![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
120 Cards in this Set
- Front
- Back
|
Anemia |
A decrease in the ability of the blood to carry oxygen to the tissues. |
|
|
Anemia is a decrease of ______________________. |
Hemoglobin or erythrocytes. |
|
|
Anemia isn't a disease, but rather: |
An expression of an underlying disease or disorder. |
|
|
Adaption of anemia depends on: |
Rate of onset, severity of blood loss, and ability of the body to adapt. |
|
|
Adaptions to anemia: |
Increase in cardiac rate, increase in cardiac output, increase in circulation rate, and preferential increase in blood flow to vital organs. |
|
|
Morphological classifications of anemia |
Macrocytic/Normochromic Normocytic/Normochromic Microcytic/Hypochromic |
|
|
Etiological classification of anemia |
Decreased production of RBCs, increased RBC destruction or loss, and hemoglobinopathy (hemoglobin disease). |
|
|
Morphology of macrocytic anemias |
Macrocytic normochromic. |
|
|
Megaloblastic anemia |
Due to abnormal DNA synthesis (nuclear maturation defect which leads to asynchronous maturation of RBCs). Most often due to vitamin b12 or folate deficiencies. |
|
|
Non megaloblastic anemia (normoblastic) |
Cause isn't well defined; can be related to an increase in membrane lipids. |
|
|
How is b12 related to folate? |
B12 is a cofactor in the conversion of methyl tetrahydrofolate (folic acid) to tetrahydrofolate. |
|
|
The product of folic acid to tetrahydrofolate is a cofactor needed for: |
Production of DNA thymidine. |
|
|
What does thymidine synchronize? |
The cells in the s phase of mitosis. |
|
|
What are 95% of megaloblastic anemias caused by? |
B12 or folic acid deficiencies. |
|
|
Vitamin b12 deficiencies are usually secondary to a deficiency in _____________ vs a ____________ deficiency. |
Intrinsic factor, nutritional deficiency. |
|
|
Most cases of folic acid deficiency (megaloblastic anemia) are due to ____________________. |
Nutritional deficiency. |
|
|
What kind of inherited disorders of megaloblastic anemia are rare? |
Disorders affecting the synthesis of DNA. |
|
|
What is intrinsic factor? |
Comes from parietal cells in the stomach. If absent, can't absorb folic acid. |
|
|
Sources of vitamin b12 |
Liver/meat Milk and eggs Mollusks/clams Fish Fortified cereals |
|
|
Dietary sources of folic acid |
Green leafy veggies Dried peas and beans Mushrooms, yeast |
|
|
Where is vitamin b12 stored? |
Liver, heart, and kidneys. |
|
|
Hematological findings in megaloblastic anemia |
🔺 MCV Normal MCH 🔻 RBC, WBC, platelets, retic count Macrocytisis of RBCs. Basophilic stippling Howell jolly bodies Schistocytes and target cells Hyper segmented neutrophils, oval shaped RBCs. |
|
|
What is the first and last thing to be seen in megaloblastic anemia morphology? |
Hyper segmented neutrophils. |
|
|
Clinical findings in megaloblastic anemias |
Seen more in women, usually affects middle age or older, SOB, light headedness, weakness, pallor, glossitis, and megaloblastic madness. |
|
|
Megaloblastic madness |
Only seen with b12 deficiencies. Brain needs b12. Dementia can develop. |
|
|
Pernicious anemia |
Autoimmune disorder caused by a 🔻 of IF that is secreted by parietal cells of gastric mucosa. |
|
|
What % of pernicious anemia patients have antibodies against parietal cells? |
90. |
|
|
What is IF necessary for? |
Absorbing b12. |
|
|
Most common cause and what % of b12 deficiencies |
Pernicious anemia, 85%. |
|
|
Other causes of b12 deficiencies |
Partial or complete gastrectomy and gastric atrophy associated with aging. |
|
|
Lab diagnosis of pernicious anemia |
Gastric analysis, shilling test, serum vitamin b12 assay, methylmalonic acid assay. |
|
|
What is MMA? |
Serum analysis of b12 and MMA confirm the decrease of b12, but can't distinguish pernicious anemia from other causes of b12 deficiency. |
|
|
Which tests are specific for pernicious anemia? |
Gastric analysis and the shilling test, but aren't commonly performed. |
|
|
Shilling test part 1 |
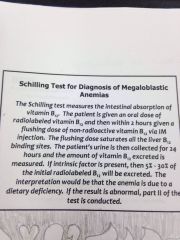
Back (Definition) |
|
|
Part 2 of shilling test |
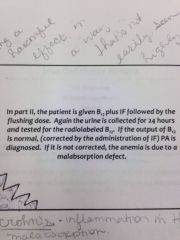
Back (Definition) |
|
|
Folate deficiency can occur to one of the following reasons: |
1. Inadequate intake: seen in the poor and elderly. 2. Increased requirement: hemolytic anemias and pregnancy. 3. Malabsorption 4. Drug inhibition: oral contraceptives, long term anticoagulant use, anti seizure meds: phenobarbital, primidone, and phenytoin. |
|
|
Other causes of megaloblastic anemia |
Strict vegetarian, malabsorption syndromes (tropical sprue or chronic wasting and non tropical sprue aka gluten sensitive enteropathy), Crohn's disease, infection with diphyllobothrium latum, and chemotherapy drugs. |
|
|
Most common cause of non anemic macrocytosis and associated conditions. |
Alcoholism. Folate deficiency due to decreased dietary intake, reticylocytosis due to hemolysis or GI bleeding, liver disease, and alcohol toxicity to erythroid precursors. |
|
|
Other conditions that contribute to macrocytic anemia without megaloblastosis |
Liver disease, hemolysis or post hemorrhagic anemia, hypothyroidism, and aplastic anemia. |
|
|
Primary storage site of folate |
Liver. |
|
|
Non megaloblastic anemia hematological findings |
Normal WBC, platelet count. 🔻 RBC and H&H MCV < 100 fl Polychromasia, target cells, stomatocytes in liver disease, schistocytes in hemolytic anemia. NO hyper segmented neutrophils. |
|
|
Where is most iron stored? |
Liver |
|
|
Ferritin |
Primary storage compound. Spherical protein shell that can store 4500 iron atoms. |
|
|
Hemosiderin |
Molecule of carbohydrate, lipid, protein, and iron. |
|
|
Where is hemosiderin primarily found and what is it formed by? |
Primarily in macrophages and formed by partial degradation of ferritin. |
|
|
Each gram of transferrin binds ___ mg of iron. |
1.4 |
|
|
Enough transferrin is present in plasma to bind _____________ micrograms of iron/dL of plasma. This is referred to as _______________________________. |
253-435. Total iron binding capacity. |
|
|
Serum concentration is _______ micrograms/dL and ___% is complexed with transferrin. |
70-201, 95. |
|
|
Cell morphology of iron deficiency anemia |
Microcytic, hypochromic. |
|
|
Etiology of IDA in neonates |
Maternal iron deficiency, multiple births. |
|
|
Etiology of IDA in premenopausal women |
Menstrual blood loss, inadequate diet and malabsorption, pregnancy. |
|
|
Etiology of IDA in adult males and postmenopausal women |
Chronic blood loss, inadequate diet, GI tract disease: peptic ulcers, malignancies, excess aspirin ingestion, alcohol gastritis, hookworms, and hemorrhoids. |
|
|
Number one cause of IDA in adult males and postmenopausal women |
Chronic blood loss. |
|
|
Etiology of IDA in infants and children |
Growth spurts, inadequate diet, and malabsorption. |
|
|
Etiology of IDA not related to age or sex |
Inherited or acquired bleeding disorders and hemodialysis. |
|
|
What is heme iron derived from? |
Hemoglobin, the protein in RBCs that deliver oxygen to cells. |
|
|
What is heme iron found in? |
Animal foods that originally contained hemoglobin, such as red meats, fish, and poultry. |
|
|
How is iron in plant foods arranged? |
Into a chemical structure called nonheme. |
|
|
What form of iron is added to iron enriched foods? |
Nonheme. |
|
|
Which form of iron is absorbed easier? |
Heme iron. |
|
|
Most dietary iron is what type? |
Nonheme. |
|
|
Most common nutritional deficiency |
Iron deficiency. |
|
|
Beverages that complement absorption of iron |
Orange juice, vitamin c, pickles, vinegar, alcohol. |
|
|
Beverages that impede absorption of iron |
Coffee, tea, milk. |
|
|
Clinical findings of IDA |
Insidious onset: over several years or months, early stages usually show no s/s. Fatigue, pallor, lethargy, dyspnea, cold intolerance, palpitations, pica, chelitis, and koilonychia. |
|
|
Hematological findings of IDA |
🔻 MCV & MCHC Slight 🔺 of RDW Target cells 🔻 serum iron and ferritin 🔺 TIBC Platelets may be 🔺 of due to hemorrhage |
|
|
Treatment of IDA |
Treatment of underlying disorder and iron therapy through drops or pills. |
|
|
What forms are iron preparations available in and what are the side effects? |
Ferrous sulfate, ferrous gluconate, and ferrous fumerate. Side effects include: constipation, stomach discomfort, or diarrhea. |
|
|
What is seen in morphology when iron therapy is working? |
Retics or polychromasia. 3 days after treatment is started. Peaks at 10 days. |
|
|
How long does it take for a patient to get back to normal after iron therapy? |
6-10 weeks. |
|
|
Morphological classification of anemia of chronic disorders |
Normocytic/normochromic; can become normocytic/hypochromic and in long standing cases, microcytic/hypochromic. |
|
|
2nd most common anemia |
Anemia of chronic disorders. |
|
|
Etiology of anemia of chronic disorders |
Chronic infections, rheumatoid arthritis, malignancies, organ failure, and lupus. |
|
|
Contributing factors of anemia of chronic disorders |
Reduced RBC life span, uncompensated bone marrow production, decreases iron transfer from the MPS storage sites to marrow. |
|
|
What is iron blocked from? (Anemia of chronic disorders) |
Release from macrophages by hepicidin. |
|
|
What is hepicidin produced in response to? |
Interleukin 6 and other inflammatory cytokines. |
|
|
Etiology of sideroblastic anemia |
Iron loading in the mitochondria due to a defect in heme synthesis. |
|
|
Inherited sideroblastic anemia etioligy |
Sex linked and autosomal recessive. |
|
|
Idiopathic sideroblastic anemia |
Referred to as refractory anemia with ringed sideroblasts or RARS. Result of stem cell disorder. |
|
|
Secondary sideroblastic anemia |
Secondary to drugs or chemicals, alcoholism, lead poisoning, may be seen in patients who need chronic transfusion, food faddists that take megavitamins. |
|
|
Morphological classification of sideroblastic anemia: inherited and acquired secondary form |
Dimorphic population of normocytic/normochromic and microcytic/hypochromic and dual populations of macrocytes and microcytes or normocytes. |
|
|
Where are macrocytic/hypochromic cells seen in (sideroblastic anemia)? |
RARS |
|
|
Treatment of sideroblastic anemia |
1. Pyridoxine (vitamin b6) although only effective in less than 50%. 2. Phlebotomy 3. Folic acid for those with macrocytic features. 4. Secondary forms are treated by treating the underlying disease or removing the toxic agent. |
|
|
Hemochromatosis |
Disease in which body absorbs and stores more iron than needed. Since the body has no natural way of ridding excess, iron is stored in tissue, especially in liver, heart, and pancreas. |
|
|
How old are most patients when they experience s/s of hemochromatosis? |
50s or 60s. |
|
|
Two forms of hemochromatosis |
Hereditary and secondary. |
|
|
Characteristics of hemochromatosis |
Increased iron absorption in the gut and progressive iron overload. |
|
|
# of people who get hereditary hemochromatosis |
1 in 200-250. 1 in 10 Caucasians in US is a carrier. |
|
|
Most common genetic abnormality in those with a European ancestry and how many genes are responsible? |
Hereditary hemochromatosis. 5. |
|
|
Which sex is more effected with hereditary hemochromatosis? |
Males. |
|
|
Secondary causes of hemochromatosis |
Anemias with ineffective RBCS. Chronic transfusions Chronic liver disease Viral hepatitis Dietary iron overload Mega dosing with iron supplements Alcoholism |
|
|
Lab findings of hemochromatosis |
*Ferritin greater than 200 in premenopausal women and greater than 300 in men and postmenopausal women. *🔺 ferritin, iron, and transferrin *TIBC normal
|
|
|
Bronze diabetes |
Can develop with hemochromatosis due to accumulation of iron in the tissues which leads to a peculiar skin discoloration. Pancreas becomes fibrotic and nonfunctional due to the iron deposits. |
|
|
Treatment of hemochromatosis |
Therapeutic phlebotomies. Reduces ferritin levels and the hematocrit level is maintained at 35%. Can also be given an iron chelating agent - Desferal. Excreted in urine. |
|
|
Anemia of blood loss morphology |
Normocytic/normochromic |
|
|
Etiology of anemia of blood loss |
Sudden blood loss. After an acute major blood loss, the H&H will stay normal for several hours due to vasoconstriction. After this time, fluid enters the circulation and the H&H and RBC 🔻. |
|
|
Anemia of chronic renal insufficiency morphology |
Normocytic/normochromic with fragmented RBCs and burr cells. |
|
|
Anemia of chronic renal insufficiency etiology |
Due to damage of the kidneys and subsequent underproduction of erythropoietin (hormone that makes RBC). |
|
|
What chemistry levels are increased with anemia of chronic renal insufficiency? |
BUN and creatinine. |
|
|
Therapy for chronic renal disease includes: |
*Renal transplant *Dialysis *EPO |
|
|
Dialysis: treatment of renal disease |
Can cause additional causes of anemia including blood loss, iron and folate deficiency, and hemolysis. Patient can develop a macrocytic or microcytic anemia without proper supportive therapy. |
|
|
Aplastic anemia morphology |
Normocytic/normochromic. |
|
|
Acquired aplastic anemia |
Due to damage to the pluripotential stem cells resulting in pancytopenia. |
|
|
Damage to stems cells may be due to: |
An antibody that attaches to antigens on stem cells or an immune mechanism. That causes t lymphs to suppress stem cell division. |
|
|
Common causes of acquired aplastic anemia |
Radiation, certain drugs, viruses, and exposure to certain chemicals. Most of the time the offending agent can't be identified and is idiopathic. |
|
|
Age groups aplastic anemia is found in |
2-5 years 15-25 years Adults over 60 |
|
|
Occurrence of aplastic anemia in children is mostly due to: |
Inherited forms, while most adult cases are acquired. |
|
|
There are more cases of aplastic anemia in what geographical location? |
Asia probably due to environmental and occupational factors. |
|
|
Idiopathic aplastic anemia % |
Approx 50-70%. |
|
|
Acquired form of aplastic anemia: drugs |
Approx 30% of cases. |
|
|
Acquired aplastic anemia: chemicals |
Industrial chemicals such as benzene and chemotherapy. |
|
|
Acquired form of aplastic anemia: ionizing radiation |
Industrial accidents, military nuclear tests, and radiation therapy. |
|
|
Acquired aplastic anemia: infectious agents |
Viral and bacterial infections can be followed by transient cytopenia. |
|
|
Inherited (constitutional) aplastic anemia |
Aka Fanconi anemia. Autosomal recessive disorder resulting from a heterogenous molecular defect and is characterized by abnormal chromosomal fragility. |
|
|
# effected with inherited aplastic anemia |
1 in 350,000 live birth in North America and has a heterozygote frequency in approx 1 in 300,000. |
|
|
Anemia develops in _____ of Fanconi patients, usually between the ages of ______. |
90%, 5-10. |
|
|
Clinical findings of fanconi's anemia |
🔺 hgb F Cutaneous hyperpigmention Hypogonadism Skeletal disorders: mostly thumbs Microcephaly Mental retardation |
|
|
Treatment of inherited aplastic anemia |
Removal of drug/environmental cause and bone marrow transplant. |
|
|
Survival rates for aplastic anemia bone marrow transplants |
90% for identical twins and 35% for mismatched donors. |
|
|
Clinical findings of HH |
*arthralgia *lethargy *abdominal pain *cardiac problems |

