![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
64 Cards in this Set
- Front
- Back
|
A substance that inhibits the enzymatic activity of a proteinase
|
antiproteinase
|
|
|
Chronic dilation of bronchi or bronchioles as a result of inflammatory disease or obstruction associated with heavy sputum; or a chronic condition of one or more bronchi or bronchioles marked by irreversible dilation and destruction of the bronchial walls.
|
bronchiecstasis
|
|
|
Surgical removal of one or more bullae(air spaces in the lung measuring more than 1 cm in diameter in the disteneded state).
|
Bullectomy
|
|
|
A systemic necrotizing vasculitis with prominent lung involvement including severe asthma and eosinophilia.
|
Churg-Strauss syndrome
|
|
|
Right-sided heart failure, usually due to structural lung disease(e.g., pulmonary fibrosis or emphysema)
|
Cor pulmonale
|
|
|
A dark blue or purple discoloration of the skin and mucous membranes due to deficient oxygenation of the blood
|
cyanosis
|
|
|
Impairment of the voice or difficulty speaking
|
dysphonia
|
|
|
Difficulty breathing; often associated with lung or heart disease, and resulting in shortness of breath
|
dyspnea
|
|
|
Abnormally high concentration of carbon dioxide in the blood
|
Hypercapnia
|
|
|
An increase in the number of cells w/in a tissue leading to an increase in tissue or organ size
|
Hyperplasia
|
|
|
Deficient oxygenation of the blood
|
Hypoxemia
|
|
|
Inflammation of the bronchioles characterized by obliteration and/or permanent narrowing of the airways
|
Obliterative bronchilitis
|
|
|
The essential and distinctive cells or tissue of an organ(as distinguished from its supporting framework)
|
Parenchyma
|
|
|
The max flow rate of air leaving the lungs upon forced exhalation
|
Peak expiratory flow
|
|
|
A condition in which there is a net increase in the total circulating erythrocyte mass of the body
|
Polycythemia
|
|
|
any one of numerous enzymes that catalyze the breakdown of proteins; aka protease
|
proteinase
|
|
|
Exaggeration of normal variation in the pulse during respiration-- the pulse becomes weaker during inhalation and stronger during exhalation; characterized by constrictive pericarditis or pericardial effusion
|
Pulsus paradoxus
|
|
|
Abnormal rumbling sounds heard on ausculation of an obstructed airway. They are more prominent during expiration and may clear somewhat on coughing
|
Rhonchi
|
|
|
Measurement of inhaled and exhaled volumes and flow rates of gas from the lungs. Pulmonary function tests obtained from this are used to aid in the diagnosis of Obstructive and restrictive airway diseases
|
Spirometry
|
|
|
Abnormally rapid respiration rate
|
tachypnea
|
|
|
A comparison of the proportion of lung tissue being ventilated by inhaled air to the rate of oxygenation of pulmonary blood
|
Ventilation-perfusion ratio
|
|
|
Which was found to be most effective step-up tx for children from Lemanske study?
LABA, ICS or LTRA step-up? |
LABA. Though some children had good response with others.
|
|
|
RB is a 13 y.o. African American girl who presents with c/o SOB when she exercises. She has joined the cross country team, and she is having trouble keeping up with the other girls ion the team because she gets extremely SOB 5-10 minutes into her run; her chest begins to feel tight, and she coughs. The symptoms usually go away 30 minutes to an hour after she stops running. She also wakes up at night approximately once a week because she is having trouble catching her breath.
What information is suggestive of asthma? How would you classify this patient’s asthma severity? . What additional information do you need to know before creating a treatment plan for this patient? |
RB is a 13 y.o. African American girl who presents with c/o SOB when she exercises. She has joined the cross country team, and she is having trouble keeping up with the other girls ion the team because she gets extremely SOB 5-10 minutes into her run; her chest begins to feel tight, and she coughs. The symptoms usually go away 30 minutes to an hour after she stops running. She also wakes up at night approximately once a week because she is having trouble catching her breath.
What information is suggestive of asthma? SOB when she exercises, SOB 5-10 minutes into her run, chest tightness, coughs Usually goes away 30 minutes to an hour after she stops running Wakes up at night, one night/week b/c trouble catching her breath How would you classify this patient’s asthma severity? Exercise-induced and mild-persistent asthma (because of nighttime symptoms once a week or 4x/month). What additional information do you need to know before creating a treatment plan for this patient? Current meds, inhaler technique, allergen, environment, spirometry PMH, FH, SH, med allergies, allergy symptoms (watery eyes, runny nose/rhinitis, cough) |
|
|
PMH: Allergic rhinitis x 6 years; bronchitis 3 times in the last 6 years, last episode 6 months ago; hospitalized with viral lower respiratory tract (LRT) infection twice at ages 2 and 4
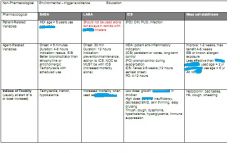
FH: mother had asthma as a child, but “outgrew” it and has had no problems with it since she was 12 or 13 years old; both her mother and father have allergic rhinitis. SH: only child who lives at home with her mother and father in a 2-BR duplex built on a concrete slab; neither the patient nor her parents smoke or dink alcohol; they have no animals inside or outside the home. Meds: Fexofenadine SR 180 mg PO daily ROS: unremarkable except as described above PE: General appearance: small for her age but appears to be well nourished and healthy. VS: BP 112/68 mm Hg, P 78 bpm, RR 18 bpm, T 37 C Ht 4’6” Wt 62 # (28kg) Chest: CTA BL, no wheezing CV: RRR, normal heart sounds, no rubs, gallops, or murmurs EXT: no clubbing, cyanosis, or edema Labs: normal except for an eosinophil count of 7% of the total WBC PFTs FEV1: 90% predicted FVC: 92% predicted FEV1:FVC: 0.914 Post-bronchodilator FEV1: 8.1% increase FEV1 after exercise 23.1% decrease Given the additional information, what is your assessment of the patient’s condition? Why now: Identify your treatment goals for this patient. What nonpharmacologic and pharmacologic alternatives are feasible for this patient? Outline a treatment plan for this patient that includes nonpharmacologic, pharmacologic therapy, and monitoring plan. What is your rationale for your choices? Nonpharmacologic: Pharmacologic: Six months later, RB’s mother brings her back for a check-up. The patient has been using her albuterol inhaler 3-4 times a week to treat symptoms, and she is waking up about twice a month with SOB. She has developed a sore mouth. White patches on the back of her tongue and the inside of her cheek are observed on exam. Meds: Beclomethasone 84 mcg/puff, 1 puff four times a day Albuterol HFA 2 puffs PRN x sx Fluticasone nasal spray 1 puff in each nostril daily What further information do you need before altering this patient’s therapy? How would you counsel this patient to prevent further adverse reactions? Assuming that the patient is currently using her meds appropriately, how would you adjust this patient’s meds? |
PMH: Allergic rhinitis x 6 years; bronchitis 3 times in the last 6 years, last episode 6 months ago; hospitalized with viral lower respiratory tract (LRT) infection twice at ages 2 and 4
FH: mother had asthma as a child, but “outgrew” it and has had no problems with it since she was 12 or 13 years old; both her mother and father have allergic rhinitis. SH: only child who lives at home with her mother and father in a 2-BR duplex built on a concrete slab; neither the patient nor her parents smoke or dink alcohol; they have no animals inside or outside the home. Meds: Fexofenadine SR 180 mg PO daily ROS: unremarkable except as described above PE: General appearance: small for her age but appears to be well nourished and healthy. VS: BP 112/68 mm Hg, P 78 bpm, RR 18 bpm, T 37 C Ht 4’6” Wt 62 # (28kg) Chest: CTA BL, no wheezing CV: RRR, normal heart sounds, no rubs, gallops, or murmurs EXT: no clubbing, cyanosis, or edema Labs: normal except for an eosinophil count of 7% of the total WBC PFTs FEV1: 90% predicted FVC: 92% predicted FEV1:FVC: 0.914 Post-bronchodilator FEV1: 8.1% increase FEV1 after exercise 23.1% decrease Given the additional information, what is your assessment of the patient’s condition? Etiology and severity (same because not currently treated): Spirometry does not clearly suggest asthma however, nighttime symptoms consistent with mild, persistent asthma. More tests needed. Spirometry does show EIB. Why now: allergic rhinitis flare Identify your treatment goals for this patient. Diagnosis asthma Control asthma symptoms (better sleep) Control allergy symptoms Exercise without symptoms What nonpharmacologic and pharmacologic alternatives are feasible for this patient? Provide education on proper inhaler technique, allergen avoidance/environment control Pharmacologic: EIB: SABA, montelukast, cromolyn, nedocromil Allergies: cetirizine, diphenhydramine Asthma : Outline a treatment plan for this patient that includes nonpharmacologic, pharmacologic therapy, and monitoring plan. What is your rationale for your choices? Nonpharmacologic: create asthma action plan and provide education on inhaler teachnique, role of medications, environement control, allergen testing to identify allergens to avoid Pharmacologic should be for EIB and for Step 2 asthma For EIB: use SABA PRN 30 minutes before exercise (benefits should last 2-3 hours) For step 2 asthma, start a low dose ICS (alternatives cromolyn, LTRA, nedocromil, or theophylline) For allergies, could consider allergen immunotherapy and/or switch to alternative antihistamine such as cetirizine, loratidine, diphenhydramine Follow up evaluation with spirometry in 2-4 weeks. Six months later, RB’s mother brings her back for a check-up. The patient has been using her albuterol inhaler 3-4 times a week to treat symptoms, and she is waking up about twice a month with SOB. She has developed a sore mouth. White patches on the back of her tongue and the inside of her cheek are observed on exam. Meds: Beclomethasone 84 mcg/puff, 1 puff four times a day Albuterol HFA 2 puffs PRN x sx Fluticasone nasal spray 1 puff in each nostril daily What further information do you need before altering this patient’s therapy? How is she actually using inhalers. Review technique. Is she swiching and spitting after use of ICS? How would you counsel this patient to prevent further adverse reactions? Rinse and spit after using beclamethasone inhaler Assuming that the patient is currently using her meds appropriately, how would you adjust this patient’s meds? Add a LABA OR LTRA, or theophylline |
|
|
CC: “My asthma has gotten worse lately. I’ve had a lot of wheezing and had to use my albuterol every three hours for the last few days, so it’s almost empty. I need my doctor to prescribe something stronger.”
HPI: PT is a 28 y.o. man with a 15 year h/o chronic asthma. His condition has been poorly controlled for the last six months, causing frequent absences from his job. Most recently, he has suffered from asthma symptoms at least once nightly during sleep requiring albuterol for relief. He has also c/o chest tightness in the mornings for the last three days. A PEFR of 280 L/min form this morning is 70% of his personal best. He does not routinely monitor his PEFR at home. PMH: Asthma since 1980, hospitalized x 3 over the last two years, seasonal allergies (fall pollens), tonsillectomy at age 10 FH: father died at age 59 lung cancer (smoker); mother (age 56) alive with HTN; sister (age 32) has allergic rhinitis SH: accountant, non-smoker, alcohol three times a month Meds: Albuterol inhaler 2 puffs QID Triamcinolone inhaler 3 puffs TID Fexofenadine 60 mg PO BID PRN Allergies: sulfa drugs (rash) ROS: cough, sore throat; otherwise unremarkable PE: Gen: patient is anxious, thin man in moderate distress VS: BP 124/76 mm Hg, p 68 bpm, RR 28 bpm T 37.1C,; Wt 68 kg; Ht 180 cm RESP: diffuse wheezing BL Remainder of PE unremarkable or non-contributory Labs Na 140 K 4.1 Cl 99 Co2 25 BUN16 SCr 1.1 Glu 97 Hgb 15.1 Hct 44% PLT 285 WBC 8 CXR: mild thoracic overinflation, no infiltrate Other: 3 refill requests in past two months for albuterol inhaler, triamcinolone last refilled 3 months ago. What is your assessment of this patient’s asthma? Etiology: Severity: Why now?” How did you arrive at the at assessment? What pieces of information were used to determine your assessment? State the treatment goals for this patient and how those goals will be measured. Acute: Chronic: Impairment: Risk: Describe the treatment plan for this patient. Include drug, dose, route of administration, duration of therapy, monitoring and follow-up. (Consider both short-term and long-term goals.) |
CC: “My asthma has gotten worse lately. I’ve had a lot of wheezing and had to use my albuterol every three hours for the last few days, so it’s almost empty. I need my doctor to prescribe something stronger.”
HPI: PT is a 28 y.o. man with a 15 year h/o chronic asthma. His condition has been poorly controlled for the last six months, causing frequent absences from his job. Most recently, he has suffered from asthma symptoms at least once nightly during sleep requiring albuterol for relief. He has also c/o chest tightness in the mornings for the last three days. A PEFR of 280 L/min form this morning is 70% of his personal best. He does not routinely monitor his PEFR at home. PMH: Asthma since 1980, hospitalized x 3 over the last two years, seasonal allergies (fall pollens), tonsillectomy at age 10 FH: father died at age 59 lung cancer (smoker); mother (age 56) alive with HTN; sister (age 32) has allergic rhinitis SH: accountant, non-smoker, alcohol three times a month Meds: Albuterol inhaler 2 puffs QID Triamcinolone inhaler 3 puffs TID Fexofenadine 60 mg PO BID PRN Allergies: sulfa drugs (rash) ROS: cough, sore throat; otherwise unremarkable PE: Gen: patient is anxious, thin man in moderate distress VS: BP 124/76 mm Hg, p 68 bpm, RR 28 bpm T 37.1C,; Wt 68 kg; Ht 180 cm RESP: diffuse wheezing BL Remainder of PE unremarkable or non-contributory Labs Na 140 K 4.1 Cl 99 Co2 25 BUN16 SCr 1.1 Glu 97 Hgb 15.1 Hct 44% PLT 285 WBC 8 CXR: mild thoracic overinflation, no infiltrate Other: 3 refill requests in past two months for albuterol inhaler, triamcinolone last refilled 3 months ago. What is your assessment of this patient’s asthma? Etiology: acute exacerbation of severe, persistent asthma Severity: moderate exacerbation, very poorly controlled (chronically) Why now?”possibly non-adherent to ICS d/t AEs, tachyphylaxis to beta-agonist How did you arrive at the at assessment? What pieces of information were used to determine your assessment? See p 54, figure 20 in guidelines and p 212 clinical presentation of acute exacerbation State the treatment goals for this patient and how those goals will be measured. Acute: resolve asthma symptoms Chronic: Impairment: Improve control of symptoms (and sleep), reduce need to use albuterol to < 2 days/week, reduce symptom frequency Risk: reduce risk for future exacerbations Describe the treatment plan for this patient. Include drug, dose, route of administration, duration of therapy, monitoring and follow-up. (Consider both short-term and long-term goals.) Acute: PO corticosteroids, monitor PEF, O2 sats, lungs (wheezing) Chronic: Step 1-2 steps (currently his regimen suggests Step 2). Given his severe disease, it is reasonable to jump to step 4 increase dose of ICS and add LABA scheduled. [Alternative regimens: medium dose ICS + LTRA, Medium-dose ICS + theophylline] If allergies are a factor, fexofenadine dose may need to be increased or alternative antihistamine, and/or immunotherapy after allergen testing once symptoms are stable. Follow-up in 2 weeks. Use the PEFR daily. |
|
|
This is from Lemanske study posted on BB:
CARE Study Activity Summarize the main research question in one sentence. Based on the NAEBPP Guidelines, what “Step” are the patients entering the study? Did the researchers define “uncontrolled” in a manner consistent with guidelines? How did the researchers define the primary outcome of “response”? Is this consistent with the guidelines? How would you answer the primary research question based on the results presented in the study? |
Summarize the main research question in one sentence.
Which of the three alternatives for step-up therapy in children with step 2 therapy (low-dose ICS) is best? (+) LABA, (+) LTRA, OR increase dose to medium dose ICS Based on the NAEBPP Guidelines, what “Step” are the patients entering the study? Step 2 Did the researchers define “uncontrolled” in a manner consistent with guidelines? Yes - occurrence of at least on eof the following for > 2 d/week during 2 week period o diary-reported symptoms o rescue use of inhaled bronchodilator with > 2 puffs/day o PEF < 80% predicted How did the researchers define the primary outcome of “response”? Is this consistent with the guidelines? Total amount of prednisone received < 180 mg over the treatment period (48 weeks or 1 year) Increase number asthma control days by 31 days or more over 1 year Increase FEV1 at least 5% over 1 year Yes, these are similar in concept to guidelines How would you answer the primary research question based on the results presented in the study? All three improved asthma, but (+) LABA seemed to give the best response overall in children ages 6-17 years. with step 2 treatment for persistent asthma. |
|
|
Define asthma. What cells are key players?
|
Asthma is a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role: in particular, mast cells, eosinophils, neutrophils (especially in sudden onset, fatal exacerbations, occupational asthma, and patients who smoke), T lymphocytes, macrophages, and epithelial cells. In susceptible individuals, this inflammation causes recurrent episodes of coughing (particularly at night or early in the morning), wheezing, breathlessness, and chest tightness. These episodes are usually associated with widespread but variable airflow obstruction that is often reversible either spontaneously or with treatment.
|
|
|
Under “Causes of Asthma”, what is the central pathophysiologic feature that is the primary target of therapy?
|
Inflammation
|
|
|
Describe the key indicators when a diagnosis of Asthma. Which is required for a diagnosis of asthma?
|
All indicators fine, but SPIROMETRY is needed to establish DIAGNOSIS
KEY SYMPTOM INDICATORS FOR CONSIDERING A DIAGNOSIS OF ASTHMA The presence of multiple key indicators increases the probability of asthma, but spirometry is needed to establish a diagnosis. -Wheezing—high-pitched whistling sounds when breathing out—especially in children. A lack of wheezing and a normal chest examination do not exclude asthma. - History of any of the following: — Cough (worse particularly at night) — Recurrent wheeze — Recurrent difficulty in breathing — Recurrent chest tightness -Symptoms occur or worsen in the presence of: — Exercise —Viral infection — Inhalant allergens (e.g., animals with fur or hair, house-dust mites, mold, pollen) — Irritants (tobacco or wood smoke, airborne chemicals) — Changes in weather — Strong emotional expression (laughing or crying hard) — Stress — Menstrual cycles -Symptoms occur or worsen at night, awakening the patient. |
|
|
List goals of therapy(2)
|
A) Reduce impairment (prevent chronic symptoms, require infrequent use of short-acting beta2-agonist
(SABA), maintain (near) normal lung function and normal activity levels). B) Reduce risk (prevent exacerbations, minimize need for emergency care or hospitalization, prevent loss of lung function, or for children, prevent reduced lung growth, have minimal or no adverse effects of therapy). |
|
|
What are the four components of a ASTHMA management program?
|
1. Assessment and Monitoring – Severity, control, followup
2. Education 3. Control Environmental Factors and Comorbid conditions 4. Medications |
|
|
[Definition] - the intrinsic intensity of the disease process. Assess asthma severity to initiate therapy.
|
Severity
|
|
|
[Definition] - the degree to which the manifestations of asthma are minimized by therapeutic interventions and the goals of therapy are met. Assess and monitor asthma control to adjust therapy.
|
Control
|
|
|
[Definition] the ease with which asthma control is achieved by therapy.
|
Responsiveness
|
|
|
[Definition] frequency and intensity of symptoms and functional limitations the patient is experiencing currently or has recently experienced
|
Impairment
|
|
|
[Definition] the likelihood of either asthma exacerbations, progressive decline in lung function (or, for children, lung growth), or risk of adverse effects from medication.
|
Risk
|
|
|
How are the concepts of severity and control used in managing asthma?(you know for adjusting and initiating tx, etc)
|
1. Assess severity to initiate therapy
2. Assess control to adjust therapy 3. For assessing a pts overall asthma severity, once the most optinal asthma control is acheieved and maintained (correlate the level of severity with the lowest level of treatment required to maintain control. |
|
|
To characterize a patient’s asthma initially, what information is important to use?(4)
|
1. Classify asthma severity
2. Identify precipitating factors for episodic symptoms 3. Identify comorbid conditions that may impeded asthma mgmt(e.g. sinusitis, rhinitis, GERD, OSA, ovesity, stress, or depression) 4. Assess the pts knowledge and skills |
|
|
What are key education messages that should be reinforced at every opportunity? (shaded box)
KEY EDUCATIONAL MESSAGES: TEACH AND REINFORCE AT EVERY OPPORTUNITY |
Basic Facts About Asthma
- The contrast between airways of a person who has and a person who does not have asthma; the role of inflammation. -What happens to the airways during an asthma attack. Role of Medications: Understanding the Difference Between: -Long-term control medications: prevent symptoms, often by reducing inflammation. Must be taken daily. Do not expect them to give quick relief. - Quick-relief medications: SABAs relax airway muscles to provide prompt relief of symptoms. Do not expect them to provide long-term asthma control. Using SABA >2 days a week indicates the need for starting or increasing long-term control medications. Patient Skills - Taking medications correctly — Inhaler technique (demonstrate to the patient and have the patient return the demonstration). — Use of devices, as prescribed (e.g., valved holding chamber (VHC) or spacer , nebulizer). - Identifying and avoiding environmental exposures that worsen the patient’s asthma; e.g., allergens, irritants,tobacco smoke. - Self-monitoring —Assess level of asthma control. — Monitor symptoms and, if prescribed, PEF measures. —Recognize early signs and symptoms of worsening asthma. -Using a written asthma action plan to know when and how to: —Take daily actions to control asthma. —Adjust medication in response to signs of worsening asthma. -Seeking medical care as appropriate. |
|
|
What are common environmental factors that affect asthma? How can they be managed or controlled? (See figure 9)
|
Tobacco Smoke
-If you smoke, ask your doctor for ways to help you quit. Ask family members to quit smoking, too. -Do not allow smoking in your home, car or around you. -Be sure no one smokes at a child’s daycare center or school. Dust Mites Many people who have asthma are allergic to dust mites. Dust mites are like tiny “bugs” you cannot see that live in cloth or carpet. Things that will help the most: - Encase your mattress in a special dust-mite proof cover.* -Encase your pillow in a special dust-mite proof cover* or wash the pillow each week in hot water. Water must be hotter than 130 °F to kill the mites. Cooler water used with a detergent and bleach can also be effective. -Wash the sheets and blankets on your bed each week in hot water. Other things that can help: -Reduce indoor humidity to or below 60 percent, ideally 30–50 percent. Dehumidifiers or central airconditioners can do this. - Try not to sleep or lie on cloth-covered cushions or furniture. -Remove carpets from your bedroom and those laid on concrete, if you can. -Keep stuffed toys out of the bed, or wash the toys weekly in hot water or in cooler water with detergent and bleach. Placing toys weekly in a dryer or freezer may help. Prolonged exposure to dry heat or freezing can kill mites but does not remove allergen. Animal Dander Some people are allergic to the flakes of skin or dried saliva from animals. The best thing to do: - Keep pets with fur or hair out of your home. If you can’t keep the pet outdoors, then: -Keep the pet out of your bedroom, and keep the bedroom door closed. -Remove carpets and furniture covered with cloth from your home. If that is not possible, keep the pet out of the rooms where these are. Cockroach Many people with asthma are allergic to the dried droppings and remains of cockroaches. Vacuum Cleaning -Try to get someone else to vacuum for you once or twice a week, if you can. Stay out of rooms while they are being vacuumed and for a short while afterward. Indoor Mold - Dehumidify basements if possible. Pollen and Outdoor Mold During your allergy season (when pollen or mold sporecounts are high): - Try to keep your windows closed. - If possible, stay indoors with windows closed during the midday and afternoon, if you can. Pollen and some mold spore counts are highest at that time. - Ask your doctor whether you need to take or increase anti-inflammatory medicine before your allergy season starts. Smoke, Strong Odors, and Sprays Exercise or Sports - You should be able to be active without symptoms. See your doctor if you have asthma symptoms when you are active—such as when you exercise, do sports,play, or work hard. - Ask your doctor about taking medicine before you exercise to prevent symptoms. - Warm up for a period before you exercise. - Check the air quality index and try not to work or play hard outside when the air pollution or pollen levels (if you are allergic to the pollen) are high. Other Things That Can Make Asthma Worse - Sulfites in foods: Do not drink beer or wine or eat shrimp, dried fruit, or processed potatoes if they cause asthma symptoms. - Cold air: Cover your nose and mouth with a scarf on cold or windy days. - Other medicines: Tell your doctor about all the medicines you may take. Include cold medicines, aspirin,and even eye drops. Key: HEPA, high-efficiency particulate air |
|
|
Is long-term or short term most effective at attenuating underlying inflammation characteristic of asthma?
|
LONG TERM
|
|
|
Long term or short term meds used to treat acute symptoms and exacerbations?
|
QUICK-ACTING/SHORT TERM
|
|
|
Corticosteroids(inhaled):
1. Short term or Long Term 2. General MOA 3. Role of this class of meds |
1. Long term
2. – anti-inflammatory that reduce airway hyperrespnosiveness, inhibit inflammatory cell migration and activation, and block late phase reaction to allergen 3. Inhaled Corticosteroids(ICSs) are better than LTRAs. Reduce impairment and risk of exacerbations, but do not appear to alter progression of underlying disease severity in child. |
|
|
CROMOLYN sodium and NEDOCROMIL:
1. Short term or Long Term 2. General MOA 3. Role of this class of meds |
1. Long term
2. stabilize mast cells and interfere with chloride channel function. 3. They are used as alternative, but not preferred, medication for patients requiring step 2 care (for mild persistent asthma). They also can be used as preventive treatment before exercise or unavoidable exposure to known allergens. |
|
|
Omalizumag(Immunomodulator)
1. Short term or Long Term 2. General MOA 3. Role of this class of meds |
1. Long term
2. (anti-IgE) is a monoclonal antibody that prevents binding of IgE to the high-affinity receptors on basophils and mast cells. 3. Omalizumab is used as adjunctive therapy for patients 12 years of age who have sensitivity to relevant allergens (e.g., dust mite, cockroach, cat, or dog) and who require step 5 or 6 care (for severe persistent asthma). Clinicians who administer omalizumab should be prepared and equipped to identify and treat anaphylaxis that may occur. |
|
|
Leukotriene modifiers(Zileuton etc):
1. Short term or Long Term 2. General MOA 3. Role of this class of meds |
1. Long term
2. interfere with the pathway of leukotriene mediators, which are released from mast cells, eosinophils, and basophils. These medications include LTRAs (montelukast and zafirlukast) and a 5-lipoxygenase inhibitor (zileuton). 3. LTRAs are alternative, but not preferred, therapy for the treatment of patients who require step 2 care (for mild persistent asthma). LTRAs also can be used as adjunctive therapy with ICSs, but for youths 12 years of age and adults, they are not preferred adjunctive therapy compared to the addition of LABAs. LTRAs can attenuate EIB. Zileuton can be used as alternative, but not preferred, adjunctive therapy in adults; liver function monitoring is essential. |
|
|
LABAs (salmeterol and formoterol). No frequent use before exercise(disguises pooly controlled persistent asthma)
1. Short term or Long Term 2. General MOA 3. Role of this class of meds |
1. Long term
2. are inhaled bronchodilators that have a duration of bronchodilation of at least 12 hours after a single dose. 3. — LABAs are not to be used as monotherapy for long-term control of asthma. — LABAs are used in combination with ICSs for long-term control and prevention of symptoms in moderate or severe persistent asthma (Step 3 care or higher in children ≥5 years of age and adults and Step 4 care or higher in children 0–4 years of age, although few data are available for 0–4-year-olds.). — Of the adjunctive therapies available, LABA is the preferred therapy to combine with ICS in youths ≥12 years of age and adults. — A LABA may be used before exercise to prevent EIB(exercise induced bronchospasm), |
|
|
Sustained-release theophylline (Methylxanthine)
1. Short term or Long Term 2. General MOA 3. Role of this class of meds |
1. Long term
2. mild to moderate bronchodilator 3. Used as alternative, not preferred, therapy for step 2 care (for mild persistent asthma) or as adjunctive therapy with ICS in patients ≥5 years of age. Theophylline may have mild anti-inflammatory effects. Monitoring of serum theophylline concentration is essential. |
|
|
Ipratropium
1. Short term or Long Term 2. General MOA 3. Role of this class of meds |
1. Short term
2. inhibit muscarinic-cholinergic receptors and reduce intrinsic vagal tone of the airway. 3. Ipratropium bromide provides additive benefit to SABA in moderate or severe exacerbations in the emergency care setting, not the hospital setting. Ipratropium bromide may be used as an alternative bronchodilator for patients who do not tolerate SABA, although it has not been compared to SABAs. |
|
|
SABAs—albuterol, levalbuterol, and pirbuterol
therapy 1. Short term or Long Term 2. General MOA 3. Role of this class of meds |
1. Short term
2. bronchodilators that relax smooth muscle. 3. They are the treatment of choice for relief of acute symptoms and prevention of EIB. Increasing use of SABA treatment or the use of SABA >2 days a week for symptom relief (not prevention of EIB) generally indicates inadequate asthma control and the need for initiating or intensifying anti-inflammatory. |
|
|
Systemic Corticosteroids
1. Short term or Long Term 2. General MOA 3. Role of this class of meds |
1. Short term
2. Anti-inflammatory. Although not short-acting, oral systemic corticosteroids are used for moderate and severe exacerbations in addition to SABA. 3. to speed recovery and to prevent recurrence of exacerbations. |
|
|
What is better for asthma pts. ICS or LTRAs?
|
ICS
|
|
|
Name two LABAs?
|
Salmeterol and formoterol. Not used as monotherapy
|
|
|
Inhaled Anticholinergic.
|
Ipratropium bromide
|
|
|
Name at least two SABAs...
|
Albuterol, levalbuterol, pirbuterol.
|
|
|
Treatment of choice for relief of acute symptoms and prevention of EIB.
|
SABAs(albuterol, levalbuterol, pirbuterol). If used greater than two days a week generally indicateds need for initiating or intensifying anti-inflammatory.
|
|
|
Define asthma exacerbation.
|
acute or subacute episodes of progressively worsening shortness of breath, cough, wheezing, and chest tightness, or some combination of these symptoms. Exacerbations are characterized by decreases in expiratory airflow; objective measures of lung function (spirometry or PEF) are more reliable indicators of severity than symptoms are. Individuals whose asthma is well controlled with ICSs have decreased risk of exacerbations. However, these patients can still be vulnerable to exacerbations, for example, when they have viral respiratory infections.
|
|
|
What factors are used to assess severity of an acute exacerbation?
|
-Previous severe exacerbation (e.g., intubation or ICU admission for asthma)
- Two or more hospitalizations or >3 ED visits in the past year - Use of >2 canisters of SABA per month - Difficulty perceiving airway obstruction or the severity of worsening asthma -Low socioeconomic status or inner-city residence - Illicit drug use - Major psychosocial problems or psychiatric disease - Comorbidities, such as cardiovascular disease or other chronic lung disease |
|

|

|
|

|

|
|

|

|
|

|

|
|
|

|
|

|

|

