![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
Def'n of inflammation
|
-protective response to microbial invason or injury to tissue ends with permanent destruction of tissue or with complete healing
|
|
|
Componenets of Inflammation
|
elevated cellular metabolism
|
|
|
Sx of Inflammation
|
Calor(heat)
Rubor(red) tumor(swelling) Dolor(pain Loss of fxn |
|
|
Tissue Mediators and what they do
histamine PG LT Lysosomal Products Lymphocyte Products Macrophage products Mast cell Products Eosinophil products |
Histamine: released by a variety of physical and chemical stimuli.
Prostaglandins: platelet aggregation, vasodilation, vascular permeability and increase pain sensitivity to other mediators Leukotrienes: involved in immediate hypersensitivity Lysosomal Products: damaged host tissue such as collagen, elastin, mucopolysaccharide and basement membrane. Lymphocyte Products -ILs-->T/B cells -MCP1 acumulation of monocyte -GMCSF(granulocyte/macrophage colony stim factor) -INFa -Skin reactive Factor Macrophage products: reactive metabolites of oxygen, INF@, IL-1, TNF@ Mast Cell: histamine Eosinophils: lyosomal enzymes |
|
|
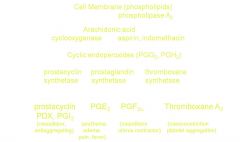
PGs derivation
|
|
|
|
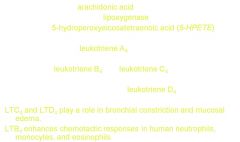
Leukotriene Formation
|
|
|
|
Plasma Mediators
|
Kinins
-bradykinin-increase cap. permeability, vasodilator, pain Complement system -inflammatory process -C3a and C5a-->bacterial lysis, phagocytosis, chemotaxis, vasodilation, increase perm NO: regulatory and proinflammatory role in various inflammatory conditions -inhibition of this = antiinflammatory |
|
|
Antiinflammatory Drug Types
|
Nonsteroidal antiinflame agents
steroidal agents |
|
|
nonsteroidal anti-inflam agents
types? exception? -curative? specific? mechanism? |
cox inhibitors
disease-modifying antirheumatic drugs(MARDs) except: paramainphenol derivatives: acetaminophen palliative, not curative nonspecific reduce body defense mechanisms |
|
|
Selectivity of Cox1/Cox 2 inhibitors
|
Negative = Cox 2
-xibs, Eto, Melo positive = Cox1 -Ibuprofen -Nap -Flurbi -Ketop -Asprin -Ketor |
|
|
Salicylates
prototype? mechansim? use? side effects? |
-aspirin
-irreversibly acetylates Cox -RA, Reiters, TMJ, ankylosing spndylitis, platelet aggregation -side effects: GI bleeding, ulcers, renal, Reyes(encephalopathy) |
|
|
Indole and Indene Acetic Acids
|
-indomethacin/indocin
-Etodolac(iodine) |
|
|
Indomethacin
mechanism? vs. aspriin? side effects? Etodolac -for? -peak plasma concentration? |
-inhibitor of Cox
-better for ankylosing spondylitis/OA -only with long-term admin Etodolac: -acute pain, RA, OA -pp at 1-2 hrs |
|
|
Antiinflammatory and COX inhibitory activity of some NSAIDs compared with acetaminophen
|
-Indomethacin is more effective/potent than aspirin
-acetaminophen has little anti-inflam effects and not very potent |
|
|
Enolic Acids
|
Piroxicam: Feldene
-equivalent to asprin. indomethacin, naproxen for RA/OA -better tolerated than aspriin and indomethacin -long 1/2 life Meloxicam: Mobic -equiv to diclofenac, naproxen, piroxicam -fewer adverse effects as week cox 2 inhibitor Other oxicams: Nabumetone(relafen) -good for RA, OA, short term soft tissue -little GI toxic |
|
|
Phenyl Acetic Acid Derivatives
mechansim? potency? analogue? long-term used for? shor-term be used for toxic effects? what is arthrotec? |
-Dicolofenac: phenyl acetic acid derivative
-weak cox 2 inhibitor -potency greater than indomethacin -long term for RA/ OA/AS -short term: acute musculoskeltal injury, acte painful shoulder, posoperative pain and dysmennorhea -toxic effects: GI -arthrotec: volatren + misoprostol |
|
|
Pyrrole Derivatives
prototype? derivative of? effects? side effects? |
-Ketorolac: heteroarl acetic acid derivative
-potent analgesic but only moderately effective antiinflammatory drug -relatively high incidence of GI ulceration and bleeding |
|
|
Selective Cox2 inhibitors
|
-Diaryl sub furanones: Rofecoxib
-Diaryl sub pyrazoles: Celecoxib -Diarly sub isoxazole: valdecoxib |
|
|
Rofecoxib:
used for? Celecoxib used for? Valdecoxib used for? |
-OA, acute pain, dysmennorhea-withdrawn from market
Celecoxib: OA/RA-FDA alert Valdecoxib: Sx of OA, RA, menstrual discomfrot-withdrawn |
|
|
NSAID adverse effects
|
CV risk: heart failure
GI ADRs: -indomethacin, ketoprofen, piroxicam high risk -ibuprofen diclofenac low Renal ADRs: change in haemodynamics which are usually medaited by PGs |
|
|
Implication for Dentistry
|
-Asprin/NSAIDS-->relieve pain
-TMJ disorder |
|
|
Disease Modifying Antirheumatic Drugs(MARDS)
act on? |
immune system to slow progression of RA
ex. anti-malaria plaquenil, cyclosporin, chemotherapy drugs, methotrextate, arava, azulfidine, gold, bio-drugs |
|
|
Plaquenil fxn?sideffects?
Neoral fxn?side effects? Arava fxn? side effects |
-antimalril/immunosuppessive fxn
-occular toxicity -immunosuppresant -increase susceptibility to infectiion, cancer, kidney things -pyrimidine synthesis inhibitor -can cause serious birth defects |
|
|
Methotrexate fxn?
Gold compounds fxn? toxicitiy? |
-inhibits folic acid slow down growth of cells
-Gold: -inhibit PG synthesis -suppress cellullar immune rxns -inhibit lysosomal hydrolases, -diminish phag activity of mononuclear cells Toxic: stomatitis, blood dyscrasias |
|
|
Gout Arthritis caused by?
|
acute attack of gout occurs via an inflammatory rxn to crystals urate that are deposited in the joint tissue
|
|
|
Clinical Manifestation of gout
|
Acute:
-deposition of sodium urate mucopolysaccharide in synovial fluid which activates Haegeman factor and leads to BRADYKININ formation -neutrophils actively phagocytize urate crystals leading to release of LYSOSOMAL ENZYMES and increased LACTIC ACID PRODUCTION Tophaceous deposit: sodium urate deposits in/around joints in cartilage, bone, bursae and subcutaneous tissue Uric Acid nephrolithiases: formation of urate stone goutry kidney: nephropathy |
|
|
Drugs used for gout
|
Colchicine
Allopurinol Uricosuric |
|
|
Colchicine
effective against? mechansim? side effects? toxic effects |
-gouty arthritis
-inteferes with mitotic spindles causing depolymerization and disappearnce of fibrillar microtubules in granulocytes and other motile cells -inhibits migration of granulocytes into inflamed area as well as decreased metbolic/phagocytic acitivty of granulocytes -SE: nausea/vomitting, diarrhea, abdominal pain -GI/Kidney/muscle/vascular |
|
|
Allopurinol
-fxn? |
-metabolite is alloxanthinine which is an inhibitor of xanthinine oxidase which is required to synthesize uric acid
|
|
|
uricosuric drugs
mechanism? prototype? therapy instructions? blunted by? can block? |
-higher doses block tubular reabsorption of urate...increasing urinary exceretion of uric acid and lowering serum urate concentration
-probenecid -fluid intake maintained for akaline diuresis -salicylates -block renal excretion of penicillin |
|
|
Adrenal corticosteroids
2 classes? production regulated by? |
corticosteroids: 21 carbon atoms
androgens: 19 carbon atoms except aldosterone...regulated by blood concentration of ACTH from AP |
|
|
Feedback mechansim for cortisol
|
hypothalamus releases CRH
stimualte pituitary to release ACTH stimulate adrenal to release cortisol negative fdbk: cortisol at all parts, ACTH on hypothalamus |
|
|
Physio fxns and Pharm effects
|
carb/protein metaboism: diminish glucose usage and increase protein breakdown
lipid metabolism: redistribute body fat and induction of lipolysis in adipocytes electrolyte/water balance immunosupressive action: suppress cell mediated immune Antiinflammatory effects |
|
|
Mechanisms of antiinflammatory effeccts
|
1. production of lipocortin (an inhibitory protein of phospholipase A2).
2. suppress the synthesis of COX. 3. inhibition of eosinophils, basophils, monocytes, and lymphocytes. 4. inhibit the synthesis of cytokines (interleukins and TNF-) in immune cells 5. inhibit histamine release. 6. inhibit the production of adhesion molecules in endothelial cell |
|
|
Therapeutic uses
|
-Replacement therapy
-Collagen-vascular disease: lupus, connective tissue -Rheumatic/joints -Grafts/Transplants -Skin problems -Hematologic problems |
|
|
Uses for Dentistry
|
-Oral ulceration(including desquamtive gingivitis and stomatitis)
* do not use for herpetic gingivostomatis -pulpal hypersensitivity -TMJ -Post operative -Anaphylaxis |
|
|
Adverse Effects
|
Hyperglycemia and glycosuria
Myopathy Suppression of growth Negative nitrogen balance Peptic ulcer Ocular effects Edema and hypokalemia Altered distribution of body fat Increased susceptibility of infection Suppression of pituitary-adrenal function |
|
|
Contraindications
|
-Viral/bacterial/fungal
-diabetes mellitus-leads to higher glucose levels -peptic ulcer -high blood pressure |
|
|
1/2 lives
short = 8-12 intermediate = 18-36 long = 36-72 |
short: cortisone hydrocortisone
intermediate: methylprednisolone, Prednisone(olone), Triamcinolone long acting -Paramethasone -betamethasone -dexamethasone |

