![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
what is Glaucoma
|
Slowly progressive, insidious onset optic nerve damage leading to reduced vision
Due to increased intraocular pressure (IOP) ?Mechanism of pressure damage to nerve ?Low tension glaucoma Divided by cause of increased IOP Open Angle Closed Angle |
|
|
Epidemiology and risks
|
Common, increases with age
2% over 40s, 5-9% over 65s Risks -family history -High IOP - african or asian descent -diabetes - near sighted - long term steroid use - hypertension - previous high injury |
|
|
Normal Eye Function Aqueous humor
|
is made in the eye (ciliaryprocesses) and then is eliminated through Schlemm‘scanal
A thick watery substance between the lens and the cornea Functions: Maintain IOP, inflates globe of eye (provides dioptericpower to cornea) Provides nutrition to avascularocular tissues Carries away waste Presence of immunoglobulins-role in immune response Problems with overproduction or lack of elimination can lead to increased pressure |
|
|
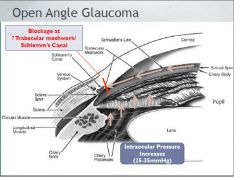
What is open angled glaucoma
|
|
|
|
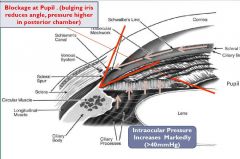
what is closed eye glaucoma
|
|
|
|
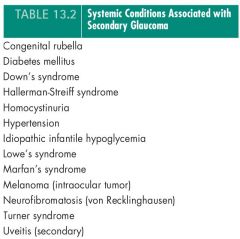
Conditions associated with glaucoma
|
|
|
|
Drugs known to cause glaucome (boxed) and type
|

|
|
|
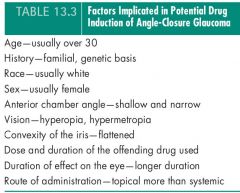
risks for angle closure glaucoma
|
|
|
|
Consequences of Increased IOP
|
Cataracts
Adhesion of Iris to Cornea Retinal and Optic Nerve damage Complete blockage of aqueous humor outflow Blindness |
|
|
What is the issue with initial diagnosis and compliance
|
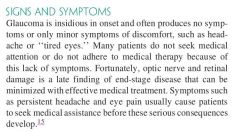
|
|
|
Clinical Presentation of open. closed and acute closed
|
Open angle
Few symptoms until visual field loss, then disease is quite advanced Acute closed angle-often symptomatic Severe pain, headache, sudden blurring of vision, pressure often >50mmHg Chronic closed angle Fewer symptoms |
|
|
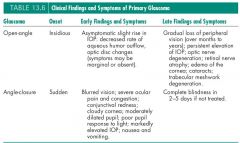
recommendations for diagnosis
|
|
|
|
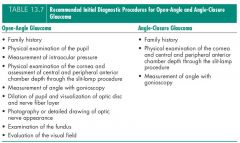
What is the order of recommended treatment
|

|
|
|
describe the surgery why is it not first line
|
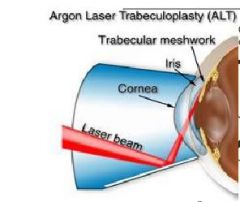
the results are not always long lasting
|
|
|
Angle Closure Glaucoma treatment
|
pilocarpine4% eye drops, 1 drop every 5 minutes for first hour
PLUS acetazolamide500 mg orally or IV, immediately, and 250 mg orally, every 6 hours until surgery OR mannitol20% 5 to 10 mL/kg (= 1 to 2 g/kg) IV over 30 minutes OR glycerol liquid 100 mL orally, with crushed ice PLUS betaxolol0.25% eye drops, 1 drop every 2 hours for the first 6 hours OR levobunolol0.25% eye drops, 1 drop every 2 hours for the first 6 hours OR timolol 0.5% eye drops, 1 drop every 2 hours for the first 6 hours PLUS brimonidine 0.2% eye drops, 1 drop every 2 hours for the first 6 hours OR apraclonidine0.5% eye drops, 1 drop every 2 hours for the first 6 hours PLUS bimatoprosteye drops 0.03%, 1 drop every 2 hours for the first 6 hours OR latanoprost eye drops 0.005%, 1 drop every 2 hours for the first 6 hours OR travaprost eye drops 0.004%, 1 drop every 2 hours for the first 6 hours. |
|
|
Prostaglandin Agonists
names mode of action indication conindication |
BIMATOPROSTLATANOPROSTTRAVOPROST
Mode of action Reduce intraocular pressure by increasing uveoscleraloutflow of aqueous humour. Indications Glaucoma Ocular hypertension Contraindications Allergy to the prostaglandin analogue Active intraocular inflammation (iritis, uveitis) |
|
|
Prostaglandin Agonists
adverse effects |
Adverse effects
Common gradual (over months to years), usually irreversible increase in iris pigmentation in treated eyes, especially those of mixed colour, egblue/brown; darkening, lengthening and thickening of the eyelashes, conjunctivalhyperaemia (usually transient) Infrequent reversible macular oedema (including cystic oedema), darkening of eyelid skin, iritisor uveitis(rare with travoprost) |
|
|
prostaglandin agonist
comparism couseling |
Comparative information
Bimatoprost, latanoprost and travoprost appear to have similar efficacy. Counselling These eye drops may slowly change the colour of your eye making the iris appear darker. This change is permanent and may be more noticeable when only 1 eye is being treated Practice points instil in the evening for optimal effect drugs in this class are structurally different; if response to one is poor, consider trying another a paradoxical increase in intraocular pressure may occur if 2ocular prostaglandin analogues are used together; avoid combination |
|
|
Beta Blockers
names mode of action indication conindication |
BETAXOLOLLEVOBUNOLOLTIMOLOL
Mode of action Reduce aqueous humour formation, probably by blockade of the beta receptors on the ciliaryepithelium. Indications All types of glaucoma Ocular hypertension Contraindications Reversible airways disease, egasthma (cardioselectiveagents, iebetaxolol, may be used with care) Bradyarrhythmia, second or third degree atrioventricularblock |
|
|
betablocker
Specific Considerations 33 Coexisting conditions |
Cardiovascular disease—consider effects of systemic beta-blockade
Treatment with systemic beta-blocker—reduces intraocular pressure (but less than with a topical beta-blocker). Adding a topical beta-blocker further reduces intraocular pressure (but this may be less effective than using an alternative class of topical agent). Risk of systemic adverse effects is increased. Treatment with verapamil—potential for profound bradycardia; avoid combination |
|
|
betablocker
adverse effects |
Adverse effects
The most important adverse effects are systemic. Common stinging on instillation (especially betaxololsolution), bradycardia Infrequent decreased corneal sensation, hypotension, syncope, fatigue, confusion, hallucinations, bronchospasm |
|
|
beta blocker
comparative |
Timolol and levobunolol(nonselectivebeta1and beta2receptor blockers), reduce intraocular pressure by 25% when used in 0.25% solution. Both agents have fewer local adverse effects than betaxolol.
Betaxolol(selective for beta1receptors) reduces intraocular pressure by about 20%. In theory, betaxololis less likely to cause bronchospasm than the nonselectiveagents but still has to be used with caution in asthmatics. Use of the suspension reduces local stinging of betaxolol, which may help compliance. |
|
|
betablocker
prative points |
a slight decrease in effect may occur during the first month of treatment; tolerance may develop after 1year or more of treatment
after stopping topical beta-blockers intraocular pressure may not return to baseline for 2–4weeks if single daily dosage is required, consider timolol gel or Timoptol-XE® |
|
|
Sympathmimetics
name drugs mode of action indication |
APRACLONIDINE
BRIMONIDINE Mode of action Reduce intraocular pressure by suppressing formation andincreasing uveoscleraloutflow of aqueous humour. Indications Chronic open angle glaucoma Prevention of ocular hypertension following laser surgery Acute closed angle glaucoma (before laser iridotomy) |
|
|
Sympathmimetics
comparative practice points |
Comparative information
Apraclonidineand brimonidinereduce intraocular pressure by 25% and 20% respectively. The effect of apraclonidineusually declines after a month; it is indicated for short term use (up to 3months). Practice points brimonidineis effective and well tolerated when used long term apraclonidineshould only be used short term for acute pressure lowering as it is associated with a high incidence of allergic blepharoconjunctivitiswith chronic use may be used by ophthalmologists in acute closed angle glaucoma or to prevent ocular hypertension following surgery |
|
|
Topical Carbonic AnhydraseInhibitors
name drugs mode of action indication contraindication |
DORZOLAMIDEMode of action
Inhibit carbonic anhydraseII (predominant subtype found in the eye) which reduces aqueous humour formation. Indications Ocular hypertension Open angle glaucoma Contraindications Sulfonamideallergy |
|
|
Topical Carbonic AnhydraseInhibitors
adverse effects counselling |
Adverse effects
Common ocular irritation, foreign body sensation, bitter taste Infrequent blepharitis, vision changes, corneal staining, GI disturbance, headache, paraesthesia, dizziness, dermatitis Counselling Your eye may feel uncomfortable for a little while after you have put in the drop. If you have blurred vision, avoid driving or operating machinery until your sight improves. Practice points may be used when beta-blocker is ineffective or not tolerated may be used with ophthalmic beta-blockers |
|
|
Acetazolamide systemic
Indications coutraindications |
Indications
Perioperativereduction of intraocular pressure, egacute closed angle glaucomaChronic open angle glaucoma where other treatments have failedEpilepsy, in particular absence seizures Contraindications Serious allergy to sulfonamidesAdrenal, respiratory or renal failure, or metabolic acidosis (increased risk of profound acidosis)Sodium or potassium depletion (is worsened)Hepatic impairment or cirrhosis (risk of hepatic encephalopathy) |
|
|
acetazolamide systemic
adverse effects tolerability |
Adverse effects
Up to 50% of patients do not tolerate acetazolamide. Adverse reactions common to sulfonamidesmay occur. Common paraesthesia (of hands, face, feet or mucocutaneousjunctions), fatigue, drowsiness, depression, decreased libido, bitter or metallic taste, nausea, vomiting, abdominal cramps, diarrhoea, black faeces, polyuria, renal stones, metabolic acidosis, electrolyte changes (hypokalaemia, hyponatraemia) |
|
|
Other Agents: Dipivefrin
mode of action practice points |
Mode of action
Pro-drug of adrenaline. Alpha-agonist effect increases aqueous outflow; beta-agonist effect decreases aqueous inflow. Practice points limited role due to poor efficacy and frequent ocular adverse effects additive effect when used with cholinergics, carbonic anhydrase inhibitors and betaxolol(less with other beta-blockers) if used in combination, instil dipivefrineat least 5minutes before beta-blocker |
|
|
Other Agents: Pilocarpine
mode of action indications and contrainidications |
Mode of action
Cholinergic effect contracts iris sphincter (miotic) and ciliarymuscle, which increases outflow through the trabecularmeshwork. Indications Chronic open angle glaucomaAcute closed angle glaucoma (2% eye drops), seek specialist advice Contraindications Uveitis(exacerbates blood–ocular barrier breakdown) Secondary glaucomasassociated with extensive outflow obstruction (ineffective, may worsen) |
|
|
Other agents Pilocarpine
adverse effects practice points |
Adverse effects
Common fluctuating blurred vision, accommodative spasm and frontal headache in people <40years (usually decreasing after 2–4weeks; simple analgesics may reduce pain), miosis, ocular irritation, follicular conjunctivitis Counselling If you are using more than one type of eye drop, put pilocarpine drops in last. These eye drops may cause blurred vision. Do not drive or operate machinery if you are affected. Practice points reassess visual acuity for driving |
|
|
Glaucoma general treatment practice points
|
- compliance is big issue, check before adding new drug, education and simplifying drug regimen may help.
-IOP target is individualised to site, retinal damage, expected life span, family history determined by specialist -treatment asses by IOP, and visual dield changes, optic disk appearance there is evidence that PG analogues are more effective than timolol in reducing IOP, and maintain long term efficacy ongoing surveillance of iris pigmentation is necessary if PG analogues are used; reassure patients that iris pigmentation and lash thickening does not affect efficacy of the drops |
|
|
glaucoma treatment general advice for patients
|
teach patients to reduce systemic absorption (by up to 70%) by closing eyes and pressing on the tear duct for 3minutes after instillation of each eye drop
when >1type of eye drop is to be instilled at the same time, separate administration by at least 5minutes |
|
|
The macula, what is it.
|
is the central, posterior portion of the retina containing the densest concentration of photoreceptors within the retina
It is responsible for central high-resolution visual acuity, allowing a person to see fine detail, read, and recognise faces Posterior to the photoreceptors lies the retinal pigment epithelium, and posterior to this lies Bruch‘s membrane, a semipermeableexchange barrier that separates the retinal pigment epithelium from the choroid The choroid supplies blood to the outer layers of the retina |
|
|
What are drussen and how are they involved in macula degenerative
|
With age, one change that occurs within the eye is the focal deposition of acellular, polymorphous debris between the retinal pigment epithelium and Bruch‘s membrane.
These focal deposits, called drusen(singular ―druse‖), are observed during funduscopicexamination as pale, yellowish lesions and may be found in both the macula and peripheral retina Drusenare ubiquitous in people over 50 and are considered a part of normal aging. Excess drusen, however, can lead to damage to the retinal pigment epithelium and destruction of the macula |
|
|
what are the two types of macula degeneration and what are the clinical outcomes
|
Significant visual loss occurs when a complication of the drusendevelops, either a choroidalneovascularmembrane (‗wet AMD‘) or atrophic (‗dry AMD‘)
In neovascularAMD, abnormal blood vessels from the choroid grow up under the retina. This causes acute loss of vision when transudateor haemorrhage accumulates beneath the retina, leading ultimately to a fibrous scar This results in progressive and irreversible loss of central vision and often becomes bilateral over a period of years In atrophic AMD the retina slowly becomes atrophic over months to years and as such central vision is gradually lost. The majority of AMD is atrophic, however most patients with severe visual impairment have neovascularAMD. |
|
|
AMD -Management - lifestyle
|
All smokers should be counselled to quit smoking
Smokers may not be fully aware of their increased risk for visual loss, and the possibility of legal blindness may be an important motivator for smoking cessation People who stop smoking for >20 years are no longer at increased risk for AMD Decrease dietary intake of fat, maintain healthy weight and blood pressure, and increase dietary intake of antioxidants through foods such as green leafy vegetables, whole grains, fish, and nuts For patients with severe visual loss, low-vision devices such as electronic video magnifiers and spectacle-mounted telescopes, as well as low-vision rehabilitation services, may also be of benefit |
|
|
AMD antioxidant supplementation, benefits and risk
|
Age-Related Eye Disease Study (AREDS)
Daily antioxidant supplement (PreserVision, Bausch & Lomb -vitamin C (500 mg), vitamin E (400 IU), beta carotene (15 mg), zinc oxide (80 mg), and cupric oxide (2 mg) reduced the rate of progression from intermediate to advanced AMD by 25% over a 5 year period, resulting in a 19% reduction in the risk of moderate visual loss Note that this supplement may not be considered appropriate for all patients Beta-carotene supplementation may increase in the relative risk of the development of lung cancer in smokers by 17% High-dose vitamin E supplementation has been associated with an increased risk of death and heart failure amongst people with diabetes or cardiac disease But the AREDS intervention group displayed a trend toward a reduced risk of death |
|
|
Anti-VGEF therapies - benefits, mechanism?, risks
|
Intravitrealantiangiogenictherapy (injection of agents that inhibit blood vessel growth directly into the vitreous) is currently the primary therapy for wet AMD
Such injections localize therapy to the eye, avoiding systemic administration and possibly reducing the incidence of systemic adverse effects Anti-VEGF agents administered systemically have been associated with serious systemic adverse events, e.g. thromboembolicevents and death. The exact stimulus for the neovascularprocess that occurs in wet AMD is unknown, but vascular endothelial growth factor (VEGF) seems to play a key role VGEF is a common growth factor expressed in many cells and malignant tumours that promotes angiogenesis and permeation of endothelial cell |
|
|
Anti VGEF therapies - drugs, adminestration
|
There are two anti-VEGF drugs currently available in Australia, bevacizumaband ranibizumab
Bevacizumabis significantly cheaper than ranibizumab(~$42 vs~$2000 per injection) But bevacizumabis currently only licensed for certain cancers, not AMD Procedures are generally performed in an outpatient setting with the use of an aseptic technique and a topical or subconjunctivalanesthetic. 4 agents currently used in Australia RanibizumabLucentis® BevacizumabAvastin® AnecortaveRetaane® VerteporfinVisudyne |
|
|
Other therapies - (assumed wet AMD)
|
Verteporfin
A photosensitiser that is administered prior to laser treatment of the affected area in the retina Light is absorbed by the photosensitiser molecules, which causes an oxidation process in lipid membranes and proteins, slowing vision loss generally does not improve vision, and less efficacious than other treatments when used as monotherapy Well tolerated, although patients should avoid sunlight exposure for 48 h after treatment Anecortave a synthetic angiostaticsteroid that prevents vascular growth by inhibiting proteases necessary for endothelial cell migration no glucocorticoidactivity (no concern with HPA suppression) and a good ocular safety profile |
|
|
Cataracts - what is it, risks
|
A cataract is any opacity in the lens
Ageing most common cause; pathogenesis not well understood protein aggregates scatter light rays and reduce lens transparency Other factors can be involved, e.g. trauma, toxins, systemic disease (e.g. diabetes), smoking, heredity Also associated with long term administration of corticosteroids (systemic or topical), some phenothiazines, amiodarone Age-related cataracts common cause of visual impairment 50% aged 65–74; 70% for those over 75 |
|
|
cateract treatment
|
Replacement of clouded lens with intraocular lenses (IOL)
Postoperative therapy may involve combinations of topical antibiotics (e.g. chloramphenicol) and NSAIDS (e.gketorolac) and/or corticosteroids (e.gfluoromethalone) |

