![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
Development of the spinal cord |
Develops from the posterior or inferior segment of the neural tube.It preserves the metamerism (segmental structure).Each segment of the body (somite) has the appropriate region on the neural tube - neuromer that is responsible for segment innervation. |
|
|
Latin term for spinal cord |
Medulla spinalis |
|
|
Length of the spinal cord |
45cm in males 41-42cm in females |
|
|
Ends of the spinal cord |
Above (cranially), it is continuous with the medulla oblongata Below (caudally), it terminates as a conic tip called conus medullaris at the level of the 2LV (3LV in newborns) |
|
|
Significance of the apex of conus medullaris |
It continues down as filum terminale - the atrophied segment of the spinal cord that is covered with the pia mater and attached to the 2nd Coccygeal Vertebra. [[Useful when performing several medical procedures to avoid damage of the spinal cord in lumbar puncture to obtain cerebrospinal fluid or to provide spinal anasthesia the needle must be inserted in the interspace between 3rd and 4th lumbar spines]] |
|
|
External structure of the spinal cord |
1. Has two enlargements along its length called intumescentia cervicalis (upper cervical enlargement) and intumescentia lumbalis (lower lumbar enlargement) - they correspond to the roots of the nerves of the upper and lower limbs 2. It is symmetrical in structure • White matter is divided into right and left halves in front by fissura mediana anterior and behind by sulcus medianus posterior • The lateral surface of each half has sulcus anterolateralis (where anterior motor root leaves the spinal cord) and sulcus posterolateralis (where the posterior afferent roots enter the spinal cord) |
|
|
Posterior root of the spinal cord |
Radix dorsalis Has an enlargement called ganglion spinale that contains pseudounipolar neurons. The dendrite enters the structure of the spinal nerve and ends as a receptor in tissues. The axon goes in the structure of the posterior root and enters the spinal cord. |
|
|
The anterior root of the spinal cord |
Radix ventralis Consists of axons of the anterior horn neurons. |
|
|
Where do the anterior and posterior roots of the spinal cord meet? |
They meet near the intervertebral foramen and form the trunk of the spinal nerve (funiculus) |
|
|
What constitutes a spinal segment? And how many spinal segments do we have? |
The portion of the spinal cord which gives the origin to the roots of one pair of spinal nerves constitutes a spinal segment. We have 31 spinal segments: 8 Cervical 12 Thoracic 5 Lumbar 5 Sacral 1 Coccygeal |
|
|
How can spinal nerves reach the intervertebral foramina of the lumbar, sacral and coccygeal vertebrae if the spinal cord is shorter than the vertebral column? |
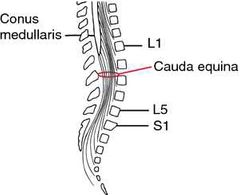
The spinal cord terminates as the conus medullaris whose apex is called filum terminale and then continues down the vertebral canal as several separate nerve fibers that extend downward and leave through the remaining intervertabral foramina. Since this bundle of nerves arising from the filum terminale of conus medullaris looks like a horse's tail, it is called cauda ecquina |
|
|
Internal structure of the spinal cord |
1. Canalis centralis is at the center. It is the residue of the primary nervous tube cavity. 2. From above, the canal is connected to the 4th ventricle of the brain and from below, at the location of the conus medullaris, it ends as an enlargement known as terminal ventricle 3. Substansia grisea / grey matter is visible on a transverse section of the spinal cord (in the form of an "H") The grey matter on Each half of the cord consists of: • cornu anterius • cornu posterius (The space between the anterior amd posterior horns is called intermediate substance) • And in the Thoracic and Lumbar (C8-L3) and Upper Sacral (S2-S4) segments, there is also cornu laterale
|
|
|
Differences between anterior, lateral and posterior horns |
1. By function The anterior horn is motor; The lateral horn is afferent (autonomic nervous system); The posterior horn is sensory in function. 2. By Arrangement of cells Anterior horn : Cells are arranged in groups: medial (ventromedial, dorsomedial), lateral (ventrolateral, dorsolateral) & central nuclei.
Posterior horn : Internuncial neurons that form afferent nuclear group.
Lateral horn : nucleus intermediolateralis which acts as a vegetative/autonomous nuclear column. It is seen at 2 levels: 1. From C8 to L3 segments Giving rise to preganglionic sympathetic fibers 2. From S2 to S4 segments Giving rise to preganglionic parasympathetic fibers (mostly for pelvic viscera) |
|
|
Main afferent nuclei of the posterior horn |
1. Substancia gelatinosa 2. Nucleus proprius 3. Nucleus thoracicus
Afferent nucleus is also present in the INTERMEDIATE SUBSTANCE near the central canal called nucleus intermediomedialis which serves to conduct unconscious proprioceptive (being aware of body position and movement) impulses to the cerebellum |
|
|
Substancia gelatinosa |
Found at the tip of the posterior horn. It is a relay station for touch and stereognosis (mental perception of depth- 3D) The nucleus is concerned with sensory associated mechanism. Its axons give rise to the anterior spinothalamic tract |
|
|
Nucleus proprius |
It lies subjacent to the substancia gelatinosa It acts as a relay station for pain and temperature. It is concerned with sensory associated mechanism Its axons give rise to the lateral spinothalamic tract |
|
|
Nucleus thoracicus (dorsalis) |
A relay nuclear column for reflex or unconscious proprioceptive (mental perception of depth - 3D) impulses to the cerebellum. Its axons give rise to the posterior spinocerebellar tract |
|
|
What is the grey matter of the spinal cord surrounded by? |
White matter / substancia alba |
|
|
Columns / Funiculi and Fasculiof the white matter |
The funiculi are divided by the dorsolateral sulcus and the site of emergence of the anterior roots from the spinal cord. 1. Funiculus anterior 2. Funiculus lateralis 3. Funiculus posterior
Sulcus intermedius posterior divides the cervical and superothoracic segments of the posterior funiculus into Two Fasciculi: 1. Fasciculus gracilis (Column of Goll) 2. Fasciculus cuneatus (Column of Burdach) Both of them pass above to the posterior surface of the medulla oblongata and known there by the same names. |
|
|
In each funiculus, short fibers that connect various segments of the spinal cord are placed adjacent to the grey matter to form _____________________. |
Proper fascicles / Fasciculi proper |
|
|
What do the fasciculi proper and nuclei of grey matter form together? |
The proper apparatus of the spinal cord which ensures reflex activity. |
|
|
Tract |
Long fibers that connect two masses of grey matter within the central nervous system. They may be ascending or descending tracts. They ensure conduction activity or two-way connecting apparatus of the spinal cord |
|
|
Funiculus Posterior |
1. Composed of afferent tracts -> Fasciculus gracilis and Fasciculus cuneatus 2. These fascicles are collections of the central processes of the pseudounipolar neurons of the spinal ganglia. 3. The fascicles reach the same-named nuclei of the medulla oblongata and carry conscious proprioceptive impulses (deep touch, pressure, tactile localization, tactile discrimination and stereognosis) from receptors placed in muscles, bones, tendons and joints. |
|
|
Funiculus Lateralis |
1. Has both afferent and efferent tracts
2. Sensory pathways contain axons of the afferent nuclei of the posterior horn cells, that are directed to different parts of the brain: 1) To the cerebellum: tractus spinocerebellaris posterior (Flechsig's tract) and tractus spinocerebellaris anterior (Gower's tract) to carry reflex (unconscious) proprioceptive sensations (kinesthesia) 2) To the tectum of midbrain: tractus spinotectalis (to subcortical centers of vision and hearing) 3) To the thalamus of the diencephalon: tractus spinothalamicus anterior (tactile sense) and tractus spinithalamicus lateralis (pain and temp. Feeling)
3. The motor descending tracts start from the brain and end in the spinal cord : 1) From pyramidal cells of the brain cortex : tractus corticospinalis lateralis (conscious motor tract of the pyramidal system) 2) From the red nuclei of the midbrain: tractus rubrospinalis (Monakow's tract) - the extrapyramidal tract for muscle tone maintenance. 3) From the olive of the medulla oblongata: tractus olivospinalis (pathway of balance)
|
|
|
Funiculus anterior |
1. Contains only motor tracts 1) From the tectum of the midbrain : tractus tectospinalis, provides the protective movements due to the visual and acoustic stimuli, this is the visual and auditory reflex tract. 2) From the brain cortex : tractus corticospinalis anterior (conscious motor tract of the pyramidal system) 3) From the reticular formation of the brainstem: tractus reticulospinalis (extrapyramidal tract) 4) From the vestibular nuclei of the pons : tractus vestibulospinalis (provides regulation of the muscle tone and movements coordination) 5) Fasciculus longitudinalis medialis : can be found upto the upper thoracic segments. It connects the motor nuclei of the eye muscle nerves with each other and with the motor nuclei of the spinal cord thus the coordinative work of eyes and head muscles is provided. |
|
|
What is the spinal cord invested in? |
The spinal cord is invested in three connective tissue membranes (meninges) derived from the mesoderm around the neural tube. 1. Dura mater / Pachymeninx (Externally) 2. Arachnoid mater / arachnoidea 3. Pia mater (Innermost) Arachnoid mater and pia mater are together known as leptomeninges Cranially, all three membranes are continuous with similar membranes of the brain |
|
|
Dura mater |
1. Dura mater spinalis. 2. Made up of 2 layers: outer endosteal layer (endorrhachis) and inner meningeal layer. 3. In between of dura mater and vertebral column is the extra dural space (cavitas epidurale) which contains fat and the internal vertebral plexus into which venous blood from the spinal cord and vertebrae flows. 4. The inner surface of the dura mater is covered with an endothelial layer which gives it a smooth, shiny appearance. 5. Cranially, the dura mater fuses with the margins of the foramen magnum of the occipital bone and caudally, terminates at the level of 2SV or 3SV as a thread like filum durae matris spinalis which is attached to the coccyx.
6. The dura mater receives arteries from spinal branches of segmental arteries . Its veins drain into internal vertebral venous plexus Nerves arise from the meningeal branches of the spinal nerves
|
|
|
Arachnoid mater |
1. Arachnoidea spinalis 2. A thin transparent membrane that loosely surrounds the spinal cord. 3. Adjoins the internal surface of the dura mater but separated from it by a slit-like space called the subdural space or cavum subdurale pierced with thin trabeculae 4. Between the arachnoid and pia mater is the subarachnoid space or cavum subarachnoidale in which the spinal cord and nerve roots lie freely surrounded by a lot of cerebrospinal fluid or liquor cerebrospinalis 5. The subarachnoid space is especially enlarged in the lower part of the arachnoid sac where it surrounds the cauda ecquina of the spinal cord - cysterna terminalis 6. The fluid in the subarachnoid space of the spinal cord continuously communicates with the fluid filling the subarachnoid space of the brain and its ventricles. 7. Septum cervicale intermedium (posterior median cervical septum) forms on the midline in the back of the cervical region between the arachnoid and pia mater covering the spinal cord. 8. Triangular shaped membranous extensions which are thickenings of the pia mater called denticulate ligament (ligamentum denticulatum) suspend in the middle of its dural sheath and consists of 19-23 projections that are projected laterally and fuse with the arachnoid mater and inner surface of the dura mater along the length of the spinal cord within the nerve roots of the spinal nerves on either side. They protect the spinal cord against shock and sudden displacement. 9. Both ligamenta denticulata divide the subarachnoid space into anterior and posterior parts. |
|
|
Pia mater |
1. Pia mater spinalis 2. A thin transparent connective tissue layer that adheres to the surface of the spinal cord. 3. It consists of collagen and elastic fibers and contains many blood vessels that supply nutrients and oxygen to the spinal cord. |
|
|
Cerebrospinal fluid |
1. Modified clear, colourless tissue fluid that contains glucose, proteins, lactic acid, urea, cations and anions as well as some lymphocytes. 2. Contained in the ventricular system of the brain and the subarachnoid space around the brain and spinal cord. 3. CSF replaces lymph in the CNS 4. Total quantity of CSF is about 150ml. 5. Formed at the rate of 200ml per hour or 5000ml per day 6. Normal pressure of CSF is 60 to 100mm of water. 7. It is a protective, nutritive substance and a pathway for metabolites from the CNS. 8. Can be obtained by: a) Spinal tap (lumbar puncture) b) Cysternal puncture c) Ventricular puncture |
|
|
Spinal tap (lumbar puncture) |
Easiest and most commonly used method.In an adult, a spinal tap is normally performed between 3LV-4LV and in children between 4th-5LV.This region is inferior to the lowest portion of the spinal cord and provides relatively safe access. (A line drawn across the highest points of the iliac crests, the supracristal line, passes through the spinous process of the 4LV) |

