![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
17 Cards in this Set
- Front
- Back
|
Primary Immunodeficiency
occurence? cause? result is? |
-relatively rare
-inherited and congenital -result in a predisposition for infections |
|
|
X-linked agammaglobulinemia:
defect in? type of infection? with what type of organism? levels of immunoglobulins? B cell/proB/preB levels? lymphoid tissue? defect in? diagnosed by? therapy? |
Pre-B cell to immature B-cell or pro-B cell to pre B-cell
-recurrent respiratory with encapsulated bacteria -low levels of all immunoglobulin classes -B-cells absent from blood, but preB or proB cells are normal -lacks germinal centers and plasma cells -defect in signal transducing molecule BTK or tyrosine kinase gene on long arm of chromosome X(xq22) |
|
|
Order to B cell maturation
|
stem cell
early pro B late pro B Large pre B-intracellular/surface U chain receptor small pre-B-intracellular U chain R immature B cell-IgM expressed on cell surface Mature B Cell-IgD and IgM on surface |
|
|
Process of elimination for:
bacteria toxins, extracellular space, plasma |
toxins(H. influenza):
cell with receptors for toxin neutralization ingestion by macrophage extracellular space(s. pneumoniae) -opsonization-ab surround microbe -ingestion by macrophage bacteria in plasma(s. aureus) -ab surround microbe -complement activation lysis and ingestion |
|
|
encapsulated removal
|
-resist uptake by neutrophils and avoid engulfment
-binding of IgG2 Abs to the bacterial surface leads to activation of complement and binding of C3b |
|
|
Flow Cytometry
|
-fluorescent aBs against cells you want to study
-cells forced through a small stream single file -hit by laser lights of different wavelengths for exication -regular white light: see how big cells is -look at shadow to determine size(aka forward scatter) -red PMT/90 degree laser assesses granularity -filters only take up certain fluorescent signals...ref fluorescence will be taken up by redPMT. |
|
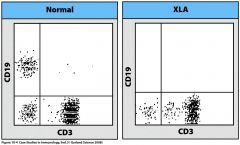
what does this show?
|
y-axis = granular
x-axis: size bottom left = small dead cells CD19 = antigen on B-cells CD3 = antigen on T cells Normally patient has mature B and T cells...in XLA patient has T cells but not B cells |
|
|
Isolated IgA deficiency
defect in? sx? immunoglobulin levels? other complications? treatment? |
-failure in B cell differentiation
-signaling molecules which allow IgA to be produced is absent in these patients -->can't develop IgA positive b-cells -asx but some have recurrent upper respiratory infections, autoimmune disease, allergies and Gi disease -other Ig levels are normal -20-40% have anti-IgA antibodies that lead to nonhemolytic transfusion reactions -immunoglobulin replacmeent is not a treatment option-patients at risk for developing aBs against IgA as they have none -treat infections aggressively |
|
|
Hyper-IgM syndrome happens because?
|
-there is no isotype switching occurs, so no IgE, IgA, IgG
|
|
|
IgG subclass deficiency:
-characterized by? -exhibit what kind of infections? -assoicated with? -treatment? |
-usually one or more subclasses are deficient
-exhibit recurrent bacterial and respiratory infections -often assoicated with other immunodeficiencies such as ataxia-telangiectasia -iv immunoglobulin |
|
|
X-linked Hyper-IgM Deficiency
caused by? characterized by? forms of disease? complications? |
-IgMs which cannot class switch due to mutated CD40L on t-cells
-thus cannot produce aB except for IgM -high levels of Igm and low levels of other isotypes -primary and acquired -recurrent infxns with pyogenic bacteria in infancy |
|
|
digeorges syndrome
what is blocked? what are the consequences of this blockage? |
maturation of t-cell blocked
-no mature CD8s and CD4s -cannot activate B cells |
|
|
Architecture of the Thymus
|
-Cells mature as they move the cortex(outside) to the medulla(inside)
-notch signalling is crucial for maturation..otherwise get a defect in T-cell maturation |
|
|
Digeorge syndrome
-physiological cause? -sxs begin to show? -causes what abnormalities -effect on immune system -antibody levels and fxns? -complications? -treatment -would a bone marrow transplant help? |
-congenital apasia or hypoplasia of thymus and parathyroid glands due to inhbited growth of 3rd and 4th pharyngeal pouches
-right after birth -low set malformed ears, fish mouth -absence of cell mediated immunity and low levels of circulating T-cells -antibody levels and fxn are variable -susceptible to fungal and viral infections(cell mediate immunity deficient) -treatment: involves monitoring heart disease, hypocalcemia, and prophy for pneumocystis(yeast infxn handled by adaptive immunity) -no problem in thymus |
|
|
Common Variable Immunodeficiency
-what is impaired? -defect in? -occur at what age? when do u see sx? -diagnosis -complications? |
-B and or T cells(defecient in ICOS)
-defect maturation of B-cells leads from either cannot have T and B cell interaction or B cell problem itself-->no plasma cells -any age, 15-35 -lack plasma cells, dx is usually one of exclusion...cannot pinpoint whether problem is in T-cells or B cells -increase susceptibility to respiratory infxns -high prevlance of autoimmune disease |
|
|
Adenosine deaminase deficiency
-deficiency at what level? leads to? -treatment? |
-enzyme deficiency at stem cell level which affects B and T cells maturation
-bone marrow transplant |
|
|
Severe Combined Immunodeficiency
-generally caused by -most common form? -autosomal recessive forms characterized by? -leads to defects in? -complications -treatments? |
-group mutations impt for T-cell maturation
-X-linked, mutation in gamma chain of IL-2-Receptor(for activation of T cell) -adensoine deaminase deficiency and HLA class I and class II antigen deficiencies(bare lymphocyte syndrome) -complete/partial defective T/B cell fxn -viral, bacterial and fungal infxns b4 6 months of age -fungal infxns on mucosal surfaces -antimicrobial and bone marrow transplant |

