![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
273 Cards in this Set
- Front
- Back
|
Steatosis
|
- In cellular pathology, steatosis (also called fatty change, fatty degeneration or adipose degeneration) is the process describing the abnormal retention of lipids within a cell.
- It reflects an impairment of the normal processes of synthesis and elimination of triglyceride fat. - Excess lipid accumulates in vesicles that displace the cytoplasm. |
|
|
necessary components to pump the heart
|
- Blood vessels (arteries and veins)
- Muscle (myocardium) - Cardiac valves - Conduction system |
|
|
blood flow of the heart
|
- De-oxygenated blood flows from the superior and inferior vena cavae into the right atrium
- Through the tricuspid valve into the right ventricle - Through the pulmonic valve into the pulmonary arteries and lungs (exchange of gases) - Through the pulmonary veins – returning oxygenated blood into the left atrium - Through the mitral valve into the left ventricle - Out through the aortic valve into aorta to be distributed to the body |
|
|
Why is the left ventricle thicker than the right ventricle?
|
Form follows function. Why?
- RV pumps blood to the lungs. LV pumps blood to the entire body. - LV AND THE AORTA ARE THICK WALLED. |
|
|
components of the heart's conduction system
|
- SA node (pacemaker), junction of the right atrial appendage and the superior vena cava
- AV node, at the right atrium along the atrial septum - Bundle of His and the right and left bundle branches |
|
|
The conductor of the rate and rhythm is the _____
|
SA node (pace maker)
|
|
|
Systole
|
contraction (the ventricular muscle contracts during systole)
|
|
|
Diastole
|
(the ventricular muscle relaxes during diastole)
|
|
|
pericardium
|
Parietal pericardium
- Fibrous tissue (collagen) Pericardial sac - Potential space - Fluid - completely surrounds the heart and is composed of fibrous connective tissue and acts as a protective membrane Visceral pericardium – Lines the epicardium - Single layer of mesothelium |
|
|
Why do you need elastic tissue in the pericardial sac?
|
Because it acts as a pump, that has to be able to expand and contact protects the heart, and holds it in place within the thorax
|
|
|
Hemopericardium
|
blood in the pericardial sac – is a pathologic state – abnormal - (MI with myocardial rupture)
- If you look at this in a radiograph you see a huge heart and makes you think is cardiomegaly , but is really blood covering the heart. - you also see hemopericardium if you have a rupture of the ascending part of the aorta , or rupture of the coronary artery and all the blood escapes into the pericardial sac. |
|
|
Pericarditis
|
an inflammation of the pericardial sac
It can be a uremic pericaritis due to kidney failure , or an infectious pericarditis |
|
|
Chronic epicarditis
|
- Adipose tissue normally covers the epicardial surface of the heart
- the epicardial surface of the heart is no longer smooth - There Is a purulent exudate, and fibrinous adhesion- this tells you this is pathologic - most common causes of chronic epicarditis – infectious(bacterial), chemical (uremia) or tumor metastasis (rare) |
|
|
Myocardium
|
- made up of specialized striated muscle fibers
- They are specialized bc they branch, (unlike smooth muscle) - Cardiac muscle branches bc the myofibrils have to stretch all the way around the heart - striated muscle (myofibrils) make up most of the volume because they are large fibers - myocardium also have endothelial cells (within)- they invest all of the valves , papillary muscles, atrial chambers, ventricular chambers |
|
|
5 components of myocytes
|
5 components of myocytes
Sarcolemma (cell membrane) conduction - Sarcoplasmic reticulum Reservoir for electrolytes - Sarcomere Contractile elements (actin, myosin) - Regulatory proteins (Troponin, tropomyosin) Mitochondria - Aerobic metabolism Nucleus - Single, spindle shaped |
|
|
Sarcolemma
|
5 components of myocytes
Sarcolemma (cell membrane) conduction - Sarcoplasmic reticulum Reservoir for electrolytes - Sarcomere Contractile elements (actin, myosin) - Regulatory proteins (Troponin, tropomyosin) Mitochondria - Aerobic metabolism Nucleus - Single, spindle shaped |
|
|
sarcoplasmic reticulum
|
5 components of myocytes
Sarcolemma (cell membrane) conduction - Sarcoplasmic reticulum Reservoir for electrolytes - Sarcomere Contractile elements (actin, myosin) - Regulatory proteins (Troponin, tropomyosin) Mitochondria - Aerobic metabolism Nucleus - Single, spindle shaped |
|
|
sarcomere
|
5 components of myocytes
Sarcolemma (cell membrane) conduction - Sarcoplasmic reticulum Reservoir for electrolytes - Sarcomere Contractile elements (actin, myosin) - Regulatory proteins (Troponin, tropomyosin) Mitochondria - Aerobic metabolism Nucleus - Single, spindle shaped |
|
|
mitochondria
|
5 components of myocytes
Sarcolemma (cell membrane) conduction - Sarcoplasmic reticulum Reservoir for electrolytes - Sarcomere Contractile elements (actin, myosin) - Regulatory proteins (Troponin, tropomyosin) Mitochondria - Aerobic metabolism Nucleus - Single, spindle shaped |
|
|
nucleus of myocyte
|
5 components of myocytes
Sarcolemma (cell membrane) conduction - Sarcoplasmic reticulum Reservoir for electrolytes - Sarcomere Contractile elements (actin, myosin) - Regulatory proteins (Troponin, tropomyosin) Mitochondria - Aerobic metabolism Nucleus - Single, spindle shaped |
|
|
average size of left ventricle
|
Left ventricle – 1.3 to 1.5 cm
Right ventricle – 0.3 to 0.5 cm *the left ventricle has to be thicker than the right ventricle bc you have to pump the blood up through the aorta. So there are higher pressures on the left side of the heart |
|
|
average size of right ventricle
|
Left ventricle – 1.3 to 1.5 cm
Right ventricle – 0.3 to 0.5 cm *the left ventricle has to be thicker than the right ventricle bc you have to pump the blood up through the aorta. So there are higher pressures on the left side of the heart |
|
|
Cardiomegaly
|
Cardiomegaly (enlarged heart):
- Hypertrophy – same number of cells, just larger - Dilation – enlarged chamber size --> In response, will release Atrial Natriuretic Peptide |
|
|
endocardium
|
- Innermost lining of heart chambers, valves, chordae tendineae, papillary muscles and trabeculae carneae
- Endothelium - Connective tissue - Smooth muscle Termination of conduction system |
|
|
Endothelial lining of the endocardium
|
a single layer of squamous epithelium , Fibrous connective tissue, is were you have small capillaries and BV
Capillaries and BV’s protect the innermost myocardium, and supply blood and nutrients Endocardial layer is critically important |
|
|
Atrio-Ventricular valves
|
- Tricuspid and mitral
- Leaflets, chordae tendinae, papillary muscles, myocardium |
|
|
Semilunar valves
|
- Pulmonic and Aortic
- Cusps |
|
|
coronary arteries
|
- 2 to 4 mm in diameter
- Supply nutrients to the heart - Arise from the ascending portion of the aorta --> Sinus of Valsalva - Course along the epicardial surface and send branches to nearly every myocyte - Flow during diastole - Collaterals |
|
|
What happens when the atherosclorotic plaque become very big and cover the coronary ostia?
|
prevents blood flow into the coronary arteries and that leads to myocardial infarcts
|
|
|
different coronary arteries
|
Left Main (left anterior descending and left circumflex):
Left Anterior Descending: - Diagonals - Supplies the apex, anterior LV wall, anterior 2/3 septum Left Circumflex: - Obtuse marginals - Lateral Left Ventricle Right Coronary Artery: - Right Ventricle, posterior 2/3 of septum (post descending) and posterior basal Left Ventricle |
|
|
left main coronary artery branches into....
|
Left Main (left anterior descending and left circumflex):
Left Anterior Descending: - Diagonals - Supplies the apex, anterior LV wall, anterior 2/3 septum Left Circumflex: - Obtuse marginals - Lateral Left Ventricle Right Coronary Artery: - Right Ventricle, posterior 2/3 of septum (post descending) and posterior basal Left Ventricle |
|
|
LAD supplies...
|
Left Main (left anterior descending and left circumflex):
Left Anterior Descending: - Diagonals - Supplies the apex, anterior LV wall, anterior 2/3 septum Left Circumflex: - Obtuse marginals - Lateral Left Ventricle Right Coronary Artery: - Right Ventricle, posterior 2/3 of septum (post descending) and posterior basal Left Ventricle |
|
|
Right Coronary Artery supplies...
|
Left Main (left anterior descending and left circumflex):
Left Anterior Descending: - Diagonals - Supplies the apex, anterior LV wall, anterior 2/3 septum Left Circumflex: - Obtuse marginals - Lateral Left Ventricle Right Coronary Artery: - Right Ventricle, posterior 2/3 of septum (post descending) and posterior basal Left Ventricle |
|
|
left circumflex artery supplies....
|
Left Main (left anterior descending and left circumflex):
Left Anterior Descending: - Diagonals - Supplies the apex, anterior LV wall, anterior 2/3 septum Left Circumflex: - Obtuse marginals - Lateral Left Ventricle Right Coronary Artery: - Right Ventricle, posterior 2/3 of septum (post descending) and posterior basal Left Ventricle |
|
|
bloodflow of the lungs
|
Deoxygenated blood from right side of heart (return from body) flows to lungs where exchange of CO2 for O2 occurs.
Oxygenated blood then leaves via pulmonary veins to the left side of the heart to be sent to the body. |
|
|
in the lungs... gaseous exchange occurs within
|
alveolar septae
--> Alveolar septa- are very thin wall capillaries that allow for exchange of gas O2 and CO2 |
|
|
Alveolar septa
|
are very thin wall capillaries that allow for exchange of gas O2 and CO2
Gaseous exchange occurs within the alveolar septae |
|
|
normal aging of the heart chambers
|
Chambers:
- Increased left atrial cavity size, Decreased left ventricular cavity size, Sigmoid-shaped ventricular septum Valves: - Aortic valve calcific deposits, Mitral valve annular calcific deposits, Fibrous thickening of leaflets, Buckling of mitral leaflets toward the left atrium, Lambl excrescences |
|
|
normal aging of the heart valves
|
Chambers:
- Increased left atrial cavity size, Decreased left ventricular cavity size, Sigmoid-shaped ventricular septum Valves: - Aortic valve calcific deposits, Mitral valve annular calcific deposits, Fibrous thickening of leaflets, Buckling of mitral leaflets toward the left atrium, Lambl excrescences |
|
|
normal aging of the epicardial coronary arteries
|
Epicardial Coronary Arteries
- Tortuosity, Increased cross-sectional luminal area, Calcific deposits, Atherosclerotic plaque Myocardium: - Increased mass, Increased subepicardial fat, Brown atrophy, Lipofuscin deposition, Basophilic degeneration, Amyloid deposits |
|
|
normal aging of the myocardium of the heart
|
Epicardial Coronary Arteries
- Tortuosity, Increased cross-sectional luminal area, Calcific deposits, Atherosclerotic plaque Myocardium: - Increased mass, Increased subepicardial fat, Brown atrophy, Lipofuscin deposition, Basophilic degeneration, Amyloid deposits |
|
|
normal aging of the aorta
|
Aorta:
- Dilated ascending aorta with rightward shift (due to a loss of elastic fibers and atheroscleorotic plaque ) - Elongated (tortuous) thoracic aorta - Sinotubular junction calcific deposits - Elastic fragmentation and collagen accumulation - Atherosclerotic plaque |
|
|
Dilated ascending aorta
|
due to a loss of elastic fibers and atheroscleorotic plaque
|
|
|
cause of heart failure
|
Systolic
- 65% - Poor pump Diastolic - 35% - Poor filling |
|
|
majority of heart failure is (systolic / diastolic)
|
Systolic
- 65% - Poor pump Diastolic - 35% - Poor filling |
|
|
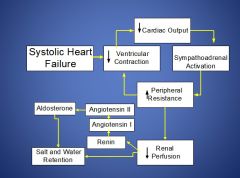
systolic heart failure
|
Compensatory mechanisms:
- Increased end diastolic filling pressure - Increased end diastolic volume - Neurohumoral Frank Starling Law - Increased volume leads to increased cardiac output - Greater overlap of sarcomere filaments thus increased force - Eventually, the length of the sarcomere length will become too long and the actin-myosin bridges will not overlap - The higher end pressure will cause backup of blood into the pulmonary circulation |
|
|
Neurohumoral Response to Heart Failure
|
|
|
|
left vs. right-sided heart failure
|
Left sided:
- More common - Systemic disease - Respiratory difficulties Right sided: - Less common - Secondary to left sided failure, pulmonary disease |
|
|
which is more common... L or R sided heart failure?
|
Left sided:
- More common - Systemic disease - Respiratory difficulties Right sided: - Less common - Secondary to left sided failure, pulmonary disease |
|
|
etiology of heart failure
|
- Hypertension
- Atherosclerosis / Myocardial infarct(s) - Valvular disease - Inflammatory disease - Tumors |
|
|
on a dead body... if you see a blue green bruise.. what does that signify?
|
tells you something is dead under the skin
|
|
|
if you see pitting edema during an autopsy...
|
Pitting edema tells us there was a heart problem
|
|
|
Most common cause of mitral valve stenosis is _____
|
rheumatic heart disease
--> causes sclerosis , and narrowing of your mitral valves --- fish mouth appearance - so the blood is having a hard time getting through that mitral valve- mitral valve is no longer pliable |
|
|
Left atrial fibrosis
|
Left atrial fibrosis c/w regurgitation
Left atrial fibrosis with regurgitation (backflow of blood)- through a stenotic mitral valve from rheumatic heart disease You may hear a heart murmur (turbulent flow) due to the flow through the stenotic valve Tx for this will be valve replacement |
|
|
What happens when you have endocarditis affecting the chordae tendinae, and you have ruptured of one of those cherdae tendinae ?
|
Then you have an incompetent valve that wont open or close properly , having regurgitant flow
|
|
|
Damage of the AV valves can lead to...
|
Stenosis
Regurgitation Mixture of both |
|
|
stenosis
|
- Does not open fully
- Impedes forward flow - Blood and pressure back up Can be either: - Acquired aortic and mitral (2/3 of all valvular disease) - Primary chronic cuspal abnormalities |
|
|
regurgitation
|
- Does not close completely
- Backflow of blood Can be from: Dilation of ventricle (affecting papillary muscle) Dilation of aorta or pulmonary artery (affecting commisures) Damage to cusps or supporting structures (chordae tendinae) |
|
|
most common valve diseases
|
Aortic stenosis: calcification of anatomically normal and congenitally bicuspid aortic valves
Aortic insufficiency: dilation of the ascending aorta, related to hypertension and aging. Mitral stenosis: rheumatic heart disease (99%) Mitral insufficiency: myxomatous degeneration (mitral valve prolapse) |
|
|
Aortic stenosis
|
calcification of anatomically normal and congenitally bicuspid aortic valves
--> mainly an aging problem |
|
|
Aortic insufficiency
|
dilation of the ascending aorta, related to hypertension and aging
|
|
|
Mitral stenosis
|
rheumatic heart disease (99%)
|
|
|
Mitral insufficiency
|
myxomatous degeneration (mitral valve prolapse)
--> Myxomatous- softening of the leaflets of mitral valves – is soft bc is a mix of mucous and loose collagenous tissue This occurs in young females (she mentioned a 30 y/o) |
|
|
what is THE most common valvular disease ?
|
CALCIFIC AORTIC STENOSIS
- Most common valvular disease - Repetitive mechanical stress - Calcification of damaged valve from wear and tear - Dystrophic deposits of calcium phosphate |
|
|
Calcific Aortic Stenosis
|
- Most common valvular disease
- Repetitive mechanical stress - Calcification of damaged valve from wear and tear - Dystrophic deposits of calcium phosphate |
|
|
Tx for rheumatic heart disease or aortic stenosis from normal aging is __________
|
valve replacement
|
|
|
**bicuspid aortic valve
|
- found in only ~1% of the population
- Instead of having three nice cusps they only have 2 - Eventually the valve will become stenotic and fibrotic bc of the undo stress and increase pressure on the valve - Predisposed to calcification – any valve that is damaged and under a lot of stress |
|
|
calcific aortic stenosis
|
- Heaped up calcifications
- Within the cusps, free edge usually uninvolved - Commisures not fused (as opposed to rheumatic disease) - Protrude into sinuses of Valsalva thus preventing complete opening |
|
|
difference between calcific aortic stenosis & rheumatic disease
|
- in calcific aortic stenosis, Commisures not fused (as opposed to rheumatic disease)
|
|
|
aortic regurgitation
|
Intrinsic Valvular Disease
- Postinflammatory scarring (rheumatic heart disease) - Infective endocarditis Aortic Disease - Degenerative and hypertensive aortic dilation - Syphilitic aortitis - Ankylosing spondylitis - Rheumatoid arthritis - Marfan syndrome |
|
|
aortic regurgitation
|
- Left ventricle hypertrophies and dilates to accommodate the regurgitant volume and provide adequate cardiac output
- Often asymptomatic, and if normal LV function these patients get medical treatment (BP lowering) - Symptomatic patients require surgery. Pts with subnormal EF and symptoms <1 yr do very well |
|
|
mitral stenosis
|
postinflammatory scarring
--> rheumatic heart disease |
|
|
Clinical symptoms : of mitral stenosis
|
- Dyspnea on exertion: sitting on a chair and they cant breath
- Orthopnea- trouble breathing - Atrial fibrillation– an irregular heart beat - Pumonary hypertension- pressure on the right side of the heart are increasing - Cor pulmonale- heart and lung condition - lungs are being affected that’s why you are having trouble breathing |
|
|
Angina
|
narrowing of the coronary arteries due to the decrease in blood flow through the coronary arteries , causing myocardial ischemia, and infarction
Angina NOT involved with mitral stenosis |
|
|
**rheumatic fever
|
- affects young people (5-15 y/o) with pharyngitis
- Follows β-hemolytic Strep group A pyogenes pharyngitis (2 - 3 weeks) Anti-streptolysin O antibodies in serum - Immune mediated (Ab against M protein) - Fibrinoid necrosis along chorda tendinae and lines of closure of valves - May lead to chronic rheumatic heart disease |
|
|
major symptoms of rheumatic fever
|
Major:
- Migratory polyarthritis (inflammation of the big joints) - Pancarditis --> “Bread and butter” pericarditis -- the exudate of the pericardial surface of the heart - Subcutaneous nodules - Eryhtema marginatum - Syndenham chorea Minor: - Fever, elevated ESR or C reactive protein, EKG changes |
|
|
minor symptoms of rheumatic fever
|
Major:
- Migratory polyarthritis (inflammation of the big joints) - Pancarditis --> “Bread and butter” pericarditis -- the exudate of the pericardial surface of the heart - Subcutaneous nodules - Eryhtema marginatum - Syndenham chorea Minor: - Fever, elevated ESR or C reactive protein, EKG changes |
|
|
Aschoff body
|
During acute RF, focal inflammatory lesions are found in various tissues. Distinctive lesions occur in the heart, called Aschoff bodies, which consist of foci of lymphocytes (primarily T cells), occasional plasma cells, and plump activated macrophages called Anitschkow cells (pathognomonic for RF).
- they can involve the endocardium, myocardium, and paricardium |
|
|
rheumatic mitral stenosis
|
- Chronic stage of RHD
- Thick fibrotic valvular disease with organization (neo-vascularization) of acute inflammation - Fusion of commisures “Fishmouth” - Short, thick chorda tendinae - Affects- Mitral (65 – 70%), Mitral + Aortic (25%) - Nearly eradicated in industrialized world |
|
|
Mitral annulus
|
The mitral annulus is a ring that is attached to the mitral valve leaflets. Unlike prosthetic valves, it is neither circular nor continuous. The annulus contracts and reduces its surface area during systole to help provide complete closure of the leaflets. Annular dilatation can result in poor leaflet apposition, leading to mitral regurgitation.
|
|
|
Mitral Regurgitation
|
Mitral leaflets
- Rheumatic heart disease with retraction - Mitral valve prolapse Mitral annulus - Dilation of annulus because of ventricular enlargement from CHF - Mitral annulus calcification Infarct of Papillary muscle |
|
|
mitral valve prolapse
|
- 3% of adults (young women)
- “Floppy valve” - Mostly incidental finding - Midsystolic click (most times you dont hear this) - Echocardiography - Rubbery, redundant leaflets - Long, thin chorda tendinae - Prone to rupture with flail valve - Dilated annulus - Myxomatous degeneration (diffuse softening of the leaflets ) - Fibrosa – attenuated - Spongiosa – thick (myxoid) |
|
|
complications of mitral valve prolapse
|
- Thick leaflets
- Endocardial fibrosis atrium and ventricle - Atrial surface thrombi - Calcification - Infective endocarditis - Systemic infarcts - Arrhythmias |
|
|
artificial valve complications
|
- 60% within 10 years
- Thrombo-embolism: - Mechanical valves - On anticoagulants (complications themselves) - Heart valve replacement complication might be that can cause blood clots so pts might be in anticoagulant medications Can deteriorate overtime – specially seen in cadaver replaced valves |
|
|
common artificial valve complication
|
infective endocarditis
- Most common in first 5 to 6 weeks - Prosthesis-tissue interface or cusps - Ring abscess - Staph epidermidis, Staph aureus, strep, fungi - Surgery may be needed |
|
|
infective endocarditis
|
- Most common in first 5 to 6 weeks
- Prosthesis-tissue interface or cusps - Ring abscess - Staph epidermidis, Staph aureus, strep, fungi - Surgery may be needed |
|
|
non-bacterial thrombotic endocarditis
|
- Fibrin, platelets and other blood products
- No infectious organisms - Not invasive or destructive - Associated with chronic illnesses |
|
|
infective endocarditis
|
Entry of bacteria into bloodstream
-Invasive (dental, surgical) procedures -Intravenous drug abuse Colonization of endocardium (valves) Superimposed on early thrombus (platelets and fibrin) -Sites of damage to endothelium of endocardium |
|
|
*acute vs. subacute infective endocarditis
|
Acute:
-Fever Normal valves -Chills Rapid course -Weakness Highly virulent organisms Staph aureus, Strep pyogenes Subacute: -Fatigue Abnormal valves -Loss of weight Protracted course -Flu-like symptoms Low virulence organisms Strep viridans, Staph epiderm |
|
|
*acute infective endocarditis
|
Acute:
-Fever Normal valves -Chills Rapid course -Weakness Highly virulent organisms Staph aureus, Strep pyogenes Subacute: -Fatigue Abnormal valves -Loss of weight Protracted course -Flu-like symptoms Low virulence organisms Strep viridans, Staph epiderm |
|
|
*subacute infective endocarditis
|
Acute:
-Fever Normal valves -Chills Rapid course -Weakness Highly virulent organisms Staph aureus, Strep pyogenes Subacute: -Fatigue Abnormal valves -Loss of weight Protracted course -Flu-like symptoms Low virulence organisms Strep viridans, Staph epiderm |
|
|
predisposing factors to infective endocarditis
|
- Rheumatic heart disease
- Mitral Valve Prolapse - Calcific stenosis - Congenital heart disease (bicuspid aortic valve) - Prosthetic valves - DM, malignancy, IVDA, immunosuppression |
|
|
infective endocarditis
|
Deformed or damaged valves:
--Strep Viridans (Oral bleeding) Normal or deformed: --Staph aureus (IVDA) Prosthetic valves: --Staph epidermidis Enterococcus HACEK (Haemophilus, Actinobacillus, Cardiobacterium, Eikinella, Kingella) |
|
|
HACEK
|
(Haemophilus, Actinobacillus, Cardiobacterium, Eikinella, Kingella)
|
|
|
complications of infective endocarditis
|
Systemic emboli (ischemic lesions)
Glomerulonephritis |
|
|
you would give anti-coagulation therapy to people who:
|
Foreign material:
- coronary artery stents - valve replacements Prone to form blood clots: - Atrial fibrillation/ Left ventricle dysfunction - Coagulation defects - Deep vein thrombosis - Individuals that don’t move a lot, confined to wheel chairs , dehydrated, diabetics, atrial fibrillation, coagulation defects, DVT, obesity are all prone to form blood clots - Obese people- die because of blood clots in their legs due to bad circulation traveling to the lungs |
|
|
Different Anticoagulant Medications
|
- Different medications effect different parts of the coagulation cascade
- They require different laboratory tests - They all effect the ability of the body to form blood clots - They all carry a risk of bleeding especially when the level is high - Any patient on anticoagulants needs to have proper levels before undergoing a procedure that can cause significant bleeding (dental, surgical, hip replacements etc.) |
|
|
Heparin
|
- Acts by enhancing the activity of antithrombin, a natural anticoagulant made by the body
- Overdose of heparin can be treated with Protamine - The test for Heparin is the Partial Thromboplastin Time (PTT) - Therapeutic levels are about 1.5 times the mean of the normal baseline - Effect is immediate |
|
|
Overdose of heparin can be treated with _____
|
Protamine
|
|
|
heparin acts by...
|
Acts by enhancing the activity of antithrombin, a natural anticoagulant made by the body
|
|
|
The test for Heparin is the ______
|
Partial Thromboplastin Time (PTT)
|
|
|
Warfarin (Coumadin)
|
- Acts by inhibiting Vitamin K
- Overdose of Warfarin can be treated by giving Vitamin K - The test for Warfarin is the Prothrombin Time (PT) - More typically Warfarin is monitored by the International Normalized Ratio (INR) - The usual therapeutic goal is an INR of 2-3 International sensitivity index (ISI) - It takes about 4-5 days for the anticoagulant affect of Warfarin to take effect - Warfarin is for long term management |
|
|
warfarin acts by inhibiting
|
vitamin K
|
|
|
Overdose of Warfarin can be treated by giving _____
|
Vitamin K
|
|
|
which is immedate ad long term use.. warfarin vs heparin
|
Warfarin is for long term management
Effect of heparin is immediate |
|
|
Acts by enhancing the activity of antithrombin, a natural anticoagulant made by the body
|
heparin
|
|
|
Overdose of _____ can be treated with Protamine
|
heparin
|
|
|
Acts by inhibiting Vitamin K
|
warfarin (coumadin)
|
|
|
Overdose of _____can be treated by giving Vitamin K
|
Warfarin
|
|
|
Aspirin (salicylate)
|
blocks prostaglandin formation by inhibiting cyclooxygenase (COX)
In clotting, COX activates thromboxane A-2, (prevents platelets from sticking together) Aspirin is frequently available in combination with other medications such as antacids, pain relievers, and cough and cold medications. |
|
|
** What does aspirin (salicylate) do?
|
blocks prostaglandin formation by inhibiting cyclooxygenase (COX)
In clotting, COX activates thromboxane A-2, (prevents platelets from sticking together) |
|
|
blocks prostaglandin formation by inhibiting cyclooxygenase (COX)
|
Aspirin (salicylate)
|
|
|
Heart Murmurs
|
The sound generated by the turbulent flow of blood
Results from one of the following mechanisms: - Flow across a partial obstruction (aortic valve stenosis) - Ejection into a dilated chamber (aortic systolic murmur associated with an aortic aneurysm) - Regurgitant flow across an incompetent valve (mitral valve regurgitation) - Shunting of blood from a high to low pressure chamber through an abnormal passage (Ventricular Septal Defect) |
|
|
Murmurs are described by their:
|
- Timing (systole, diastole or continuous)
- Intensity (Systolic murmur 1-6/6 and diastolic murmur 1-4/4) - Location (Point where maximal intensity is heard on the body) - Shape (Crescendo, decrescendo, diamond shaped or pansystolic) - Radiation and maneuvers |
|
|
A heart murmur is an indication of:
|
- underlying valvular (mitral or aortic) disease
- congenital heart abnormality |
|
|
Ventricular Assist Devices (VADs)
|
- VADs improve the length and quality of life but at the expense of an increased incidence of inappropriate shocks, strokes, bleeding, and infection/sepsis.
- VADs are for patients who are not candidates for a heart transplant (destination therapy) or to bridge patients until a heart becomes available. - Even without the unintended consequences, these therapies can extend patients’ lives to the point of developing other diseases, e.g., dementia or cancer. |
|
|
one of the major complications of VAD
|
strokes
|
|
|
Ethical Principles
|
- Respect for patient autonomy and informed consent
- If patients lack an understanding of the benefits and burdens of device therapy, they are less capable of making informed decisions. - Nonmaleficence—One ought not to inflict evil or harm—Some patients may experience decrements in quality of life leaving them worse off than before device implantation - Distributive justice—fair and equitable distribution of resources—”To each his or her equal share”. Substantial justification is required for more than an equal share. |
|
|
nonmaleficence
|
- Nonmaleficence—One ought not to inflict evil or harm—Some patients may experience decrements in quality of life leaving them worse off than before device implantation
- Distributive justice—fair and equitable distribution of resources—”To each his or her equal share”. Substantial justification is required for more than an equal share. |
|
|
Distributive justice
|
- Nonmaleficence—One ought not to inflict evil or harm—Some patients may experience decrements in quality of life leaving them worse off than before device implantation
- Distributive justice—fair and equitable distribution of resources—”To each his or her equal share”. Substantial justification is required for more than an equal share. |
|
|
Alcoholism also affects the heart muscle how
|
it causes cardiac hypertrophy (hypertensive cardiovascular disease), and cardiac arrhythmias
|
|
|
if pts skin is VERY dry in an autopsy... what could it be
|
diabetes? dehydration from hyperglycemia / and or renal failure). Well groomed.
|
|
|
Dilated cardiomyopathy
|
a condition in which the heart becomes weakened and enlarged. As a result, the heart cannot pump enough blood to the rest of the body. There are several different types of cardiomyopathy. Dilated cardiomyopathy is the most common form.
|
|
|
Most vulnerable part of the myocardium-
|
the inner third of the myocardium (subendocardial region )
In the inner third of the myocardium (subendocardial region) this is were most of the MI’s and ischemia will start |
|
|
Atherosclerosis
|
- ‘hardening of the arteries’
- Accumulation of fat, cholesterol, and other substances build up and damage the vessel - Calcification and plaque formation - Over time, plaques block the arteries, may rupture and / or break off starts from damage to the ENDOTHELIAL lining --> then invades the muscularis |
|
|
- ‘hardening of the arteries’
- Accumulation of fat, cholesterol, and other substances build up and damage the vessel - Calcification and plaque formation - Over time, plaques block the arteries, may rupture and / or break off |
Atherosclerosis
|
|
|
where does atherosclerosis start?
|
damage to the ENDOTHELIAL lining --> then invades the muscularis
|
|
|
What does atherosclerosis affect?
|
- The large elastic arteries... like the aorta
- medium and large muscular arteries (coronary arteries ) - It is a Disease of the intima (where it starts) – can involve media - It’s the leading cause of death in developed nations and is becoming the leading cause of death in developING nations as diet changes - Commonly referred to as ‘ischemic heart disease’ (IHD)- bc it goes from ischemia to infarction |
|
|
What is the leading cause of death in developed nations and is becoming the leading cause of death in developING nations as diet changes
|
atherosclerosis
|
|
|
atherosclerosis is a Disease of the ______ (where it starts) – can involve ____
|
intima ... can involve media
|
|
|
intima
|
Intima
- Endothelium to internal elastic lamina Media - Smooth muscle - Internal to external elastic lamina Adventitia - Collagen, smooth muscle, vessels, nerves |
|
|
media
|
Intima
- Endothelium to internal elastic lamina Media - Smooth muscle - Internal to external elastic lamina Adventitia - Collagen, smooth muscle, vessels, nerves |
|
|
adventitia
|
Intima
- Endothelium to internal elastic lamina Media - Smooth muscle - Internal to external elastic lamina Adventitia - Collagen, smooth muscle, vessels, nerves |
|
|
What is the purpose of the internal elastic layer of blood vessels?
|
it is so the vessel can constrict and relax
|
|
|
Separates blood stream from vessel wall
|
endothelium
|
|
|
*** endothelium
|
- Separates blood stream from vessel wall
- Non-thrombogenic Vasoregulatory factors - Nitric Oxide (EDRF, vasodilates, prevents aggregation of platelets) - Endothelin-1 (Vasoconstricts, normal response to injury) - Prostacyclin (Vasodilates, prevents aggregation of platelets - Platelet derived growth factor |
|
|
*** vasoregulatory factors of the endothelium
|
- Separates blood stream from vessel wall
- Non-thrombogenic Vasoregulatory factors - Nitric Oxide (EDRF, vasodilates, prevents aggregation of platelets) - Endothelin-1 (Vasoconstricts, normal response to injury) - Prostacyclin (Vasodilates, prevents aggregation of platelets - Platelet derived growth factor |
|
|
**an important point about endothelium
|
it is NON-THROMBOGENIC
--> thats why it needs to be damaged in order to form blood clots |
|
|
insults to the endothelium
|

|
|
|
the results of anything that will cause insult to the endothelium....
|
- atherosclerosis
- thrombosis - ischemia - infarct - death |
|
|
**risk factors
|
*Cigarette smoking
- Endothelial damage, hypoxia Hypertension - Accelerates atherogenesis Lipoproteins (LDL) - Cholesterol, hyperlipidemia *Diabetes Mellitus Obesity |
|
|
risk factors
|
Family (parent or sibling, cardiac death < 55 year old)
Estrogen via lipoproteins Age (Men > 45 year old, Women > 55 year old) Exercise Lifestyle Synergism of the above |
|
|
Three stages of atherogenesis:
|
Initiation
Adaptive Clinical |
|
|
initiation of atherogenesis
|
- Endothelial dysfunction and / or accumulation of smooth muscle cells (predisposition at branching points)
- Disruption of endothelium - LDL internalized by intimal smooth muscle cells - Reactive oxygen species - Further endothelial disruption - Buildup of macrophages - Macrophages ingest lipid and become foamy - Cytokines released - Macrophage accumulation and smooth muscle proliferation |
|
|
fatty streak
|
- IN the beginning of atherosclerosis
- We start to see Fatty streaks in the aorta (in the large elastic vessels) - Can start early in age - Yellow flat intimal lesion - Lipid laden macrophages - Few lymphocytes and smooth muscle cells - Regression or progress to fibrofatty plaque |
|
|
intimal thickening
|
increase in smooth muscle cells and connective tissue
|
|
|
FIBROFATTY (ATHEROMATOUS) PLAQUE
|
- Elevated, white/yellow
- Often eccentric - Eventually fuse - Neovascularization – new vessels are thin and delicate and may rupture leading to an acute expansion of the plaque |
|
|
cells involved in fibrofatty (atheromatous) plaque
|
- endothelium
- foam cells - smooth muscle - macrophages - lymphocytes - lipids, lipoproteins - serum proteins |
|
|
matrixes involved in fibrofatty (atheromatous) plaque
|
- collagen
- proteoglycans - elastin - glycoproteins |
|
|
2nd stage of atherogenesis - adaptive
|
- As lumen size decreases, the vessel remodels to try and maintain normal caliber
- Collaterals - Once the lumen is narrowed to 45% of its original diameter, cannot compensate (there will be no more collateral flow) |
|
|
3rd stage of atherogenesis - clinical (complicated plaque)
|
- Stenosis >75%
- Ulceration, Fissure, Thrombus - May have intraplaque hemorrhage - Dystrophic calcification - Aneurysm - Rupture (thrombus = acute) - Lifestyle change and medications may cause regression of plaque |
|
|
syndromes of atherosclerosis
|
- Angina pectoris (chest pain):
---> Stable – Atheroma which limits blood flow, especially under stress ---> Unstable – Thrombus overlying plaque, not fully occlusive - Myocardial infarct - Sudden death |
|
|
angina pectoris
|
- chest pain from the heart muscle itself bc of a lack of blood flow (ischemia , infarct )
-usually occurs when Occlusion > 75% - No death of myocytes - Ischemia leads to pain: ---> Substernal, down LEFT arm ---> Pressure on chest ---> “Heartburn” |
|
|
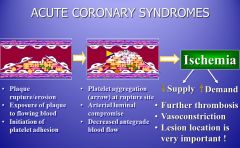
ACUTE CORONARY SYNDROMES
|
|
|
|
complications of atherosclerosis
|
Occlusion of vessel, thrombus or embolus:
- Myocardial infarct - Stroke (intracerebral hemorrhage) Peripheral Vascular Disease (lower extremities) Aortic Aneurysm |
|
|
acute myocardial infarction
|
- Increased morbidity and mortality
- Same symptoms as angina but more severe and lasting at least 20 minutes - Sweating, shortness of breath, nausea, radiating pain , Pale - Diagnosis made by ECG, laboratory tests (troponins, CK) |
|
|
Location of the myocardial infarct will depend upon what
|
the artery that is occluded.
|
|
|
What happens if you have a blockage of the left anterior descending coronary artery?
|
Have ischemia and infarct of the anterior wall of LV, and apex
|
|
|
*Most vulnerable part of the myocardium?
|
Inner 1/3rd *
|
|
|
Zone of perfusion
|
the initial insult of the myocardial wall (inner 1/3rd most vulnerable part of the myocardium)
|
|
|
Zone of necrosis
|
when it fans out and my become transmural
|
|
|
Cardiac Myocytes
|
Myocytes- the specialized cells of the myocardium
Fibroblast- provide structure and support for the myocytes ( they are like an infrastructure) - Ischemic changes within seconds - Buildup of noxious substances (lactate) - Loss of contractility within 60 seconds - Still reversible until 30 minutes when myocyte coagulation necrosis - Classic MI in 2 to 4 hours, irreversible damage - Necrosis complete within 6 hours (unless collaterals) |
|
|
what happens when you lose myocytes?
|
they will NOT regenerate
--> replaced by fibrous scar tissue |
|
|
CONSEQUENCES OF ISCHEMIA
|
Cardiac arrhythmia
Sudden death due to Ventricular Fibrillation |
|
|
*** Factors affecting the severity and outcome of the myocardial infarction
|
- The location, severity, and rate of development of coronary atherosclerotic obstructions
- The size of the vascular bed perfused by the obstructed vessels - The duration of the occlusion - The metabolic/oxygen needs of the myocardium at risk - The extent of collateral blood vessels - The presence, site, and severity of coronary arterial spasm - Other factors, such as alterations in blood pressure, heart rate, and cardiac rhythm |
|
|
when looking at a cross-section of a heart... how can you tell between the anterior and posterior walls?
|
posterior wall is always flat
|
|
|
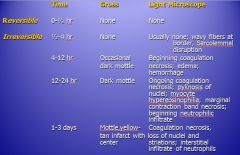
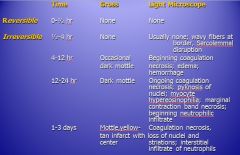
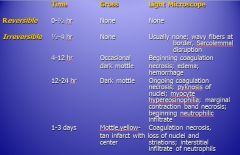
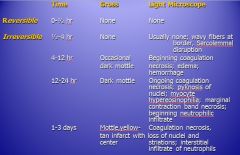
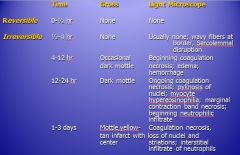
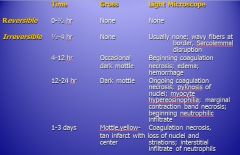
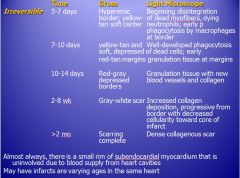
how long is a reversible MI
|
|
|
|
MI for 1/2 - 4 hours....
|
|
|
|
MI for 4 - 12 hours....
|
|
|
|
MI for 12 - 24 hours....
|
|
|
|
MI for 1-3 days...
|

|
|
|
how long would you have to have a MI infarction before it shows up on gross look... and you can see the beginning of coagulation on light microscope ?
|
4 - 12 hours
|
|
|
how long before you would see a dark mottle in the heart.. and under light microscope see pyknosis of the nuclei and myocyte hypereosinophilia & contraction band necrosis?
|
12 - 24 hours
|
|
|
how long before you would see a mottle, yelllow-tan infarct on heart and under microscope, see coagulative necrosis, loss of nuclei and striations
|
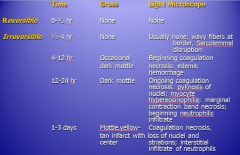
1-3 days
|
|
|
general outline of an evolving MI
|
couple of dats --> increase of neutrophils
couple of weeks --> increase of granulation tissue couple of months --> scar tissue |
|
|
when is scarring complete in a MI
|
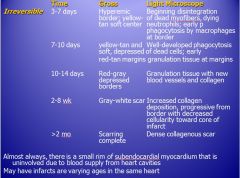
> 2 months
|
|
|
when does granulation tissue form during an evolving MI
|
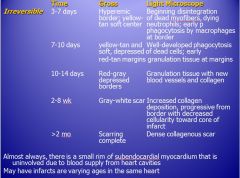
10-14 days
|
|
|
when, during an evolving MI, would you see a hyperemic order, yellow-tan soft center.. and under a microscope see beginning of the disentigration of dead myofibers & dying neutrphils
|
|
|
|
Coagulative necrosis
|
the myofibrils are breaking apart bc the normal adjacent myocardium is pulling on he fibers and the fibers start to break apart
|
|
|
Complications of Myocardial Infarction
|
Contractile dysfunction
- Heart failure, cardiogenic shock Arrythmias - Relies on location of infarct Cardiac rupture - Free wall, septum and papillary muscle - 3 to 7 days most often Pericarditis |
|
|
When are you most vulnerable to rupture the periocardium?
|
3-7 days you are most prone to get cardiac rupture b/c that when you have intense coagulative necrosis , and the fibroblast have still not come in to lay down that fibrous scar tissue
|
|
|
therapy for MIs
|
- Thrombolytics:
---Streptokinase, t-PA (tissue type plasminogen activator) - PTCA (balloon angioplasty) - CABG (Coronary artery bypass grafts) - Stents - Long term anticoagulants! |
|
|
difference between atherosclerosis and hypertension
|
in atherosclerosis... there are SYMPTOMS
- angina pectoris - impedes perfusion hypertension - NO symptoms (no pain) - pressure IN the vessels - does NOT impede perfusion |
|
|
what is important about the fact that hypertension is "systemic"
|
HTN is systemic !!
not only affects the smaller vessels of the heart.. but ALSO the brain and the kidneys !!! the "end" organs |
|
|
myocytes increase in _____ , NOT ______
|
myocytes increase in SIZE, not in NUMBER
|
|
|
hypertension (definition)
|
- a chronic condition in which the blood pressure in the arteries is elevated.
- Blood pressure is determined by two measurements - systolic and diastolic - which depend on whether the heart muscle is contracting (systole) or relaxed between beats (diastole). - HTN / HBP IS HEART DISEASE!!!!! |
|
|
is hypertension / high blood pressure heart disease?
|
YES !!!
- a chronic condition in which the blood pressure in the arteries is elevated. - Blood pressure is determined by two measurements - systolic and diastolic - which depend on whether the heart muscle is contracting (systole) or relaxed between beats (diastole). - HTN / HBP IS HEART DISEASE!!!!! |
|
|
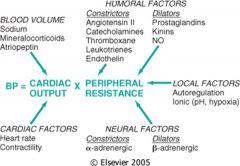
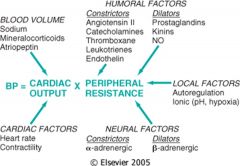
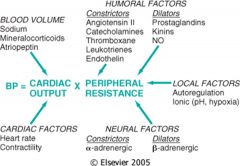
blood pressure = ??
|
Blood Pressure = Cardiac Output x Peripheral Vascular Resistance
- Alteration in either CO or PVR can alter BP - If Cardiac Output is low, need to increase Peripheral Vascular Resistence to maintain blood pressure - Thus low renal perfusion - Cycle continues |
|
|
What factors affect cardiac output?
|

|
|
|
What are the 3 types of factors that affect peripheral vascular resistance?
|
1) humoral
2) local 3) neural |
|
|
What are the humoral factors that affect peripheral resistance?
|
|
|
|
What are the local factors that affect peripheral resistance?
|
|
|
|
What are the neural factors that affect peripheral resistance?
|

|
|
|
Clinical parameters of High Blood Pressure
|
Systolic pressure >140 mm Hg
Diastolic pressure > 90 mm Hg Malignant HTN >200 / 120 mm Hg - Rapid onset - Complications within 1 to 2 years - The higher the BP, the greater risk of complications - Control significantly decreases morbidity and mortality |
|
|
hypertension
|
- “Silent killer”
---> Asymptomatic (UNLIKE atherosclerosis) ---> 25% of population - Idiopathic (essential) – 95% - Secondary (tumors, syndromes) – 5% - Genetic / Familial / Racial Predisposition - Environmental / Lifestyle (obesity, stress, cocaine) - Hypertension is a Systemic Illness ---> Causes blood vessel and organ dysfunction and damage |
|
|
What affects cardiac output (autoregulation) ?
|
|
|
|
What affects total peripheral resistance?
|

|
|
|
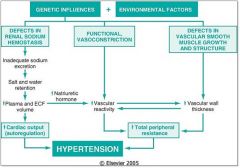
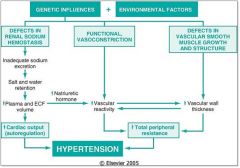
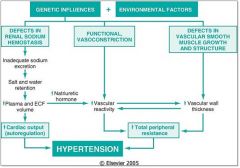
What kind of effect do defects in renal sodium hemostasis have on blood pressure?
|
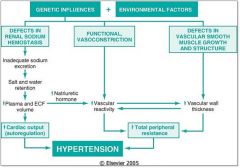
|
|
|
What effect does functional vasocstriction have on blood pressure?
|
|
|
|
What effects do defects in vascular smooth muscle growth and structure have on hypertension?
|
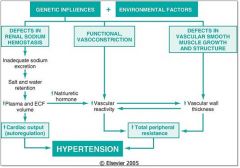
|
|
|
What would increase plasma and ECF volume? And what effect would that have on blood pressure?
|
|
|
|
What kind of effect would a decrease in natrieuretic hormone have on blood pressure?
|
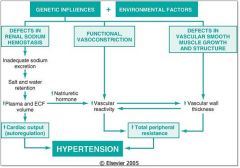
|
|
|
What kind of effect would increasing vascular reactivity have on blood pressure?
|
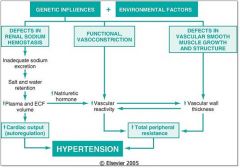
|
|
|
What kind of effect would increasing the vascular wall thickness have on hypertension?
|
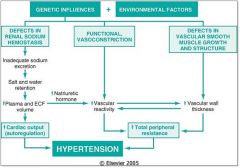
|
|
|
Impact of HTN on Blood Vessels
|
Accelerates atherogenesis
Degenerative changes Arteriosclerosis |
|
|
Systemic Effects of HTN
|
- Myocardial Infarct
- Cardiac Arrhythmias - Congestive Heart Failure - Intracerebral Hemorrhage (stroke) ---> Basal Ganglia ---> Pons - Chronic Renal Failure ---> Dialysis |
|
|
How does HTN affect the heart?
|
- Cardiac hypertrophy
- Concentric left ventricular hypertrophy ---> Leads to stiffness of the wall and poor compliance - Hypoperfusion to heart itself - Abnormal function |
|
|
Myocyte hypertrophy
|
the muscle fibers themselves increase in size NOT number = hypertrophy
we know they are cardiac muscle cells bc they are branching and they have a single centrally placed nucleus |
|
|
Prevention of HTN
|
- Regular Blood Pressure Check-Ups
- Diet - Exercise - Lifestyle changes (cig’s, ETOH, cocaine) - Medication (diuretics AKA water pills) |
|
|
Can HTN be successfully treated?
|
YES !! can be successfully treated and prevented !
|
|
|
risk factors are (additive / synergistic) ?
|
synergistic
--> by eliminating one, you can significantly uncouple the risk |
|
|
what does "pre-cordial" mean
|
"pre-cordial" means "before the heart" --> in front of the heart
also called sub-sternal |
|
|
EKG shows an infarct.. WHAT is an infarct ?
|
- tissue is DEAD
- will NOT conduct |
|
|
what kind of necrosis is an infarct?
|
coagulative
|
|
|
why do people get myocardial infarctions?
|
- NO blood supply
--> b/c of blockage of an artery |
|
|
what is the most common cause of blockage of a coronary artery?
|
a thrombus
(NOT an embolis.. thats rare) |
|
|
what are the 3 coronary arteries?
|
1) LAD coronary artery
---> feeds the apex of the heart (the distal end of the ventricles), the anterior wall of L ventricle, 2/3 of ant. Ventricular septum that separates R & L ventricles 2) Left circumflex artery ---> feeds the post. 1/3 of ventricular septum, and (along with LAD), feeds L ventricular wall 3) Right coronary artery ---> feeds entire R ventricular wall, posterior 1/3 of ventricular septum, postero-basal portion of L ventricle |
|
|
what does the LAD supply blood to?
|
1) LAD coronary artery
---> feeds the apex of the heart (the distal end of the ventricles), the anterior wall of L ventricle, 2/3 of ant. Ventricular septum that separates R & L ventricles 2) Left circumflex artery ---> feeds the post. 1/3 of ventricular septum, and (along with LAD), feeds L ventricular wall 3) Right coronary artery ---> feeds entire R ventricular wall, posterior 1/3 of ventricular septum, postero-basal portion of L ventricle |
|
|
what does the circumflex artery supply blood to?
|
1) LAD coronary artery
---> feeds the apex of the heart (the distal end of the ventricles), the anterior wall of L ventricle, 2/3 of ant. Ventricular septum that separates R & L ventricles 2) Left circumflex artery ---> feeds the post. 1/3 of ventricular septum, and (along with LAD), feeds L ventricular wall 3) Right coronary artery ---> feeds entire R ventricular wall, posterior 1/3 of ventricular septum, postero-basal portion of L ventricle |
|
|
what does the right coronary artery supply blood to ?
|
1) LAD coronary artery
---> feeds the apex of the heart (the distal end of the ventricles), the anterior wall of L ventricle, 2/3 of ant. Ventricular septum that separates R & L ventricles 2) Left circumflex artery ---> feeds the post. 1/3 of ventricular septum, and (along with LAD), feeds L ventricular wall 3) Right coronary artery ---> feeds entire R ventricular wall, posterior 1/3 of ventricular septum, postero-basal portion of L ventricle |
|
|
what is ischemia?
|
LESS bloodflow because of a decrease of the size of the vessel.. perhaps because of atherosclerotic heart
|
|
|
can you die from ischemia?
|
YES
|
|
|
what is CPK?
|
creatinine phospho-kinase (aka creatine kinase)
found in a # of tissues... including the heart if your heart dies... myocardial cells die, releasing CPK into the blood --> when you see elevated CPK levels in serum, must be heart damage |
|
|
what do elevated CPK levels in serum indicate?
|
creatinine phospho-kinase (aka creatine kinase)
found in a # of tissues... including the heart if your heart dies... myocardial cells die, releasing CPK into the blood --> when you see elevated CPK levels in serum, must be heart damage |
|
|
what is the principle cell in a thrombus?
|
platelet
--> ONLY stick on abnormal, rough surfaces |
|
|
what is the most common cause of having emboli
|
from thrombi
|
|
|
where would emboli from the left ventricle go?
|
- would go down the aorta
- could travel down the abdominal aorta - could travel far and go to the kidney - could could up into the ascending aorta into the carotid and give you a stroke |
|
|
what is THE MOST COMMON outcome following an M.I. ?
|
ventricular fibrullation
--> when the tissue dies, it no longer conducts current |
|
|
what kinds of cells are PNMs
|
acute
|
|
|
in chronic disease... what cell types are expected
|
monocytes, macrophages & kymphycytes
--> phagocytoze fat --> when they digest lipids, they become more aggressive and start secreting enzymes (i.e. colalgenase, protease --> further destroying arterail wall) and secrete cytokines that will cause the smooth muscle cells from the media to come over |
|
|
foam cells
|
macrophages that digest lipids
--> phagocytoze fat --> when they digest lipids, they become more aggressive and start secreting enzymes (i.e. colalgenase, protease --> further destroying arterail wall) and secrete cytokines that will cause the smooth muscle cells from the media to come over |
|
|
what types of cells primarily make up the media
|
smooth muscle cells
|
|
|
vasa vasorum
|
blood vessels that feed other blood vessels
The vasa vasorum are found in large arteries and veins such as the aorta and its branches. These small vessels serve to provide blood supply and nourishment for tunica adventitia and outer parts of tunica media of large vessels |
|
|
diabetes has 2 major outcomes
|
1) damage to the small blood vessels (microvascular disease --> eyes, kidneys & nerves)
- controlled by controlling blood glucose 2) macrovascular disease = medium + large size arteries - in diabetes, most common COD is myocardial infarction --> coronary artery diseaase ---> control of blood glucose makes NO DIFFERENCE in this |
|
|
why would you refer to a diabetic as "brittle"
|
means they're not stable
--> blood glucose goes up and down |
|
|
what is SGOT
|
Aspartate transaminase AKA serum glutamic oxaloacetic transaminase (SGOT)
a pyridoxal phosphate (PLP)-dependent transaminase enzyme (EC 2.6.1.1). AST catalyzes the reversible transfer of an α-amino group between aspartate and glutamate and, as such, is an important enzyme in amino acid metabolism. AST is found in the liver, heart, skeletal muscle, kidneys, brain, and red blood cells, and it is commonly measured clinically as a marker for liver health. --> if elevated.. can indicate a problem in one of those organs |
|
|
troponin test
|
The troponin test measures the levels of certain proteins called troponin T and troponin I in the blood. These proteins are released when the heart muscle has been damaged, such as a heart attack. The more damage there is to the heart, the greater the amount of troponin T and I there will be in the blood.
|
|
|
what would cause the tissues to separate during a myocardial infarction?
|
- tissue is dead
- there is inflammation --> edema --> fluid buildup |
|
|
most of the time when people get MI...
|
thrombi in coronary arteries
|
|
|
3 types of arteriosclerosis
|
1) atherosclerosis
--> aorta, coronary, cerebral 2) medial calcinosis --> muscular arteries 3) arteriolat sclerosis --> arterioles |
|
|
medial calcinosis
|
doesnt really do any damage
3 types of arteriosclerosis 1) atherosclerosis --> aorta, coronary, cerebral 2) medial calcinosis --> muscular arteries 3) arteriolat sclerosis --> arterioles |
|
|
arteriolar sclerosis
|
these small arterioles do not have plaques, but does narrow the lumen to them (i.e. kidney)
3 types of arteriosclerosis 1) atherosclerosis --> aorta, coronary, cerebral 2) medial calcinosis --> muscular arteries 3) arteriolat sclerosis --> arterioles |
|
|
most common site for atherosclerosis
|
abdominal aorta
|
|
|
what is a stroke
|
atherosclerosis in a cerebral artery --> thrombus forms --> infarct = stroke
this is liquifactive necrosis |
|
|
diplopia
|
"seeing double"
a result of severe ischemia of the cerebral arteries in the brain |
|
|
transient ischemic attacks
|
when cerebral arteries are occluded.. but not fully blocked off (infarct)
can lead to a major stroke in a short amount of time |
|
|
What can cause pericarditis?
|
- viral common
- fibrinous (acute MI, post MI caleld Dresslers, rheumatic fever) - purulemt or supperative; infections --> friction rub on phys exam (goes away when pt leans forward) |
|
|
Dressler's Syndrome
|
fibrinous pericarditis days after MI
|
|
|
bruit
|
turbulent bloodflow in a large vessel
|
|
|
prophylaxis
|
Amoxicillin 500mg caps
Disp: 4 caps Sig: take 4 caps po 1 hour before dental appt Refills: 0 **for pen allergy Clindamycin 150mg caps Disp: 4 caps Sig: Take 4 capsules po 1 hour before dental appt Refills: 0 |
|
|
prophylaxis for pt with penicillin allergy
|
Amoxicillin 500mg caps
Disp: 4 caps Sig: take 4 caps po 1 hour before dental appt Refills: 0 **for pen allergy Clindamycin 150mg caps Disp: 4 caps Sig: Take 4 capsules po 1 hour before dental appt Refills: 0 |
|
|
Jaw claudication
|
Jaw claudication is pain in the jaw or ear while chewing. This is caused by insufficiency of the arteries supplying the jaw muscles, associated with giant cell arteritis.
--> could be from giant cell arteritis |
|
|
giant cell arteritis
|
- elderly people
- chronic granulamatous inflammation of large to small sized arteries - NOT continuous... 9areas of disease / norml / disease etc) -->> so has "skip areas" ***opthalmic arterial involvement can lead to permanent blindness !! medical emergency !!! usually UNILATERAL |
|
|
amarousis fugax
|
- fleeting darkness
- sudden loss of vision - partial OR complete - one OR both eyes - mild blurring or fogging or complete blackness, and may involve a part of or all of visual field **NEEDS EMERGENCY EVALUATION !!! |
|
|
- fleeting darkness
- sudden loss of vision - partial OR complete - one OR both eyes - mild blurring or fogging or complete blackness, and may involve a part of or all of visual field **NEEDS EMERGENCY EVALUATION !!! |
amarousis fugax
|
|
|
mechanism of injury for amarousis fugax
|
granulamatous !!!!!!
|
|
|
Takayasu aortitis
|
- younger than 50
- like Giant cell arteritis - etiology unknown - large and small vessels - used to be sseen in Japanese now in other groups worldwide --> "pulseless disease) .. associated w. women |
|
|
difference between Takayasu aortis and giant cell artiritis
|
GCA --. elderly
Takayasu - younger than age 50 |
|
|
what cells are in a granuloma
|
giant cells
macrophages |
|
|
buergers disease
|
- segmental thrombosing
- medium and small arteries - acute and chronic inflammation + luminal thrombosis - especially tibial and radical - can extend into veins and nerves of extremities - associated with heavy cigarette smokers < 35 y/o males - tobacco usage essential for initiation and pregression of disease - reported in cigar smokers marijuana users and smokeless tobacco users --> ** 2/3 of people with burgers have periodontal disease |
|
|
what is buerges disease strongly linked with
|
- segmental thrombosing
- medium and small arteries - acute and chronic inflammation + luminal thrombosis - especially tibial and radical - can extend into veins and nerves of extremities - associated with heavy cigarette smokers < 35 y/o males - tobacco usage essential for initiation and pregression of disease - reported in cigar smokers marijuana users and smokeless tobacco users --> ** 2/3 of people with burgers have periodontal disease |
|
|
wegners granulomatosis (w/ poly angiitis)
|
- granulomatous inflammation involving respiratory tract
- necrotizing - small vessels including kidney - nasal or oral ulcers --. painless or painful. >1 month duration - bloody or purulent nasal discharge - CXR: nodules, infiltrates or cavities - urine with hematuria |
|
|
R to L shunt
|
- blood leaves right heart, bypasing lung
- thru shunt - mixes with deoxygenated blood in R heart & oxygenated blood in L heart |
|
|
cardinal features of Tetrology of Fallot
|
- large VSD
- obstruction of RV outflow tract - RVH - aorta overrides VSD |
|
|
what is the most common form of cyanotic congenital heart disease?
|
teratology of fallot
|
|
|
transposition of great arteries (TGA)
|
- aorta arises from RV
- not compatible ith life - ignoring LV - survive with shunt |
|
|
Total anomalous pulmonary venous circulation (TAPVC)
|
- pulmonary veins may not form
- atresia |
|
|
for congenital defects... which are blue... L to R or R to L ?
|
ONLY R to L
ONLY ones that make you blue require prophylaxis |
|
|
PDA (patent ductus aerteriosis)
|
allows blood to go away from the lungs when they re in utero
--> |
|
|
which congenital heart diseases require prohylaxis?
|
the ones that cause caynoiss !!
aka all the R to L shunt disorders !!! "take time to prophylax the T's" |
|
|
"take time to prophylax the T's"
|
any congenital heart disorder with a R to L shunt causes cyanonis and needs prohylaxis
|
|
|
what is the most common cyanotic CHD?
|
teratolgy of fallot
|
|
|
what is the most common CHD?
|
Ventricular Septal Defect (VSD)
|

