![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
79 Cards in this Set
- Front
- Back
|
What is the actual definition of a fever in a neonate or infant?
|
38.0°C or 100.4°F
|
|
|
What is the actual definition of a fever in older kids and adults?
|
Variable:
- "Low grade fever" 100.4-101°F - "Fever" 101-102°F - "High fever" >103°F |
|
|
Why is it important to know if a fever is >100.4°F in a neonate?
|
A fever may be suggestive of a serious bacterial infection, even without other signs of symptoms
|
|
|
What is the gold standard for measuring core body temperature?
a) Oral b) Axillary c) Rectal d) Temporal e) Ear/ Tympanic membrane |
Rectal
|
|
|
What are the characteristics of a rectal temperature?
|
Gold standard for core body temperature
|
|
|
What are the characteristics of an oral temperature?
|
Typically 0.6°C lower than rectal d/t mouth breathing
|
|
|
What are the characteristics of an axillary temperature?
|
Consistently lower than rectal, but variable
|
|
|
What are the characteristics of a temporal temperature?
|
Affected by sweating or vascular changes, contradictory results
|
|
|
What are the characteristics of an infrared tympanic membrane temperature?
|
Insufficient agreement with established methods of core temperature
|
|
|
Case 1:
- 9 day old M is brought to the Emergency Department by his parents for a “fever - The patient’s temperature was taken in the ED and was 101.2° F What else would we like to know about the history? |
- Born at 37 weeks gestation
- Normal spontaneous vaginal delivery - Mom’s prenatal labs were negative - Mom had a fever and flu-like illness a few days prior to delivery - Normal nursery course, discharged home with mom on day of life 2 - Breast feeding well until today - Fussier for the past 2 days - Spit up after each feed, but only a little bit - 8-10 wet diapers/day - 6-8 poopy diapers/day, yellow and seedy (normal) |
|
|
Case 1:
- 9 day old in ED with fever of 101.2°F - Born at 37 weeks gestation, normal spontaneous vaginal delivery - Mom had a fever and flu-like illness a few days prior to delivery - Fussier in last 2 days, spit up after each feed - 8-10 wet diapers/day, 6-8 poopy diapers/day, yellow and seedy (normal) Exam abnormalities: - Anterior fontanelle slightly bulging - Cool hands and feed, capillary refill ~3-4 seconds What is on the differential diagnosis? |
- Meningitis
- Inborn errors of metabolism (eg, phenylketonuria) - Viral infection |
|
|
Case 1:
- 9 day old in ED with fever of 101.2°F - Anterior fontanelle slightly bulging - Cool hands and feed, capillary refill ~3-4 seconds What is the best next step? a) Reassurance and discharge home with close follow up b) No further tests, but admit to the hospital for observation c) Check blood, urine and CSF cultures but do not start antibiotics unless cultures positive d) Check blood, urine and CSF culture and start empiric antibiotics pending culture results e) Perform a whole body MRI scan, then investigate the patient’s home for environmental toxins |
Check blood, urine and CSF culture and start empiric antibiotics pending culture results
- Because they are only 9 days old you are acting more aggressively |
|
|
Case 1:
- 9 day old in ED with fever of 101.2°F - Anterior fontanelle slightly bulging - Cool hands and feed, capillary refill ~3-4 seconds For this infant, what lab tests do you need to do? |
- Blood culture
- Urinalysis and urine culture: UA negative for nitrites and leukocyte esterases, 0 WBC (normal) - CSF cell count, glucose, protein, and culture: pleiocytosis w/ monocyte predominance, low glucose, and elevated protein |
|
|
Case 1:
- 9 day old in ED with fever of 101.2°F - Anterior fontanelle slightly bulging - Cool hands and feed, capillary refill ~3-4 seconds CSF cell count, glucose, protein, and culture: pleiocytosis w/ monocyte predominance, low glucose, and elevated protein What does this make you think? |
Bacterial meningitis
- Low glucose: bacteria are eating glucose - High protein: inflammatory response - Usually bacteria have a neutrophil predominance (more on this later) |
|
|
Case 1:
- 9 day old in ED with fever of 101.2°F - Anterior fontanelle slightly bulging - Cool hands and feed, capillary refill ~3-4 seconds - CSF cell count, glucose, protein, and culture: pleiocytosis w/ monocyte predominance, low glucose, and elevated protein How do you choose what antibiotics to use? |
- Depends on what organisms are likely to be causing the infection
- In neonates, the most common organisms that cause meningitis are: Group B streptococcus, E. coli, and Listeria monocytogenes |
|
|
What are the most common causes of meningitis in neonates?
|
1. Group B streptococcus
2. Escherichia coli 3. Listeria monocytogenes |
|
|
How do you identify Group B Strep?
|
- G+ diplococci
- Lancefield group B - β-hemolytic on blood agar |
|
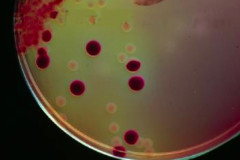
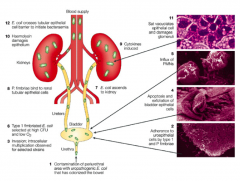
What is this bug? Signs?
|
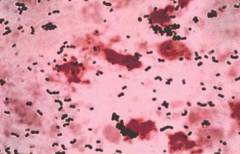
Group B Strep
- G+ diplococci - Lancefield group B - β-hemolytic on blood agar |
|
|
What are the virulence factors of Group B Strep?
|
- Capsular polysaccharides
- Direct cytotoxicity to host phagocytes |
|
|
What are the signs of Group B Strep in a neonate?
|
Bacteremia without a focus, sepsis, pneumonia and/or meningitis
|
|
|
How do you identify E. coli?
|
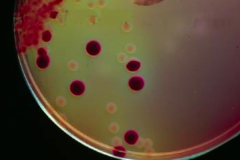
- G- rods
- Mostly lactose fermenting (pink colonies on MacConkey agar) |
|
What is this bug? Signs?
|
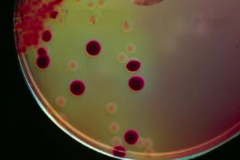
E. coli
- G- rods - Mostly lactose fermenting (pink colonies on MacConkey agar) |
|
|
What are the signs of E. coli in a neonate?
|
UTI, sepsis, and/or meningitis
|
|
|
What are the signs of E. coli in an older child?
|
Mostly UTI and GI illness
|
|
|
How do you identify Listeria?
|
- G+ rod, singly or in short chains
- Aerobic and facultatively anaerobic - β-hemolytic on blood agar - Characteristic TUMBLING MOTILITY by light microscopy |
|
|
What is Listeriosis most common? Symptoms?
|
3rd trimester of pregnancy - flu-like illness
- Can cause fetal death, premature birth, sepsis, meningoencephalitis - Can cause gastroenteritis if ingested |
|
|
What are the common drugs used to treat neonatal meningitis?
|
Ampicillin and Cefotaxime +/- Gentamicin
|
|
|
Cefotaxime is in which drug class/subclass?
|
3rd generation cephalosporin
|
|
|
Which drug used for neonatal meningitis covers Listeria?
|
Ampicillin +/- Gentamicin
|
|
|
Which drug used for neonatal meningitis covers E. coli?
|
Cefotaxime, Gentamicin
- Resistance to Ampicillin is common |
|
|
Which drug used for neonatal meningitis covers Group B Streptococci?
|
Ampicillin, Cefotaxime (+/- Gentamicin)
|
|
|
Among cefotaxime, gentamicin, and ampicillin, which are time-dependent killers?
a) Ampicillin b) Cefotaxime c) Gentamicin d) A and B e) A and C f) B and C g) All of the above |

Ampicillin and Cefotaxime
|
|
|
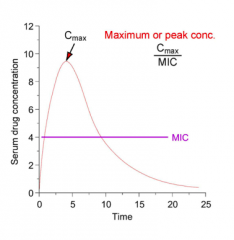
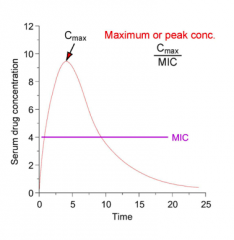
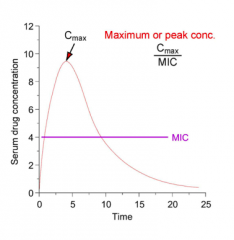
What are the characteristics of Time-Dependent Killing?
|

- Maximize the duration of effective concentration
- These drugs work best when concentration exceeds 4x the MIC for >50% of the time |
|
|
Which antibiotics have time-dependent killing?
|

β-lactams
- Penicillins - Cephalosporins - Monobactams |
|
|
What are the resistance mechanisms to β-lactam drugs?
|
- β-lactamase production
- Alterations in penicillin binding protein (PBP) - Permeability barrier in certain G- bacilli |
|
|
What are the characteristics of β-lactamase production?
|
- Other than Staph, β-lactamase not associated with most G+
- 3rd generation (and some 2nd generation) cephalosporins are not degraded by some common G- β-lactamases |
|
|
Among cefotaxime, gentamicin, and ampicillin, which exhibit a post-antibiotic effect?
a) Cefotaxime b) Gentamicin c) Ampicillin d) None of the above |
Gentamicin (aminoglycosides)
|
|
|
What is the post-antibiotic effect?
|
Sustained activity for several hours after aminoglycoside concentration has dropped below effective levels
|
|
|
What are the benefits of the post-antibiotic effect?
|
Less frequent dosing
|
|
|
Which best describes the killing of gentamicin?
a) Time-dependent killing b) Concentration-dependent killing c) Area under the curve-dependent killing |
Concentration-dependent killing
|
|
|
What are the characteristics of Concentration-Dependent Killing?
|
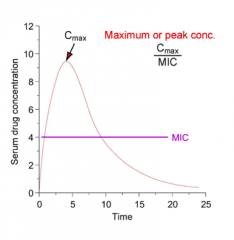
- Maximize the peak concentration (Cmax)
- Cmax/MIC ratio ≥ 8 is best |
|
Which antibiotics have concentration-dependent killing?
|
Aminoglycosides
- Gentamicin - Tobramycin - Amikacin - Have persistent effect even when levels fall below MIC |
|
|
What is the mechanism of Aminoglycosides (Gentamicin, Tobramycin, Amikacin)?
|
• Bind 30S ribosome at several sites → inhibition of protein synthesis
- Stops initiation, causes mRNA misreading • Bactericidal against susceptible aerobic gram-negative bacilli - Potential for synergism with gram-neg. and gram-pos. bacteria |
|
|
What are the resistance mechanisms against Aminoglycosides (Gentamicin, Tobramycin, Amikacin)?
|
Not common:
• Inactivating enzymes (most common, transmissable) • Decreased import, increased efflux systems (rare) • Ribosomal modifications (rare) • There are some strains that are highly resistant to gentamicin and/or tobramycin |
|
|
What are the side effects of Gentamicin?
a) Ototoxicity b) Nephrotoxicity c) Hepatotoxicity d) A and B e) All of the above |
Ototoxicity and Nephrotoxicity
|
|
|
Case 1:
- 9 day old in ED with fever of 101.2°F - Anterior fontanelle slightly bulging - Cool hands and feed, capillary refill ~3-4 seconds - CSF cell count, glucose, protein, and culture: pleiocytosis w/ monocyte predominance, low glucose, and elevated protein - Patient started on Cefotaxime and Ampicillin and admitted to hospital - Within 8 hours, blood and CSF cultures started growing Listeria monocytogenes What question do you wish you had asked mom now? |
If she has been exposed to unpasteurized milk (in fact she works on a dairy farm and indulged in Queso Fresco during pregnancy)
|
|
|
Case 1:
- 9 day old in ED with fever of 101.2°F - Anterior fontanelle slightly bulging - Cool hands and feed, capillary refill ~3-4 seconds - CSF cell count, glucose, protein, and culture: pleiocytosis w/ monocyte predominance, low glucose, and elevated protein - Patient started on Cefotaxime and Ampicillin and admitted to hospital - Within 8 hours, blood and CSF cultures started growing Listeria monocytogenes Now that you have established the causative organism, how should their treatment be changed? |
Patient should be treated with Ampicillin for 21 days as well as with Gentamicin (for potential synergy) for 14 days
- This will only be synergistic if this Listeria strain has some sensitivity to gentamicin on its own; gentamicin will not target intracellular forms but ampicillin will |
|
|
Case 1:
- 9 day old in ED with fever of 101.2°F - Anterior fontanelle slightly bulging - Cool hands and feed, capillary refill ~3-4 seconds If this was a G- meningitis and you gave the infant a combination of Cefotaxime + Ampicillin, what type of β-lactamase might you be particularly worried about? |
- AmpC β-lactamases (can be strongly induced by ampicillin and can degrade many cephalosporins, including cefotaxime; found in some G-, including E. coli)
- Extended spectrum β-lactamases (render G- resistant to essentially all penicillins and cephalosporins, associated with some strains of Klebsiella and E. coli, some are transmissible) |
|
|
Case 2:
- 16 yo F presents to ER w/ fever of 1 day, Tmax = 103.5°F (axilary) - Sharp pain R side of lower back (6/10) - Tylenol improved pain and fever - Pain / burning w/ urination, decreased frequency + urgency and hesitancy - Nausea and vomiting today - Decreased PO intake of food and fluids since yesterday - Unable to go to HS today d/t fever and nausea PMH: intermittent asthma, Albuterol as needed, symptoms w/ exercise - Treated for Chlamydia 1y ago - Tonsillectomy and adenoidectomy at age 6 Meds: - Oral contraceptive pills Allergies: - Hives and difficulty breathing (required tx in ER) when given Amoxicillin for an ear infection when she was younger Fam Hx: mom (46) and dad (48) healthy, brother (10) has asthma Social Hx: denies drugs & alcohol, sexually active w/ 1 partner, 3 lifetime partners, condoms "most of the time" Exam abnormalities: - 103°F, HR 120 bpm, moderate distress, mucus membranes dry, tenderness in suprapubic region Problem List? |
• Fever
• Back pain • Dysuria • Changes in urinary frequency • Urinary urgency and hesitancy • High risk sexual activity (hx of UTI, non-consistent w/ condoms, multiple partners) • Tachycardia • Dehydration • Suprapubic pain • CVA tenderness |
|
|
Case 2:
• 16 yo F presents to ER w/ fever of 1 day, Tmax = 103.5°F (axilary) • Fever • Back pain • Dysuria • Changes in urinary frequency • Urinary urgency and hesitancy • High risk sexual activity (hx of UTI, non-consistent w/ condoms, multiple partners) • Tachycardia • Dehydration • Suprapubic pain • CVA tenderness Differential diagnosis? |
More likely
- Pyelonephritis (kidney infection) = most likely - STI / Urethritis → PID - Cystitis (bladder infection) Less likely - Appendicitis - Nephrolithiasis (kidney stone) or Ureterolithiasis |
|
|
Case 2:
• 16 yo F presents to ER w/ fever of 1 day, Tmax = 103.5°F (axillary) Based on this differential, what tests do you want to order? Why? - Pyelonephritis (kidney infection) - STI / Urethritis → PID - Cystitis (bladder infection) - Appendicitis - Nephrolithiasis (kidney stone) or Ureterolithiasis |
- Urinalysis (look for blood or WBCs)
- Urine culture (takes a while) - Urine gonorrhea and chlamydia test (high risk factors) - CBC with differential (gauge how high WBC is) - Basic Metabolic Panel - Blood culture (check for bacteremia if you suspect pyelonephritis) - β-hCG (check for pregnancy, if you treat patient you don't want tx to be contraindicated) |
|
|
Case 2:
RESULTS • 16 yo F presents to ER w/ fever of 1 day, Tmax = 103.5°F (axilary) • Fever • Back pain • Dysuria • Changes in urinary frequency • Urinary urgency and hesitancy • High risk sexual activity (hx of UTI, non-consistent w/ condoms, multiple partners) • Tachycardia • Dehydration • Suprapubic pain • CVA tenderness Labs: • WBC 14,000 (80% neutrophils) • Hgb 12.5 • Platelets 450,000 • BUN 20 mg/dL • Creatinine: 1.5 mg/dL (elevated) Urinalysis: • + leukocyte esterase • + nitrite • 1+ protein • 2-5 RBCs/hpf • 25 WBC/hpf (anything >5 = inflammation) |
Case 2:
• 16 yo F presents to ER w/ fever of 1 day, Tmax = 103.5°F (axilary) • Fever • Back pain • Dysuria • Changes in urinary frequency • Urinary urgency and hesitancy • High risk sexual activity (hx of UTI, non-consistent w/ condoms, multiple partners) • Tachycardia • Dehydration • Suprapubic pain • CVA tenderness Labs: • WBC 14,000 (80% neutrophils) • Hgb 12.5 • Platelets 450,000 • BUN 20 mg/dL • Creatinine: 1.5 mg/dL (elevated) Urinalysis: • + leukocyte esterase • + nitrite • 1+ protein • 2-5 RBCs/hpf • 25 WBC/hpf (anything >5 = inflammation) |
|
|
Why do you check for leukocyte esterase in urinalysis?
|
Marker of WBCs / inflammation
|
|
|
Why do you check for nitrites in urinalysis?
|
Marker of G- rods
- Primarily enterobacteriaceae - Only a minority of Pseudomonas are nitrite + - Other non-fermentatives are often nitrite - (Not very sensitive ~50-55%) |
|
|
What is "sensitivity"? How do you calculate?
|
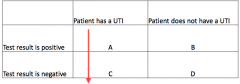
Probability that a sick patient will have a positive test result
Sensitivity = A / (A + C) |
|
|
What is "specificity"? How do you calculate?
|
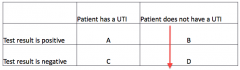
Probability that a healthy patient will have a negative result
Specificity = B / (B + D) |
|
|
What are tests with high sensitivity used for? High specificity?
|
- High sensitivity: rule out diagnosis
- High specificity: rule in diagnosis |
|
|
Is leukocyte esterase more sensitive/specific? Implications?
|
More sensitive than it is specific (high rate of false positives)
|
|
|
Is nitrite test more sensitive/specific? Implications?
|
Specific but not very sensitive (high rate of false negatives)
|
|
|
What are the typical findings for a diagnosis of Pyelonephritis?
|
- Fever
- Flank pain - CVA tenderness - Nausea - Vomiting |
|
|
What are the typical findings for a diagnosis of Cystitis?
|
- Dysuria
- Frequency - Urgency - Suprapubic pain - Hematuria |
|
|
What are the typical findings for a diagnosis of Urethritis and Vaginitis?
|
- Dysuria
- Discharge - Pruritus - Dyspareunia - No frequency or urgency |
|
|
What is the most common bacterial pathogen to cause pyelonephritis?
a) Neisseria gonorrhoeae b) Staphylococcus aureus c) Chlamydia d) Enterobacter cloacae e) Escherichia coli |
E. coli
|
|
|
What are the most common causes of UTI?
|
• Serratia marcescens
• Staphylococcus saphrophyticus • Escherichia coli • Enterobacter cloacae • Klebsiella pneumoniae • Proteus mirabilis • Pseudomonas aeruginosa |
|
|
Why is E. coli good at colonizing the urinary tract?
|
(2) Adheres to uroepithelial cells by type 1 and P fimbriae
|
|
|
Case 2:
- Diagnose her with pyelonephritis What would be the safest and most effective IV antibiotic to use for tx in this patient? |
Ciprofloxacin
- Another treatment for pyelonephritis is Ampicillin but she has a history of allergic reaction to Amoxicillin |
|
|
What are the treatment choices for Pyelonephritis?
|
IV antibiotics
- Ampicillin - Ciprofloxacin - Cephalosporins (3rd generation) Alternatives: - Aztreonam (Monobactam) - Aminoglycosides (eg, Gentamicin and Tobramycin - but concern for nephrotoxicity or ototoxicity) |
|
|
What are the concerns for treating Pyelonephritis with IV Ampicillin?
|
- Check for allergies
- β-lactamase is quite common in E. coli and other Enterobacteriaceae |
|
|
What are the concerns for treating Pyelonephritis with IV Ciprofloxacin (fluoroquinolone)?
|
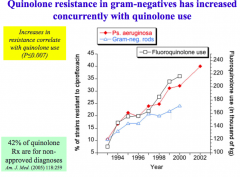
- Nationally, resistance among G- is 20-30%
- But there are no allergic cross-reactions with β-lactams |
|
|
What are the general properties of β-lactams as a group?
|
- Bactericidal (rapid)
- Irreversible / competitive inhibitors of PBPs (Penicillin-Binding Proteins; Transpeptidases) - prevents cell wall cross-linking - Excretion: usually renal, glomerular filtration and anion secretion |
|
|
In a patient with a history of Penicillin allergies, what are the implications for the safety of taking Cephalosporins?
|
Cross-allergies between Penicillins and Cephalosporins are <1 to >10% (typically at lower end)
- Depends on whether allergic to CORE structure or SIDE GROUPS - Shared side chains are associated with increased likelihood of allergic cross-reaction - Amoxicillin and Ceftriaxone do not share common side chains - but does not mean the risk is zero |
|
|
Case 2:
- Diagnose her with pyelonephritis What are other IV alternatives if we want to avoid β-lactam allergy issues? |
- Quinolones (eg, Ciprofloxacin)
- Aztreonam (monobactam - no cross-allergies) - Aminoglycosides (eg, gentamicin and tobramycin) but concern for nephrotoxicity and ototoxicity |
|
|
Case 2:
- Diagnose her with pyelonephritis What are other ORAL alternatives? |
- Ciprofloxacin
- Bactrim (Trimethoprim / Sulfamethoxazole) |
|
|
What are the most commonly used drugs for fever?
|
- NSAIDs: oral ibuprofen or IV ketorolac
- Acetaminophen |
|
|
What would be the best medication in this specific case to treat both pain and fever?
a) Ibuprofen b) Acetaminophen c) Naproxen d) Morphine e) Ketorolac |
Acetaminophen will treat fever and pain
Want to avoid NSAIDs because she already has some kidney damage |
|
|
Case 2:
- Diagnose her with pyelonephritis Why avoid NSAIDs in this patient? Alternative? |
• Elevated creatinine
• Can block production of vasodilatory prostaglandins, thereby decreasing renal blood flow and GFR • Presumed impaired excretion during acute infection • Can use acetaminophen instead |
|
|
Case 2:
- What if the urine culture had instead indicated that this E. coli was categorized as ESBL (extended-spectrum β-lactamase) Would ceftriaxone likely work? |
No. Extended spectrum b-lactamases often render bacteria resistant to most/all penicillins, cephalosporins, and aztreonam.
|
|
|
Case 2:
- What if the urine culture had instead indicated that this E. coli was categorized as ESBL (extended-spectrum β-lactamase) Would Ciprofloxacin likely work? |
Depends. ESBL strains often harbor resistance to several other drug classes as well. High concentration of quinolones in urine are of potential benefit here.
|
|
|
Case 2:
- What if the urine culture had instead indicated that this E. coli was categorized as ESBL (extended-spectrum β-lactamase) What is typically recognized as an effective treatment for ESBL E. coli? |
• Carbapenems (e.g. imipenem/cilastatin, meropenem, ertapenem, etc.)
• However, there are penicillin cross-allergies |

