![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
How many stages are there for evaluating Chronic Kidney Disease?
|
5 stages
|
|
|
What is the definition of the first stage of Chronic Kidney Disease?
|
GFR > 90 with renal damage as evident by proteinuria
|
|
|
What is the definition of the second stage of Chronic Kidney Disease?
|
GFR 60 - 89
|
|
|
What is the definition of the third stage of Chronic Kidney Disease?
|
GFR 30-59 (A and B)
|
|
|
What is the definition of the fourth stage of Chronic Kidney Disease?
|
GFR 15-29
|
|
|
What is the definition of the fifth stage of Chronic Kidney Disease?
|
GFR < 15
|
|
|
What are the GFR criteria for the five stages of GFR?
|
1. GFR > 90
2. GFR 60-89 3. GFR 30-59 4. GFR 15-29 5. GFR < 15 |
|
|
Which chronic diseases have increased in prevalence according to medicare beneficiaries?
|
* Chronic Kidney Disease
- Depression - Diabetes Mellitus - Rheumatoid Arthritis and Degenerative Joint Disease |
|
|
Which chronic diseases have decreased in prevalence according to medicare beneficiaries?
|
- Congestive Heart Failure
- Coronary Artery Disease - CVA and TIA |
|
|
Case 1:
- 53 yo male who is establishing care - Not seen a physician for 6 years - Refilling meds through free clinic - Diagnosed w/ T2DM 10 years ago - he was on oral hypoglycemic drugs - Main complaint now is leg swelling and polyuria - Obese, BP 167/102, HR 98 - He has 3+ LE edema bilaterally and symmetrical What is the most likely cause of LE edema? a) Hypertension b) Deep vein thrombosis c) Left ventricular failure d) Kidney disease complications of DM e) Cellulitis Why are other answers wrong? |
Kidney disease complications of DM
- Why not HTN: low that this would cause edema - Why not DVT: symmetric edema unusual, usually asymmetric - Why not LV failure: possible, but if lungs are clear unlikely - Why not cellulitis: rarely symmetrical |
|
|
What is one of the leading causes of nephrotic syndrome? What are the signs of nephrotic syndrome?
|
- Diabetes is a common cause of nephrotic syndrome
Constellation of features: - Proteinuria >3.5 g/24 hr - Hypoalbuminemia - Hyperlipidemia - Edema (caused by volume retention - salt retaining nephrons - and low oncotic pressure caused by hypoalbuminemia) |
|
|
What causes edema in diabetic nephropathy?
|
Caused by volume retention - salt retaining nephrons - and low oncotic pressure caused by hypoalbuminemia
|
|
|
What happens in the body in the fasting state?
|

- Glucose preferentially goes to brain
- Pancreas releases glucagon on liver to stimulate glucose production - Fatty acids from adipose tissue got o liver to make glucose |
|
|
What happens in the body in the prandial state?
|

- Dietary carbohydrate adds to glucose stores
- Glucose goes to brain, liver, and skeletal muscle for use - Pancreas releases insulin which acts on liver, skeletal muscle, and adipose to store glucose |
|
|
Who has a high GFR? Implications?
|
- Patients eating lots of protein or protein shakes
- Pregnant patients - Diabetic patients initially Eventually leads to decreased GFR Damaging to kidney - podocyte hypertrophy - can lead to PROTEINURIA |
|
|
What leads to proteinuria?
|
- Glomerular hyperfiltration
- Podocyte hypertrophy, detachment, and apoptosis - Thickening of glomerular BM and decreased charge - Glomerular endothelial cells reduce glycocalyx / charge, which increases permeability |
|
|
If there is injury to the glomerular hemodynamics, what is the effect?
|
Glomerular hyperfiltration
|
|
|
If there is injury to the glomerular endothelial cells, what is the effect?
|
- Endothelial cell injury
- Diminished endothelial glycocalyx - Altered VEGF signaling |
|
|
If there is injury to the glomerular basement membrane, what is the effect?
|
- Irregular thickening
- Decreased negative charge |
|
|
If there is injury to the podocyte, what is the effect?
|
- Podocytopenia (detachment and apoptosis of podocytes)
- Loss of slit diaphragm integrity - Foot process widening and effacement - Loss of negative charges |
|
|
If there is injury to the proximal tubule, what is the effect?
|
Decreased protein reabsorption
|
|
|
Case 1:
- 53 yo male who is establishing care - Not seen a physician for 6 years - Refilling meds through free clinic - Diagnosed w/ T2DM 10 years ago - he was on oral hypoglycemic drugs - Main complaint now is leg swelling and polyuria - Obese, BP 167/102, HR 98 - He has 3+ LE edema bilaterally and symmetrical On further interview he said that he is get tired and wants to lay down during the day especially after he takes his meds in the morning. His current medications are metformin, clonidine, glyburide, and Lasix. What are the possible cause(s) of his fatigue? a) Hypoglycemia b) Obstructive sleep apnea c) Hypotension d) TIAs |
- Hypoglycemia - a lot of diabetics who take sulfonylureas and insulin
- Hypotension - hypoglycemia can cause osmotic diuresis, leading to volume loss and hypotension |
|
|
What is the mechanism of Metformin? Negative effects?
|
- Works by suppressing hepatic glucose production
- May cause lactic acidosis (rare) |
|
|
What is the mechanism of Thiazolidinediones (glitazones)? Why is it not a first line drug?
|
- Enhances insulin sensitivity
- Liver fibrosis and liver disease - Edema - Weight gain - Fracture risk |
|
|
What are the types of insulin?
|
Number of different types of insulin:
- Short-acting insulin - Intermediate-acting insulin - Glargine - long-acting insulin (maintains glucose over long time) |
|
|
How is glucose taken up?
|
Glucose taken up by GLUT-4
|
|
|
What is the action of central α2 agonists?
|
Inhibits SNS:
- ↓ HR (via β1) → ↓ CO → ↓ BP - ↓ Vascular Tone (via α1) → ↓ Peripheral Resistance → ↓ BP - ↓ Renin (via β1) → ↓ AngII → ↓ Vascular Tone (via α1) → ↓ Peripheral Resistance → ↓ BP |
|
|
What is the mechanism of Clonidine? What other drugs have the same mechanism?
|
Central α2 agonists:
- Clonidine - Guanabenz - α-Methyldopa Stimulates α2-adrenergic receptors in the brain; reduces sympathetic outflow from the brain's vasomotor center; increases vagal tone |
|
|
What are the adverse effects of central α2-agonists?
|
- Na+/H2O retention
- Abrupt discontinuation may cause rebound HTN - Depression - Orthostatic hypotension - Dizziness - Clonidine - anti-cholinergic - Methyldopa - hepatitis, hemolytic anemia (rare) |
|
|
Case 1:
- 53 yo male who is establishing care - Not seen a physician for 6 years - Refilling meds through free clinic - Diagnosed w/ T2DM 10 years ago - he was on oral hypoglycemic drugs - Main complaint now is leg swelling and polyuria - Obese, BP 167/102, HR 98 - He has 3+ LE edema bilaterally and symmetrical What should you do next? a) Blood chemistry (BMP, HbA1C) b) Urine albumin/creatinine ratio c) Lipids profile d) Kidney biopsy |
a) Blood chemistry (BMP, HbA1C)
b) Urine albumin/creatinine ratio c) Lipids profile Very rare that he has anything but diabetic nephropathy, so probably unnecessary |
|
|
What are the actions of stimulation of α1 receptors?
|
- ↑ Intracellular Ca2+ (via Gq)
- Vasoconstriction (↑ TPR and BP) - Mydriasis |
|
|
What are the actions of stimulation of α2 receptors?
|
- ↓ cAMP (via Gi)
- ↓ NE release (autoreceptor activity) |
|
|
What are the actions of stimulation of β1 receptors?
|
- ↑ cAMP (via Gs)
- ↑ HR (tachycardia) - ↑ Myocardial contractility |
|
|
What are the actions of stimulation of β2 receptors?
|
- ↑ cAMP (via Gs)
- Vasodilation (non-innervated β2 → ↓ TPR and ↓ BP) - Bronchodilation |
|
|
What are the actions of stimulation of β3 receptors?
|
- ↑ cAMP (via Gs)
- ↑ Lipolysis |
|
|
What is the normal drop in GFR for a patient with severe diabetes?
|
10
|
|
|
Case 1:
- 53 yo male who is establishing care - Not seen a physician for 6 years - Refilling meds through free clinic - Diagnosed w/ T2DM 10 years ago - he was on oral hypoglycemic drugs - Main complaint now is leg swelling and polyuria - Obese, BP 167/102, HR 98 - He has 3+ LE edema bilaterally and symmetrical What is missing from the treatment regimen? |
ACE-I - helps with hypertension and limits additional kidney damage
|
|
|
If you have a patient with T2DM, what is the first thing you need to assess?
|
HbA1c
|
|
|
What is the first line treatment for a patient with T2DM?
|
- Diabetes education
- Medical nutrition therapy - Physical activity - Metformin |
|
|
What do you need to screen in a patient with T2DM?
|
- Retinal exam
- Urine microalbuminemia - Neuropathy exam - Vascular evaluation |
|
|
What other co-morbidities should you evaluate and treat in a patient with T2DM?
|
- Dyslipidemia
- Hypertension - Obesity - CV disease |
|
|
Case 2:
- 53 yo female w/ fam hx of autosomal dominant polycystic kidney disease (ADPKD) - Told 14 years ago she has polycystic kidney disease but told her it was nothing to worry about - Started to notice blood in urine and has right flank pain - Takes ibuprofen for headache - BP 176/105, HR 72, RR 16, T 37°C What is the most likely cause of her symptoms ? a) Urinary tract infection b) Kidney stones c) Ruptured renal cyst d) Tubal pregnancy e) Renal cell carcinoma f) Diverticulitis |
*Kidney stones and ruptured renal cyst*
- Kidney stones can cause hematuria and pain - Ruptured renal cyst is most common cause of hematuria and pain in patients with ADPKD - UTI: this is not the most likely cause of the hematuria and pain - Tubal pregnancy wouldn't likely cause hematuria - Renal cell carcinoma only if it is persistent hematuria (need to image) |
|
|
What are the most common causes of hematuria and pain in patients with Autosomal Dominant Polycystic Kidney Disease?
|
- Ruptured renal cyst
- Kidney stones |
|
|
What are the renal complications of Autosomal Dominant Polycystic Kidney Disease? How common?
|
- Infection (30-50%)
- Kidney stones (25%) - Hematuria (35-50%) - Renal cell carcinoma is suspected when hematuria is recurrent or persistent |
|
|
What are the genetic characteristics of Polycystic Kidney Disease?
|
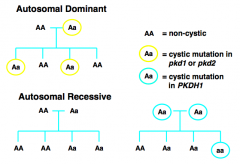
- Autosomal Dominant: cystic mutation in PKD1 (85% of cases, chromosome 16) or PKD2 (15% of cases, chromosome 4)
- Autosomal Recessive: cystic mutation in PKDH1 |
|
|
How would you diagnose Polycystic Kidney Disease?
|
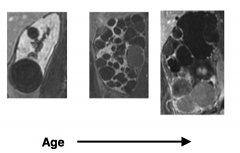
- Imaging (eg, MRI or ultrasound) of cysts in kidneys and other organs
- Family medical history (genetic testing) |
|
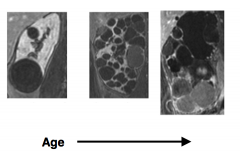
What kind of image is this? What does this show?
|
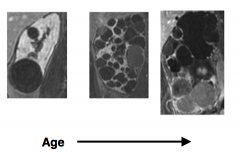
MRI of kidneys
- Polycystic Kidney Disease |
|

What kind of image is this? What does this show?
|

Ultrasound of kidneys
- Polycystic Kidney Disease |
|
|
Case 2:
- 53 yo female w/ fam hx of autosomal dominant polycystic kidney disease (ADPKD) - Told 14 years ago she has polycystic kidney disease but told her it was nothing to worry about - Started to notice blood in urine and has right flank pain - Takes ibuprofen for headache - BP 176/105, HR 72, RR 16, T 37°C No UTI identified, pain resolved after 2 weeks and hematuria also resolved. Blood chemistry also sent. What should you do to advice on ibuprofen use? |
...
|
|
|
Case 2:
- 53 yo female w/ fam hx of autosomal dominant polycystic kidney disease (ADPKD) - Told 14 years ago she has polycystic kidney disease but told her it was nothing to worry about - Started to notice blood in urine and has right flank pain - Takes ibuprofen for headache - BP 176/105, HR 72, RR 16, T 37°C No UTI identified, pain resolved after 2 weeks and hematuria also resolved. Blood chemistry also sent. What should you do about her BP? |
....
|
|
|
What drugs are good for treating patients with non-diabetic nephropathy?
|
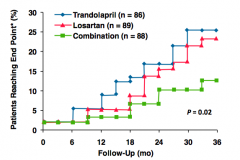
ACE-Is, ARBs, and combination therapy
|
|
|
What diuretic drugs are carbonic anhydrase inhibitors? Location of action?
|
Acetazolamide - acts on proximal tubule
|
|
|
What diuretic drugs are osmotic diuretics? Location of action?
|
Mannitol - acts on proximal tubule
|
|
|
What diuretic drugs are loop diuretics? Location of action?
|
- Furosemide
- Bumetanide - Thick ascending loop |
|
|
What diuretic drugs are thiazide diuretics? Location of action?
|
- Indapamide
- Hydrochlorathiazide - Chlorthalidone - Distal convoluted tubule |
|
|
What diuretic drugs are aldosterone antagonists? Location of action?
|
- Spironolactone
- Distal convoluted tubule |
|
|
What diuretic drugs are K+ sparing diuretics? Location of action?
|
- Triamterene
- Amiodarone - Distal convoluted tubule |
|
|
What is absorbed in the ascending limb of the loop of Henle?
|
- Na+ and Cl- (20-30%), active Cl- reabsorption
- Impermeable to H2O - Can compensate for increased Na+ delivery from proximal tubule by increasing reabsorption |
|
|
What are the characteristics of thiazide and thiazide like diuretics? How effective?
|
- Orally active
- Intermediate efficacy (8-10% of filtered Na+ load excreted) - Moderate onset of activity (60 minutes) - Long duration of action |
|
|
What is the mechanism of Thiazide diuretics?
|
- Filtered and secreted by OAT
- Inhibits Na/Cl symporter - Acts on cortical segment of distal tubule - Increases excretion of Na+, K+, Cl-, and H2O - Urine becomes hypertonic, unable to dilute |
|
|
What are the other actions of Thiazide diuretics not directly related to its use?
|
- Increases K+ secretion
- Enhances urate reabsorption (PT) |
|
|
What are the disadvantages and side effects of Thiazide diuretics?
|
- Hypokalemia
- Alkalosis - Hyperuricemia - Hyperglycemia - Decrease in GFR |
|
|
What are the uses of Thiazide diuretics?
|
- Edema due to CHF
- Hypertension - Hypercalciuria / Ca2+ salt - renal caliculi |
|
|
What are the characteristics of loop diuretics? How effective?
|
- Orally and IV active
- High efficacy (20-30% of filtered Na+ load excreted) - Rapid in onset (20-30 min) - Short duration of action |
|
|
What is the mechanism of Loop diuretics?
|
- Filtered and secreted by OAT
- Inhibits Na/K/2Cl symporter - Acts on cortical and medullary segments of ascending limb of Loop of Henle - Increases excretion of Na+, K+, Cl-, and H2O |
|
|
What are the other actions of Loop diuretics not directly related to its use?
|
- Increases renal blood flow and GFR
- Enhances Ca2+ excretion - Large urine volume |
|
|
What are the disadvantages and side effects of Loop diuretics?
|
- Hypokalemia
- Alkalosis - Hypovolemia - Hyperuricemia (urate reabsorption - PT) - Hyperglycemia - furosemide only - Ototoxicity |
|
|
What are the uses of Loop diuretics?
|
- Edema of cardiac, hepatic, or renal origin
- Acute pulmonary edema - Hypertension |
|
|
Case 2:
- 53 yo female w/ fam hx of autosomal dominant polycystic kidney disease (ADPKD) - Told 14 years ago she has polycystic kidney disease but told her it was nothing to worry about - Started to notice blood in urine and has right flank pain - Takes ibuprofen for headache - BP 176/105, HR 72, RR 16, T 37°C Blood chemistries: - eGFR 18 - Ca2+ 7.1 - Hemoglobin 8.5 - PO4(3-) 7.8 - PTH 328 What is the stage of CKD? |
Stage 4
1. GFR > 90 2. GFR 60-89 3. GFR 30-59 4. GFR 15-29 5. GFR < 15 |
|
|
Case 2:
- 53 yo female w/ fam hx of autosomal dominant polycystic kidney disease (ADPKD) - Told 14 years ago she has polycystic kidney disease but told her it was nothing to worry about - Started to notice blood in urine and has right flank pain - Takes ibuprofen for headache - BP 176/105, HR 72, RR 16, T 37°C Blood chemistries: - eGFR 18 - Ca2+ 7.1 - Hemoglobin 8.5 - PO4(3-) 7.8 - PTH 328 What is the cause of the low Ca2+ and low Hb? |
- Vitamin D is activated in kidney but if kidney function is compromised by cysts she won't be absorbing enough Ca2+, which stimulated her PTH to increase
- Low Hb is because kidney makes erythropoietin - which stimulates erythropoiesis, as kidney fails, EPO drops so not making enough RBCs (not due to hematuria) |
|
|
Case 2:
- 53 yo female w/ fam hx of autosomal dominant polycystic kidney disease (ADPKD) - Told 14 years ago she has polycystic kidney disease but told her it was nothing to worry about - Started to notice blood in urine and has right flank pain - Takes ibuprofen for headache - BP 176/105, HR 72, RR 16, T 37°C Blood chemistries: - eGFR 18 - Ca2+ 7.1 - Hemoglobin 8.5 - PO4(3-) 7.8 - PTH 328 What should you give next ? a) Erythropoietin b) Calcitriol c) Phosphate binders d) All of the above Why do you give the one(s) you give? |
All of the above
- Epo → improve anemia by stimulating erythropoiesis - Calcitriol = 1,25(OH)2 - Vitamin D → will improve Ca2+ absorption - Phosphate binders → excess phosphate can kill chronic kidney disease patients |
|
|
Case 2:
- 53 yo female w/ fam hx of autosomal dominant polycystic kidney disease (ADPKD) - Told 14 years ago she has polycystic kidney disease but told her it was nothing to worry about - Started to notice blood in urine and has right flank pain - Takes ibuprofen for headache - BP 176/105, HR 72, RR 16, T 37°C Blood chemistries: - eGFR 18 - Ca2+ 7.1 - Hemoglobin 8.5 - PO4(3-) 7.8 - PTH 328 Patient calls and says she is enrolled in a clinical trial at Mayo Clinic. 6 months later she was sent to ER after she was found down. EMS shows BP of 85/-, HR 125, w/ dry mucus membranes What is the likely event that caused her symptoms? |
She was most likely in a trial that was testing Tolvaptan (vasopressin receptor 2 antagonist) designed to treat hyponatremia
|
|
|
What is the mechanism of Tolvaptan?
|
- Vasopressin receptor 2 antagonist
- cAMP carries out the signal of V2 receptor - In PKD, cAMP also stimulates cystogenesis and increases the size of cysts - Drug has been shown to reduce cyst growth |
|
|
Why did the Case 2 patient fall to ground and have to go to ED with BP of 85/-, HR 125, and dry mucus membranes when taking Tolvaptan?
|
One of the main complications of Tolvaptan is volume loss
|
|
|
Case 2:
- 53 yo female w/ fam hx of autosomal dominant polycystic kidney disease (ADPKD) - Told 14 years ago she has polycystic kidney disease but told her it was nothing to worry about - Started to notice blood in urine and has right flank pain - Takes ibuprofen for headache Patient calls and says she is enrolled in a clinical trial at Mayo Clinic. 6 months later she was sent to ER after she was found down. EMS shows BP of 85/-, HR 125, w/ dry mucus membranes; she was taking Tolvaptan. What is the most likely chemical changes seen on BMP on first blood draw in ED? |
- Creatinine: increases
- Sodium: increases drastically - BUN: increases |
|
|
Case 2:
- 53 yo female w/ fam hx of autosomal dominant polycystic kidney disease (ADPKD) - Told 14 years ago she has polycystic kidney disease but told her it was nothing to worry about - Started to notice blood in urine and has right flank pain - Takes ibuprofen for headache Patient calls and says she is enrolled in a clinical trial at Mayo Clinic. 6 months later she was sent to ER after she was found down. EMS shows BP of 85/-, HR 125, w/ dry mucus membranes; she was taking Tolvaptan. Patient withdraws from clinical trial. eGFR is stable. Two months later she calls your office and said she has the worst headache of her life. What advice should you give her? a) Take a Tylenol and sleep on it. b) Call 911 or go to the nearest ER. c) Check your blood pressure and if it is OK there is nothing to worry about d) You will likely need to start dialysis soon |
Call 911 or go to the nearest ER
|
|
|
What are the extra-renal complications of Autosomal Dominant Polycystic Kidney Disease? Odds of having each of these?
|
- Intracranial aneurysms (5-7%, up to 12-15% if another family member had one)
- Liver cysts (>85%) - Heart valve disease (25%) - Abdominal wall hernias (45%) |
|
|
What is the likelihood of having an intracranial aneurysm if you have ADPKD?
|
- 5-7% of adults may have brain aneurysm
- 12-15% if another family member had an intracranial aneurysm - This is 5x higher than general population |
|
|
What is the likelihood of having a liver cyst if you have ADPKD?
|
>85% of patients will have liver cysts by age 30
|
|
|
What is the likelihood of having heart valve disease if you have ADPKD? Treatment?
|
25% of patients w/ ADPKD
- Usually requires no treatment but can become severe enough to require valve replacement |
|
|
What is the likelihood of having an abdominal wall hernia if you have ADPKD?
|
45% of patients with ADPKD
|

