![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
53 Cards in this Set
- Front
- Back
|
At what age do strokes begin to account for the majority of deaths?
|
For 65 and greater, strokes account for 70-80% of deaths.
|
|
|
What are the common SXS of stroke?
|
1) Sudden onset
2) Hemiparesis 3) Aphasia/Dysphasia 5) Loss of consciousness |
|
|
Are all CVD pathologies sudden in onset?
|
No. Vascular dementia has an insidious onset.
|
|
|
What are the two major types of stroke?
|
Ischemic or Hemorrhagic
|
|
|
What are the risk factors for CVD?
|
1) arteriosclerosis
2) HTN 3) Cardiac Hx 4) DM |
|
|
What are TIAs?
|
Transient Ischemic Attacks, or "mini-strokes." By definition, they symptomatically clear within 24 hours.
|
|
|
What is "encephalomalacia"?
|
Brain softening, due to hemorrhage or inflammation
|
|
|
What "color" are Ischemic Infarctions?
|
Ischemic infarcts appear white, pale, or gray.
|
|
|
What are the three pathologic classifications of an ischemic infarct?
|
1) Fresh - within two days
2) Recent - days to weeks 3) Old - weeks+ |
|
|
What are the characteristics of a "fresh" cerebral infarct?
|
Gross - poor demarcation, dusy/grey, RBCs.
Micro - "Red" ischemic neurons, eosinophilic cytoplasm, pyknotic nuclei, PMNs |
|
|
What are the characteristics of a "recent" cerebral infarct?
|
Gross - well defined, "softer, granular" lesion
Micro - Macrophage aggregates, astrocytes with early hyperplasia |
|
|
What are the characteristics of a "old" cerebral infarct?
|
Gross - defined cavity lined with "rust-colored" membrane
Micro - Few BVs, lipid/hemosiderin-filled macrophages, margins made of glial cells/astrocytes |
|
|
What is the gross appearance of a hemorrhagic stroke?
|
BVs will have sustained damage, therefore they'll leak, causing petechial hemorrhages in the parenchyma.
|
|
|
What are the three main causes of CVD?
|
1) Thrombosis
2) Embolism 3) Intrinsic vessel disease |
|
|
What are the main emboli that can lodge in the brain?
|
Bacteria, fat globules, gas bubbles, cancer cells, and especially cardiac mural thrombus fragments.
|
|
|
What three types of arteriosclerosis may lead to a CV event?
|
1) Atherosclerosis - plaque deposition/cholesterol. May embolize.
2) Arteriolar sclerosis/fibrosis from longstanding HTN 3) Arteritis - many causes |
|
|
What is a leukoencephalopathy?
|
A disease of the white matter (myelin, etc.) of the brain.
|
|
|
Can infarction lead to hemorrhage?
|
Yes. Infarction can weaken vessel walls, leading to aneurysm or hemorrhage.
|
|
|
What are the four major, permanent outcomes of CVD?
|
1) Infarction
2) Intracranial hemorrhage 3) Anoxic leukoencephalopathy 4) Dementia |
|
|
What type of infarction does cerebral hypotension produce?
|
Hypotension produces "Borderzone Infarcts" (garden sprinkler analogy)
|
|
|
Infarction of a cerebral artery produces what kind of infarction?
|
Major arterial infarction produces a "Territorial Infarct"
|
|
|
Infarction of a cerebral arteriole produces what kind of infarction?
|
Arteriole infarction produces a "Lacunar" or "Binswanger's" infarction.
|
|
|
Cerebral venous thrombosis produces what kind of infarction?
|
Cerebral venous thrombosis produces a bilateral, hemorrhagic infarction.
|
|
|
What are the five causes of a Regional Arterial Infarct?
|
1) Atherosclerosis
2) Thromboembolism 3) Dissection 4) Vasospasm 5) Vasculitis |
|
|
What percentage of Regional Arterial Cerebral Infarcts progress to hemorrhage?
|
40%
|
|
|
Hemorrhagic infarction is commonly associated with...
|
...a preceding embolic etiology.
|
|

When did this lesion occur?
|
Acute Hemorrhagic Infarct
|
|
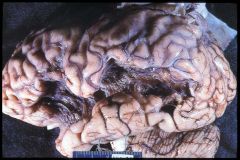
When did this lesion occur?
|
Remote Hemorrhagic Infarct.
|
|
|
What is Wallerian Degeneration?
|
Loss of axonal projects following the death of the neuron cell body (e.g., pyramidal tract degeneration following a supratentorial infarct.)
|
|
|
What is the typical cause of a Regional Infarct?
|
Arteriolosclerosis, typically involving a basal penetrating artery.
|
|
|
What are the 3 most common complications of a regional infarct?
|
1) Lacunar infarction
2) Micro-aneurysm 3) Hemorrhage |
|
|
What is a Lacunar Infarction? What is the typical cause of a lacunar infarction?
|
Lacunar infarctions are caused by occlusion of a deep penetrating artery in the brain. They scar by leaving small "lakes" of fluid. They are typically caused by hypertension.
|
|
|
What are the four causes (given in lecture) for "Regional" or Capillary cerebral infarction?
|
1) TTP - Thrombotic Thrombocytopenic Purpura
2) Rickettesial infection 3) Fat emboli 4) Air emboli |
|
|
What are the pathologic signs of a regional/capillary infarction?
|
Gross - Petechial hemorrhage, typically widespread
Micro - Perivascular loss of Myelin |
|

What is the pathology?
|
Regional infarction with petechial hemorrhages.
|
|
|
What are the common causative factors in cerebral venous thrombosis?
|
1) Dehydration
2) Hypercoaguable State 3) Phlebitis 4) Compression/infiltration by neoplasm |
|
|
What is the typical lesion pattern for a cerebral venous thrombosis?
|
Bilateral hemorrhagic lesions
|
|
|
What are the two most common locations for cerebral venous thrombosis?
|
The central and superior sagittal sinuses.
|
|
|
What are the two cell types most vulnerable to global ischemia?
|
1) CA1 neurons in the hippocampus
2) Purkinje neurons in the cerebellum |
|
|
What is the most common cause of global ischemia?
|
A hypotensive event.
|
|
|
The zone between which to cerebral arteries is most vulnerable to "border zone lesions"?
|
The cortical neurons between the Anterior and Middle cerebral arteries.
|
|
|
Besides the internal carotid, which arterial supply may provide very limited nourishment to the brain?
|
The meningeal arteries, via external carotid, provide limited nourishment to the very outermost cortical neurons.
|
|
|
What are the GROSS indications of Acute, Subacute and Remote brain injury?
|
Acute: none
Subacute: edema, liquefaction Remote: progressive cavitation |
|
|
What are the GROSS indications of Acute, Subacute and Remote brain injury?
|
Acute: "red" neurons
Subacute: transient neutrophils, massive macrophages Remote: rim of astrogliosis |
|
|
What is the most common cause of an epidural hematoma? Which artery is usually damaged?
|
1) Commonly caused by a depressed skull fracture
2) Middle meningeal artery usually damaged. |
|
|
Why do epidural hematomas progress relatively quickly?
|
Damage to a high-pressure artery forces the epidural potential space to form.
|
|
|
What is the most common cause of a subdural bleed?
|
Tearing/rupture of a Bridging Vein. Atrophic changes in elderly brains make them more vulnerable.
|
|
|
What are three common causes of a subarachnoid hemorrhage?
|
1) Congenital (berry) aneurisms
2) Septic aneurysm 3) AVM |
|
|
What is the most common cause of an intracerebral hemorrhage?
|
Hypertension, most commonly affecting the basal ganglia, although a variety of other causes exist:
1) Amyloid angiopathy (usually lobar) 2) Post-infarction hemorrhage 3) Neoplasm and trauma |
|
|
Cerebral Amyloid Angiopathy
|
Deposition of beta-amyloid in small arteries, typically lobar. Seen in advancing age, familial and sporadic causes, as well as with AD.
|
|
|
A neonatal hypoxic event may lead to what cerebral bleed?
|
Germinal Matrix Hemorrhage.
|
|
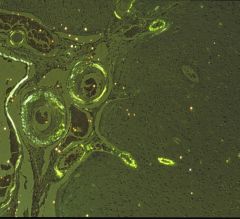
Name the pathology
|
Cerebral Amyloid Angiopathy, demonstrated here by apple/green birefringence from a Congo Red stain.
|
|
|
The following symptomatology suggests what?
1) Vertigo, nausea, nystagmus 2) Ipsilateral facial pain/temp sensation and Horner’s sxs 3) Contralateral impaired body pain/temp sensation |
Wallenburg's Syndrome, caused by an embolization/infarction of the PICA
|

