and ulnar notch |

what is Tinels? |
|
|
carpal tunnel, compress the carpal tunnel with two hands together |
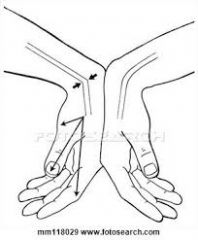
what is phalens? |
|
|
dequervains. compress thumb , bend your hand forward |

what is finkelsteins? |
|
|
tubercle of scaphoid, trapezium, pisiform, hamate, roof -flexor retinaculum |
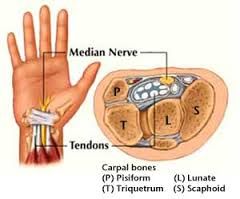
what are the contents of the carpal tunnel? |
|
|
APL tendon , EPB tendon |
what is the lateral boundary of the snuffbox? |
|
|
EPL tendon |
what is the medial border of the snuffbox? |
|
|
scaphoid, trapezium, ECRL and ECRB tendons |
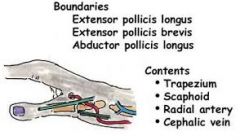
what is the floor of the anatomical snuffbox? |
|
|
radial artery |
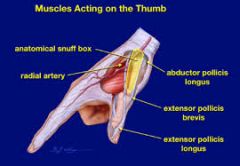
what are the contents of the snuffbox? |
|
|
transition from zone 2-3(palm) |

what zone in the hand is considered no mans land? |
|
|
levator scapula-dorsal scapular upper trap-axillary |
scapula elevators |
|
|
Lats-thoracodorsal lower trap- CN11 / accessory |
scapula depressors |
|
|
serratus ant.-long thoracic |
scapula protraction (ABD) |
|
|
middle trap- CN11/ accessory rhomboids- dorsal scapular |
scapula retractors (ADD) |
|
|
upper trap- CN11/ accessory middle trap- same lower trap- same serratus ant- long thoracic |
scapula upward rot. |
|
|
levator scapula-dorsal scapular rhomboids-dorsal scapular pec minor- med. pec |
scapula downward rot. |
|
|
ant delt- axillary pec major- lat. and med. pec biceps- muscu. corachobrachialis- muscu.
|
shoulder flexors |
|
|
post delt- axillary lats- thoracodorsal teres major- subscapular triceps- radial |
shoulder extensors
|
|
|
supraspinatus- suprascapular middle delt- axillary |
shoulder ABD |
|
|
lats- thoracodorsal teres major- subscapular pec major-med and lat pec |
shoulder ADD
|
|
|
post delt- axillary |
horizontal shoulder ABD |
|
|
ant delt- axillary pec major- med. and lat pec |
horizontal shoulder ADD |
|
|
subscapularis- subscapular teres major- subscapular lats-thoracodorsal pec major- med and lat pec ant delt- axillary |
int. rot. of the shoulder |
|
|
post delt- axillary infraspinatus- suprascapular teres minor- axillary |
ext. rot. of the shoulder |
|
|
biceps- muscu. brachialis- muscu. brachiradialis- radial |
elbow flexors |
|
|
triceps- radial |
elbow ext. |
|
|
biceps- muscu. supinator- radial |
forearm supination |
|
|
pronator teres- median pronator quadratus- median |
forearm pronation |
|
|
FCR- median PL- median FCU- ulnar |
wrist flexion (off medial epicondyle) |
|
|
ECRL- radial ECRB- radial ECU-radial |
wrist ext (off lateral epicondyle and supracondylar ridge) |

