![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
121 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is the internal largest organ in the body |
Liver |
|
|
|
Why dose the liver genarate heat |
Lots of matabolic activity happens in the liver |
|
|
|
What is the role of the liver |
Protein and glucose metabolism |
Ooo I am just gonna
|
|
|
Which two vessels supplies blood to to the liver |
Hepatic portal vein ( from the intestines) blood has high concerntrations of glucose amino acids basically digested food products after meal Hepatic artery ( from the aorta) oxygenated blood |
|
|
|
Blood leaves the liver by ? |
Hepatic vein (transports deoxygenated blood to vena cava) |

|
|
|
What happens to all the food materials absorbed from the digestive system |
They pass to the liver where they are stored or converted into any form that’s required by the body. |
|
|
|
What happens to all the food materials absorbed from the digestive system |
They pass to the liver where they are stored or converted into any form that’s required by the body. |
|
|
|
reactions that takes place in the liver |
1 regulation of blood glucose levels 2 protein metabolism 3 haemoglobin metabolism 4 fat metabolism 5 alcohol metabolism 6 drug metabolism |
|
|
|
Which vessel dose sugers such as glucose from the gut enter the liver with? |
Heptic portal vein |
|
|
|
Define homeostasis |
Physiological control system that maintain the internal environment within restricted limits ( maintains constant internal environment) |
|
|
|
Factors that is controlled by homeostasis? |
-Core body temperature ( stable temperature to provide optimum temperature for enzyme activity. Low temp not enough kenetic energy for optimum enzyme activity. High temperature enzyme denatures) - blood PH ( needs to be stable to provide an optimum PH for enzyme activity. Extreme changes in ph causes denaturation) - blood glucose concerntration ( stable blood concerntration needed to provide enough substantiate for respiration to release energy for metabolic processes in the body) - water potential of the blood ( water potential of the blood needs to be within restricted limits) |
|
|
|
What rely on negative feedback |
The physiological control system used in homeostasis |
|
|
|
What is negative feed back |
Process in which your body reverse a change that’s occurring eg high or low blood glucose, high or low body temperature. Restores system to their original level |
|
|
|
When is negative feedback stimulated |
Divisions from norm (original level) |

|
|
|
What happens when blood glucose increases ( after meal ) |
- high blood glucose levels is detected by the pancreas - pancreas’s beta cells releases insulin into the blood - insulin attaches to receptors on surface of target cells eg liver and muscle cells - insulin increases the permeability of target cells to glucose. By stimulating the inclusion of more channel proteins in the membrane, which allows glucose to enter, reducing blood glucose concerntration. - insulin also activates enzymes in liver and muscle that convert glucose into glycogen (glycogenesis). Excess glucose is converted to fat when glycogen stores are full. This corrective mechanism causes the blood glucose concerntration to decrease and inhibits insulin production by negative feedback. |
|
|
|
What is glycogenesis |
The conversion of glucose to glycogen |
|
|
|
What happens when blood glucose is low eg during fasting or exercise. |
-Low level of blood glucose detected by the pancreas. - the pancreas’s alpha cells secretes the hormone glucagon into the blood. - glucagon attaches to specific receptors on the surface of target cells of the liver and activates enzyme which hydrolyse glycogen into glucose( glycogenesis) the glucose is released to the blood. Blood concerntration is increased. - when glycogen stores are finished and there is a high demand in glucose. Then glucagon activates enzyme which convert glycerol and amino acid into glucose ( gluconeogenesis) glucose released into the blood This corrective mechanism causes the blood glucose concerntration to increase to normal, and inhibit glucagon secreation by negative feedback |
|
|
|
Define glycogenolysis |
When glycogen is hydrolysed ( broken down) into glucose |
|
|
|
Define gluconeogenesis |
The conversion of glycerol and amino acid into glucose |
|
|
|
What is adrenaline |
Adrenaline is a hormone Which is released by the adrenal glands when blood concerntration is low ( especially during exercise or in response to stress) |
|
|
|
Role of adrenaline |
It attaches to receptors on the surface of of specific target cell especially of the liver and muscles, and activates enzyme which hydrolyse glycogen into glucose ( glycogenolysis). |
|
|
|
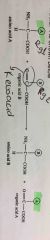
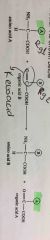
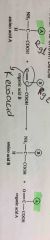
What are the fisrts messenger system and second messenger system |
First - adrenaline Second- cyclic AMP |
|
|
|
What is the role of glycogen phosphorylase |
An enzyme which is activated by second messenger system it’s the final enzyme that converts glycogen to glucose. In second messenger model of glucagon Adenyl cyclase atp to amp cyclic 2 pi Inactive protein kinase into active protein kinase this converts inactive phoplolyrase into active phosphorylase this converts glycogen into glucose |

|
|
|
What is active phosphorylase |
Its an enzyme that converts glycogen to glucose in second messenger model of adrenaline |

|
|
|
What is the roles of insulin and glucagon in the regulation of blood glucose |
Back (Definition) |
|
|
|
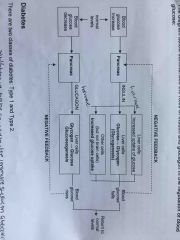
What is type 1 diabetes and how is it caused |
People with type one diabetes dose not produce insulin or very little. Cells in the pancreas’s which produces insulin (beta pancreas cells) are destroyed (its thought to be done by the immune system attacking the insulin producing beta cells) |
|
|
|
What is type 2 diabetes |
Usually Occurs in adulthood. Happens because cells have fewer insulin receptors, or the receptors are less sensitive in responding to insulin. So less glucose is taken in by cells from the blood to convert to glycogen and so the concerntration of glucose in blood remains high. |
|
|
|
What is the most significant risk factor of type 2 diabetes |
Long term obesity |
|
|
|
How can you manage type one and type two diabetes |
Type one - insulin dependant so needs insulin injections Type 2 - avoid food that causes rapid increase in blood glucose, instead consume complex carbohydrates such as starch which is digested slowly do that blood glucose dose not increase rapidly. |
T |
|
|
How can you diagnose diabetes |
-Glucose tolerance test is given -overnight fast -in hospital drink a solution contains 75g glucose - remain in rest movement would increase the rate of respiration which would consume glucose. - blood glucose can be tested using test strip with immobilised enzymes, the enzymes produce colour change proportional to glucose concerntration. Results read by colorimeter accurate reading - before strips were used to to determine the presence of glucose in the urine. But glucose only appears in urine once the patient has severe diabetes. |
|
|
|
Define hyperglycaemia and hypoglycaemia |
It’s for u to find out |
|
|
|
The body is unable to directly store absorbed amino acids, the amino acids which is not immediately required for protein synthesis or glucose formation (gluconeogenesis) may undergo ......... |
Transamination or deamination |
|
|
|
Explain transamination. |
- the amino group from one amino acid can be transferred to a Leto-acid to produce a new amino acid |
|
|
|
Explain transamination. |
- the amino group from one amino acid can be transferred to a Leto-acid to produce a new amino acid |
|
|
|
How do we produce amino acids that we are lacking in our diet |
Transamination |
|
|
|
Explain transamination. |
- the amino group from one amino acid can be transferred to a Leto-acid to produce a new amino acid |
|
|
|
How do we produce amino acids that we are lacking in our diet |
Transamination |
|
|
|
Define non essential and Essential amino acids |
Non essential- These are amino acids which are lacking in the diet Essential amino acids cannot be made from the body and so it has to come from our food |
|
|
|
Explain transamination. |
- the amino group from one amino acid can be transferred to a Leto-acid to produce a new amino acid |
|
|
|
How do we produce amino acids that we are lacking in our diet |
Transamination |
|
|
|
Define non essential and Essential amino acids |
Non essential- These are amino acids which are lacking in the diet Essential amino acids cannot be made from the body and so it has to come from our food |
|
|
|
What is deamination |
- Amino acids may be delaminates in the liver. This is the removal of the amino group (NH2) from the amino acid along with hydrogen to form ammonia (NH3) - a keto-acid is also produced, this can enter the respiratory pathway to release energy via glycolysis or Krebs cycle (depending on the initial amino acid) |

|
|
|
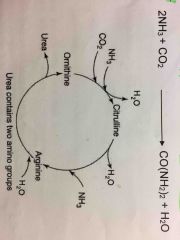
What is the ornithine cycle What is produced in this cycle and how’s its used |
-The ammonia produced from the deamination of amino acid is highly toxic. So in the ornithine cycle the ammonia combines with CO2 to form urea. - urea is transported in the blood from the liver to the kidneys where it’s excreted in urine. -the keto acid produced is either used in respiration or is converted to carbonhydrates and stored as glucagon in the liver. |
|
|
|
Why is it good that urea is soluble |
Check |
|
|
|
What happens to red blood cells when they have exceeded their 120 days life span |
Broken down by macrophages in the liver |
|
|
|
Describe heamoglobin metabolism |
1. The heamoglobin is released and broken down into heam and globin 2. Globin is broken down into amino acids 3. The iron is removed from the heam. The reamains of the heam group forms a pigment known as biliverdin. This is then converted to bilirubin which is a yellow component of bile (excreated in feaces) |
|
|
|
What is Bilirubin |
Yellow component of bile. Is produced by the conversion of the green pigment of heam group known as Biliverdin |
|
|
|
What dose the accumulation of bilirubin leads |
Bilirubin is a yellow component of of bile, it’s accumulation leads to jaundice (yellowing of the skin) this is an indication of liver disease. |
|
|
|
Describe fat metabolism |
1. The liver converts excess carbohydrates into fats 2. If glucose is in short supply the liver breaks down lipids into glycerol and fatty acids. The fatty acids can enter kerbs cycle and glycerol can be converted to into glucose. |
|
|
|
What is statins |
They are drugs that reduces cholesterol level in the body by slowing down the production of cholesterol by the liver. |
|
|
|
What is statins |
They are drugs that reduces cholesterol level in the body by slowing down the production of cholesterol by the liver. |
|
|
|
Role of the liver in terms of cholesterol |
The liver removes cholesterol from the blood / body by converting it to bile salt and eliminated as faeces. Cholesterol is a type of lipid which is synthesised by the liver ( to be exported to other cells) and the levels of cholesterol in the body is regulated by the liver too. |
|
|
|
What transports cholesterol and other lipids to other cells of the body |
Lipoproteins synthesised by the liver |
|
|
|
What is lipoproteins |
They are particles that contain triacylglycerol ( triglycerides) , cholesterol, phospholipids and proteins called apolipoprotiens Lipoproteins transports lipids and cholesterol around the body. |
|
|
|
What is apolipoprotiens |
They are proteins that bind lipids they are different for each lipid being carried |
|
|
|
What is apolipoprotiens |
They are proteins that bind lipids they are different for each lipid being carried |
|
|
|
How can lipoproteins be differentiated |
By there density and the type of apolipoproteins they contain. The lower the density of the lipoprotein the more lipid it contains compared to protein |
|
|
|
What is apolipoprotiens |
They are proteins that bind lipids they are different for each lipid being carried |
|
|
|
How can lipoproteins be differentiated |
By there density and the type of apolipoproteins they contain. The lower the density of the lipoprotein the more lipid it contains compared to protein |
|
|
|
What are the 4 major lipoproteins |
Chylomicrons Very low-density proteins (VLDL) Low density lipoprotein (LDL) High density lipoprotein (HDL) |
|
|
|
What is apolipoprotiens |
They are proteins that bind lipids they are different for each lipid being carried |
|
|
|
How can lipoproteins be differentiated |
By there density and the type of apolipoproteins they contain. The lower the density of the lipoprotein the more lipid it contains compared to protein |
|
|
|
What are the 4 major lipoproteins |
Chylomicrons Very low-density proteins (VLDL) Low density lipoprotein (LDL) High density lipoprotein (HDL) |
|
|
|
Where are chylomicrons synthesised, and what is there function |
1. Synthesised by the epithelial cells from lipids absorbed in the small intestine 2. Function- deliver energy rich triglycerides to cells + muscles in the body |
|
|
|
What is apolipoprotiens |
They are proteins that bind lipids they are different for each lipid being carried |
|
|
|
How can lipoproteins be differentiated |
By there density and the type of apolipoproteins they contain. The lower the density of the lipoprotein the more lipid it contains compared to protein |
|
|
|
What are the 4 major lipoproteins |
Chylomicrons Very low-density proteins (VLDL) Low density lipoprotein (LDL) High density lipoprotein (HDL) |
|
|
|
Where are chylomicrons synthesised, and what is there function |
1. Synthesised by the epithelial cells from lipids absorbed in the small intestine 2. Function- deliver energy rich triglycerides to cells + muscles in the body |
|
|
|
How is triglycerides removed from the chylomicrons |
By the action of lipoprotein lipase. An enzyme found on the surface of endothelial cells digests the triglycerides to fatty acids and monoglycerides which can then diffuse into the cell to be oxidised In the case of adipose cells to be resynthesized into triglycerides and stored in the cell |

|
|
|
Where is VLDL synthesised and what is it’s function |
Synthesised in the liver and has the same function as chylomicrons |
|
|
|
Where is VLDL synthesised and what is it’s function |
Synthesised in the liver and has the same function as chylomicrons |
|
|
|
Where is LDL synthesised and what is it’s Function |
Synthesised in the liver Function - delivers cholesterol to cells in the body |
|
|
|
Where is VLDL synthesised and what is it’s function |
Synthesised in the liver and has the same function as chylomicrons |
|
|
|
Where is LDL synthesised and what is it’s Function |
Synthesised in the liver Function - delivers cholesterol to cells in the body where it’s used in membranes or for synthesis of steroid hormones |
|
|
|
How is LDL made |
When the triglycerides of the VLDL is removed they become more dense. They are remodelled in the liver and transformed into LDL |
|
|
|
Why is LDL referred to as a bad cholesterol |
Forms plaque (thick hard deposit which can clog arteries and make them less flexible ) |
|
|
|
Where is HDL synthesised and What is it’s function. |
Synthesised and secreted by the liver and small intestine Function- reverse cholesterol transport. Excess cholesterol from cells are brought back to the liver by HDL by various pathways. Cholesterol is eliminated from the body by the liver. The liver might secrete cholesterol in bile or convert it to bile salt which is then removed from the body |
|
|
|
Why is HDL cholesterol considered a good cholesterol |
Because it helps remove excess LDL cholesterol’s from the body / clogged arteries |
|
|
|
What happens to the lipoproteins produced by the liver |

Back (Definition) |
|
|
|
Why is ethanol soluble both in aqueous and lipid Environment. And how is this a benefit |
Because ethanol’s small size and alcoholic hydroxyl group. This allows ethanol to freely pass from bodily fluids into cells |
|
|
|
Where is alcohol metabolised |
The invested ethanol from the gut is metabolised in the liver. |
|
|
|
What two enzymes are involved in the metabolism of ethanol and what is third roles |
Alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH) they apart the alcohol molecule. So ADH metabolises alcohol to acetaldehyde (highly toxic substance) this requires the reduction of NAD to form NADH + H. The acetaldehyde then enters the mitochondria, where it is oxidised to a less active by product called acetate. This also can be further broken down to CO2 and H2O for easy elimination |

|
|
|
What is the symptoms of alcohol related liver disease (ARLD) |
ARLD doesn’t usually cause any symptoms until the liver has been severely damaged when this happens you may feel sick, weight loss , yellow eyes and skin (jaundice), swelling in the ankle and tummy, vomiting blood or passing out blood in your stools |
|
|
|
What happens to the cells of the liver every time your liver filters alcohol |
Some liver cells die, but liver is capable of regenerating itself, prolonged use of alcohol may reduce the ability of the liver to regenerate itself this can cause serious and permanent damage to the liver. |
|
|
|
What is alcohol hepatitis |
Is a diseased inflammatory condition of the liver cause by consuming too much alcohol over a long time. This is because when alcohol is being processed by the liver it produces highly toxic chemicals which can injure liver cells, this can lead to inflammation and alcoholic hepatitis |
|
|
|
Alcoholic hepatitis dose not occur in all heavy drinkers it at even happens to moderate drinkers too so what other factors may influence the development of this condition(4) |
1. Genetic factors that affects how body processes alcohol 2. The presence of other liver disorders such as hepatitis C 3. Malnutrition 4. Drinking outside of meal times |
|
|
|
Are women twice as likely to get alcohol hepatitis And why |
Yeas maybe because of the differences in how the body of men and women absorbs and breakdown alcohol |
|
|
|
What is cirrhosis? |
Cirrhosis is the scarring of the liver caused by continuous long term liver damage. Liver can’t work properly as the healthy tissues are replaced by the scar tissues. This damage cannot be reversed, the liver cannot regenerate itself. It can become so intensive that your liver stops functioning. It takes long time for the process to reach this stage and treatment can help slow it down |
|
|
|
What is cirrhosis? |
Cirrhosis is the scarring of the liver caused by continuous long term liver damage. Liver can’t work properly as the healthy tissues are replaced by the scar tissues. This damage cannot be reversed, the liver cannot regenerate itself. It can become so intensive that your liver stops functioning. It takes long time for the process to reach this stage and treatment can help slow it down |
|
|
|
What are the common causes of cirrhosis (3) |
1. Drinking too much alcohol over a long period of time 2. Being infected with hepatitis C virus for a long time 3. A condition known as non-alcoholic steatohepatitis (NASH) that causes excess fat to build up in the liver. |
|
|
|
What are the less common cause of cirrhosis |
Hepatitis B infection and inherited liver disease such as heamochromatosis |
|
|
|
Where dose drug metabolism occur(4) |
Most occur in the liver, some in the gut wall, lungs and blood plasma |
|
|
|
Where dose drug metabolism occur |
Most occur in the liver, some in the gut wall, lungs and blood plasma |
|
|
|
Why All Metabolic processes will convert the drug into a more water soluble compound by increasing its polarity. |
So that the drug can be excreted in the body fluids such as urine or bile (body fluids) only a few drugs can be excreted without being metabolised first |
|
|
|
Where dose drug metabolism occur |
Most occur in the liver, some in the gut wall, lungs and blood plasma |
|
|
|
Why All Metabolic processes will convert the drug into a more water soluble compound by increasing its polarity. |
So that the drug can be excreted in the body fluids such as urine or bile (body fluids) only a few drugs can be excreted without being metabolised first |
|
|
|
What happens to the therapeutic effect of drug when it’s metabolised |
It diminishes it has no affect no more |
|
|
|
How are drugs oxidised What enzyme catalyses oxidation What happens when the drug is catalysed |
Oxidation is catalysed by cytochrome p450 enzyme, this results in the drug loosing an electron, loosing an electron makes the drug more reactive |
|
|
|
Why dose some drugs goes through phase 1 and not phase 2 or undergoes just phase 2 or goes through both phases |
If the metabolites/ drug of phase 1 is water soluble enough they can be excreted at this point if not they go through phase 2 as well. Some drugs directly go though phase two and then excreted |
|
|
|
How are drugs oxidised What enzyme catalyses oxidation What happens when the drug is catalysed |
Oxidation is catalysed by cytochrome p450 enzyme, this results in the drug loosing an electron, loosing an electron makes the drug more reactive |
|
|
|
Why dose some drugs goes through phase 1 and not phase 2 or undergoes just phase 2 or goes through both phases |
If the metabolites/ drug of phase 1 is water soluble enough they can be excreted at this point if not they go through phase 2 as well. Some drugs directly go though phase two and then excreted |
|
|
|
phase 2 of drug metabolism involves conjugation what is conjunction. |
Conjunction is the attachment of an ionised group such as ( glutathione, methyl or acetyl groups) to the drug. The attachment of an ionised group makes the metabolite more water soluble. There for the drug can be excreted and it’s pharmacological activity decreases too. |
|
|
|
phase 1 and phase 2 of drug metabolism occur in which cytoplasm and where |
In the hepatocyte cytoplasm in the liver |
|
|
|
How are drugs oxidised What enzyme catalyses oxidation What happens when the drug is catalysed |
Oxidation is catalysed by cytochrome p450 enzyme, this results in the drug loosing an electron, loosing an electron makes the drug more reactive |
|
|
|
Why dose some drugs goes through phase 1 and not phase 2 or undergoes just phase 2 or goes through both phases |
If the metabolites/ drug of phase 1 is water soluble enough they can be excreted at this point if not they go through phase 2 as well. Some drugs directly go though phase two and then excreted |

|
|
|
phase 2 of drug metabolism involves conjugation what is conjunction. |
Conjunction is the attachment of an ionised group such as ( glutathione, methyl or acetyl groups) to the drug. The attachment of an ionised group makes the metabolite more water soluble. There for the drug can be excreted and it’s pharmacological activity decreases too. |
|
|
|
phase 1 and phase 2 of drug metabolism occur in which cytoplasm and where |
In the hepatocyte cytoplasm in the liver |
|
|
|
in which stage 1 or 2 of drug metabolism is the drug metabolite still active |
In Phase 1 the drug metabolite is still chemically active as it has lost and electron, but phase 2 the drug metabolites is decreased in pharmacological activity. |
|
|
|
explain the drug metabolism of aspirin. |
Aspirin is a drug that is metabolised by the liver, aspirin goes through phase 1 hydrolysis to salicylic acid. In phase 2 it is conjugated with either glycine or glucuronic acid forming a range of ionised metabolites that can be excreted in urine |
|
|
|
what is a free radical |
Free radical is an atom or group of atoms that has an unpaired electrons and is therefore unstable and highly reactive |
|
|
|
how is the chemical behaviour of an atom determined |
The chemical behaviour of an atom is determined by the number of electrons in its outer most shell. Full outer shell electrons the atom dose not engage in chemical reactions. And when it’s not full it is unstable. It will either stable it self by gaining or loosing electrons, to fill or empty its outer most shell. Or the atom would share its electrons by bonding with another atom that is also looking to complete its outer shell |
|
|
|
how are free radicals formed |
They form when one of the week bonds between electrons are broken, and there is an uneven number of electrons present, this means electron is unpaired making it chemically reactive, now it will try to gain an electron by stealing from neighbouring molecule to stabilise itself |
|
|
|
explain free radical cascade and how it’s caused |
Free radical cascade is a large chain reaction of free radicals that damages living tissues very fast. It’s caused by unstable atoms stealing electrons to make them selfs stable. Leaving it’s victim free radical and the process carries on by the unstable victim picking up an electron from another atom making them a free radical and itself stable and so on. And that results in free radical cascade. |
|
|
|
what ways and what processes can result in the formation of free radicals. (3) |
Normally during metabolism External Exposures to x rays, cigarette smoke or pollutants The immune system creates them to neutralise virus and bacteria |
|
|
|
what are the affects of free radicals. |
Free radicals can attack molecules such as fats, DNA, RNA, cellular membranes, proteins vitamins and carbohydrates. But especially oxygen and with aerobic organisms this can be very lethal. Oxygen free radicals are involved in the overall ageing process. |
|
|
|
what is oxygen free radical responsible for(3)
|
They are responsible for ageing, cancer and inflammation in the skin. |
|
|
|
What are antioxidants and what is there role |
Antioxidants are molecules which interact with free radicals and neutralizes them by donating one of there own electrons. And ending the electron stealing reaction. |

|
|
|
why does antioxidant nutrients themselves become free radicals |
Because they are stable in either form, they help prevent cell and tissue damage that could lead to cellular damage and disease |
|
|
|
name three micronutrients (vitamin)antioxidants |
Vitamin E - most abundant fat soluble antioxidant in the body present in nuts seeds vegetables and fish oils Vitamin C - most abundant water soluble antioxidant in the body they are present in citrus fruits and green vegetables. It combats free radicals caused by cigarettes smoke and pollution Beta - carotene - eg vitamin A (retinol) present in liver, dairy products and fruits and vegetables.
The body cannot make these micronutrients they must be supplied in the diet. |
|
|
|
name three micronutrients (vitamin)antioxidants |
Vitamin E - most abundant fat soluble antioxidant in the body present in nuts seeds vegetables and fish oils Vitamin C - most abundant water soluble antioxidant in the body they are present in citrus fruits and green vegetables. It combats free radicals caused by cigarettes smoke and pollution Beta - carotene - eg vitamin A (retinol) present in liver, dairy products and fruits and vegetables.
The body cannot make these micronutrients they must be supplied in the diet. |
|
|
|
Give examples of diseases which antioxidants could prevent and why (3) |
Heart disease - vitamin E protects against cardiovascular diseases by defending against LDL oxidation and artery-clogging plaque formation Cancer - there is a high correlation between the intake of vitamin C and low cancer especially the cancers of the mouth, oesophagus and larynx. Age related eye disease - intake of vitamin C E and beta carotene and zinc offers protection against the development of advanced age related macular degeneration in people who were in high risk of developing them. |
|

