![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
66 Cards in this Set
- Front
- Back
|
Case 1:
- 48 yo woman presents to PCP w/ 6 month history of weakness, fatigue, and weight loss - Otherwise she appears healthy and has no other major complaints What diagnoses MUST you consider? |
- Hyperthyroidism
- Adrenal insufficiency - Primary hyperparathyroidism |
|
|
What is the feedback look for the thyroid hormones?
|

- TRH from hypothalamus stimulates TSH from anterior pituitary
- TSH stimulates T3 and T4 release from thyroid gland - T3 and T4 have negative feedback on TSH in anterior pituitary - T3 also has negative feedback on TRH in hypothalamus |
|
|
What are the types of hyperthyroidism?
|
- Primary: increased free T4, suppressed TSH
- Secondary: increased free T4, inappropriately not suppressed TSH |
|
|
What is the most common cause of hyperthyroidism?
|
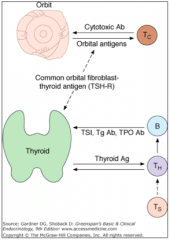
Graves Disease
- Autoantibodies (IgG) stimulate TSH receptors on thyroid (Thyroglobulin/Tg Ab and Thyroid Peroxidase/TPO Ab) - Stimulates thyroid to release T4 and T3 |
|
|
What are the symptoms of hyperthyroidism?
|
1. Alertness, emotional lability, nervousness, irritability
2. Poor concentration *3. Muscular weakness, fatigability 4. Palpitations *5. Voracious appetite, weight loss 6. Increased frequency of bowel movements 7. Heat intolerance |
|
|
What are the signs of hyperthyroidism?
|
1. Hyperkinesia, rapid speech
*2. Proximal muscle weakness, fine tremor 3. Fine, moist skin; fine, abundant hair; onycholysis (separation of the nail from its bed); pretibial skin thickening 4. Lid lag, stare, chemosis, periorbital edema, proptosis 5. Accentuated first heart sound, tachycardia, atrial fibrillation, widened pulse pressure, dyspnea |
|
|
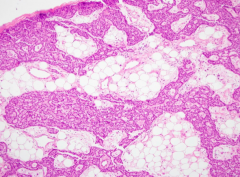
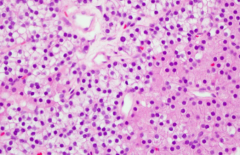
What does a normal thyroid look like histologically?
|

***
|
|
|
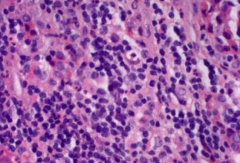
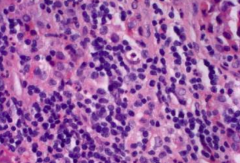
What does a thyroid look like in a patient with Graves Disease?
|
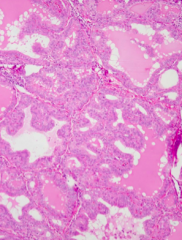
- Irregular follicles
- Scalloped colloid - Diffuse involvement (auto-immune) |
|
|
Although the patient has weight loss, she reports a decrease in her appetite.Rhetorical question: Is Graves likely? Which laboratory test would you order FIRST to rule out Graves’ disease?
a) Serum free T3 b) Serum thyroid binding globulin c) Serum thyroglobulin d) Serum TSH e) Serum total T3 |
Serum TSH
TSH is the screening test used for almost all thyroid disorders! |
|
|
Case 1:
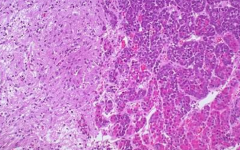
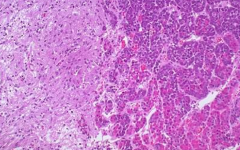
- 48 yo woman presents to PCP w/ 6 month history of weakness, fatigue, and weight loss - Otherwise she appears healthy and has no other major complaints - Patient's serum TSH is within the reference range. Serum lab studies show that the patient has autoantibodies. What is the most likely diagnosis based on the following picture of a thyroid resection? a) Graves disease b) Riedel thyroiditis c) Hashimoto thyroiditis d) Follicular adenoma e) Papillary carcinoma |
*Hashimoto Thyroiditis*
Graves - would have had scalloped borders Hashimoto is the only other one with auto-immune (early on can be hyperthyroid) |
|
|
What happens in the HPA axis?
|
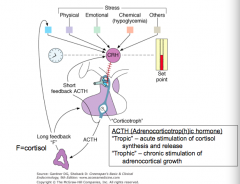
- CRH in hypothalamus stimulates ACTH in anterior pituitary
- ACTH stimulates adrenal gland to release cortisol - Cortisol inhibits both CRH and ACTH - ACTH inhibits CRH too |
|
|
What is the difference between "tropic" and "trophic"?
|
- Tropic: acute stimulation of cortisol synthesis and release
- Trophic: chronic stimulation of adrenocortical growth |
|
|
How do ACTH and cortisol change with the Circadian rhythm?
|
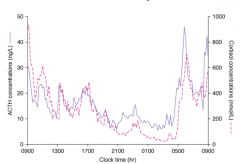
- Both peak early in the morning ~5 AM
- Stays high for a few hours - Drops down for the rest of the day and lowest while sleeping |
|
|
What can cause primary adrenal insufficiency?
|
Destruction (usually irreversible) of adrenal cortex
- Auto-immune - Tuberculosis - Adrenal hemorrhage - Etc |
|
|
What are the levels of hormones in primary adrenal insufficiency?
|

- Cortisol low
- ACTH high (loss of negative feedback) - Aldosterone low - Renin high (loss of negative feedback) |
|
|
What can cause secondary adrenal insufficiency?
|
Chronically inadequate ACTH secretion, resulting in loss of adrenocortical volume = adrenal atrophy
|
|
|
What are the levels of hormones in secondary adrenal insufficiency?
|

- Cortisol low
- ACTH inapproprilately not increased - Aldosterone and renin usually unaffected |
|
|
What are the signs and symptoms of adrenal insufficiency?
|
- Fatigue, malaise, lack of energy
- GI: nausea, vomiting, anorexia → weight loss - Hypotension → dizziness, orthostasis - Increased skin pigmentation, salt craving (primary) |
|
|
What are the layers of the adrenal cortex? What hormones are made there?
|
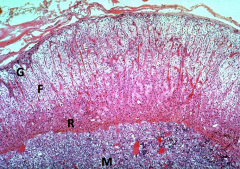
- Zona Glomerulosa (G): mineralocorticoids (aldosterone)
- Zona Fasciculata (F): glucocorticoids (cortisol) - Zona Reticularis (R): sex steroids (estrogens and androgens) |
|
|
What kinds of cells are found in the adrenal medulla? What hormones are made there?
|
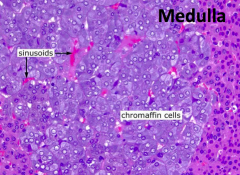
Chromaffin cells: catecholamines (epinephrine)
|
|
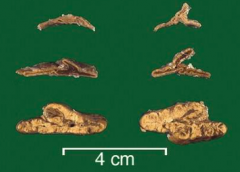
What is the difference between these different adrenal glands?
|
- Top: atrophy (eg, Addison disease, long term corticosteroid use)
- Middle: normal - Bottom: hyperplastic (eg, increased ACTH with ectopic production either from neoplasm - small cell lung carcinoma or pituitary adenoma --> Cushings) |
|
What kind of tissue is on left? Right?
|
- Left: Posterior Pituitary
- Right: Anterior Pituitary |
|
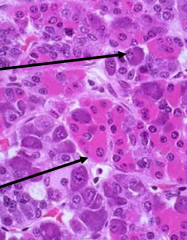
What do these arrows point out in the anterior pituitary?
|
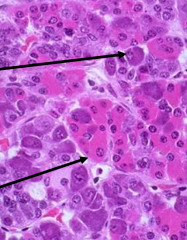
- Top arrow: basophil (bluer)
- Bottom arrow: acidophil (pinker) |
|
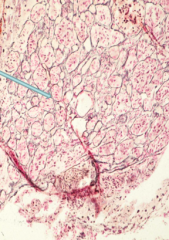
What does this image show?
|
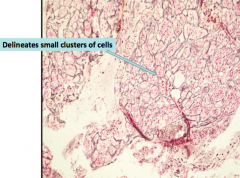
Normal anterior pituitary gland architecture (reticulin stain)
|
|
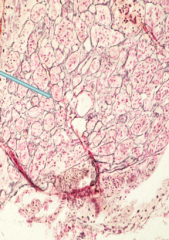
How would this histology of the anterior pituitary be different in a patient with a pituitary adenoma?
|
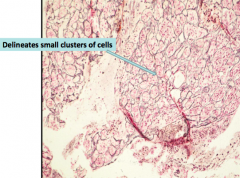
The reticulin meshwork would be lost as there would be larger clusters of cells
|
|
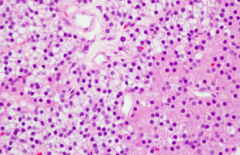
What does this image show?
|
Lymphocytic Hypophysitis (primary hypophysitis)
- Auto-immune disorder classically affecting young women during late pregnancy or in early postpartum period, mimics adenoma, and shows sheets of cytologically bland pure lymphocytic infiltrates |
|
|
Case 1:
- 48 yo woman presents to PCP w/ 6 month history of weakness, fatigue, and weight loss - Otherwise she appears healthy and has no other major complaints Which screening test would you do to rule out adrenal insufficiency of any etiology in an ambulatory patient? a) Cosyntropin (ACTH) stimulation test b) Plasma renin activity and aldosterone c) Late-night salivary cortisol d) Anti-adrenal antibodies e) Plasma ACTH at 8AM |
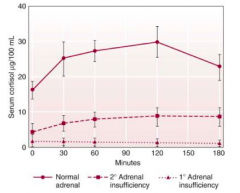
Cosyntropin (ACTH) stimulation test
If you have any suspicion of adrenal insufficiency in a patient, you should do this test! |
|
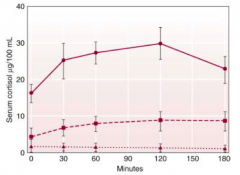
These are the results for different patients to a Cosytropin (ACTH) stimulation test. What do the different lines represent?
|
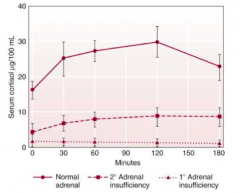
- Dark upper line: normal adrenal (serum cortisol should be elevated in response to ACTH)
- Middle dashed line: 2° adrenal insufficiency - Bottom dotted line: 1° adrenal insufficiency (adrenal gland is unable to respond to increased ACTH) |
|
|
Which of the following is NEVER associated with adrenal cortical atrophy?
a) Sheehan syndrome b) Pituitary prolactinoma c) Exogenous steroids d) Congenital adrenal hyperplasia e) Addison disease |
Congenital adrenal hyperplasia
|
|
|
Case 1:
- 48 yo woman presents to PCP w/ 6 month history of weakness, fatigue, and weight loss - Otherwise she appears healthy and has no other major complaints - Fasting serum glucose is within reference range Following serum results: - Total Ca2+: 10.9 (8.5-10.3) - Phosphorus: 2.9 (2.6-4.5) - Creatinine: 1.0 (0.6-1.1) - Albumin: 3.4 (3.4-5.0) What other diagnosis should we consider to explain her symptoms? |
Primary hyperparathyroidism
|
|
|
Where is calcium absorbed in GI? How much is absorbed?
|
- 20-70% (highest in children)
- 90% absorbed in duodenum and jejunum |
|
|
How is Ca2+ absorbed in GI?
|
- Energy-mediated process regulated by 1,25-(OH)2-D
- Passive diffusional paracellular process |
|
|
Which form of Vitamin D is in plants?
|
Vitamin D2 = Ergocalciferol
|
|
|
Which form of Vitamin D is in animals?
|
Vitamin D3 = Cholecalciferol
|
|
|
Which from of Vitamin D is made in the skin?
|
Vitamin D3 = Cholecalciferol
|
|
|
How does Vitamin D get modified?
|
- Hydroxylated to 25(OH)D in liver in unregulated step
- 1-Hydroxylated to 1,25(OH)2-D in highly regulated step stimulated by PTH in kidney - 24 hydroxylase deactivates 25-D |
|
|
How does PTH affect Vitamin D?
|
PTH stimulates the hydroxylation in kidney of 25(OH)D to 1,25(OH)2-D
|
|
|
What are the symptoms of hypercalcemia?
|
*Fatigue, weakness
*Anorexia *Dehydration - Nausea, vomiting, constipation - Polyuria, polydipsia - Memory impairment - Drowsiness, confusion, coma *Most ambulatory patients have no clear symptoms |
|
|
What happens in kidneys in response to excess calcium?
|
- Renal salt and water loss
- ECF volume contraction |
|
|
What causes primary hyperparathyroidism?
|
Hypercalcemia caused by an INCREASE in PTH secretion (usually d/t parathyroid adenoma)
|
|
|
How does hypercalcemia affect PTH?
|
Hypercalcemia (d/t vitamin D intoxication or d/t malignancy) suppresses PTH secretion
|
|
|
What are the findings of primary hyperparathyroidism?
|
- Hypercalcemia
- Serum PTH inappropriately not suppressed - Can have hypOphosphatemia) - High normal or increased calcium excretion |
|
|
What is the most common cause of primary hyperparathyroidism?
|
Parathyroid Adenoma: MEN1 or MEN2A
|
|
|
What are the types of neoplasias in MEN1?
|
- Parathyroid
- Pituitary - Pancreatic islet |
|
|
What are the types of neoplasias in MEN2A?
|
- Parathyroid
- Pheochromocytoma - Medullary carcinoma of thyroid |
|
|
What are the types of neoplasias in MEN2B?
|
- Medullary carcinoma of thyroid
- Pheochromocytoma - Neuromas, ganglioneuromas |
|
|
What can cause PTH-independent hypercalcemia?
|
Malignancy:
- Bone metastases - PTH-related protein - Osteoclast activating factors - Unregulated calcitriol (1,25(OH)2-D) production - True ectopic PTH (very rare) |
|
|
What is calcitriol?
|
Synonym for 1,25(OH)2-D
|
|
|
You do addition blood testing and find the following results:
- Serum 1,25(OH)2D = 75 pg/ml (15-70) - Serum 25(OH)D = 24 ng/ml (20-60) - Serum PTH = 60 pg/ml (10-65) - 24 hr Urinary calcium 260 mg/24 hours (90-250) What is your diagnosis? a) Vitamin D intoxication b) Tuberculosis-mediated expression of 1-hydroxylase c) Primary hyperparathyroidism d) Secondary hyperparathyroidism e) Hypercalcemia of malignancy |
Primary Hyperparathyroidism
- High calcium because excreting excess Ca2+ in urine - Inappropriately elevated PTH (should be decreased) |
|
|
Case 1:
- 48 yo woman presents to PCP w/ 6 month history of weakness, fatigue, and weight loss - Otherwise she appears healthy and has no other major complaints - Fasting serum glucose is within reference range Following serum results: - Total Ca2+: 10.9 (8.5-10.3) - Phosphorus: 2.9 (2.6-4.5) - Creatinine: 1.0 (0.6-1.1) - Albumin: 3.4 (3.4-5.0) Outcome? |
Solitary parathyroid adenoma is removed and patient's hypercalcemia and symptoms resolve over next few weeks to months
|
|
|
What is the normal appearance of a parathyroid gland?
|
- Yellow, brown ovoid nodule
- 30-45 mg - Large amounts of intervening stromal fat (30-70%) |
|
|
What kinds of cells are in a normal parathyroid gland?
|
- Chief cells: secrete PTH
- Oxyphil cells |
|
|
Which cells secrete PTH
|
Chief cells of parathyroid
|
|
What does this histologic image show?
|
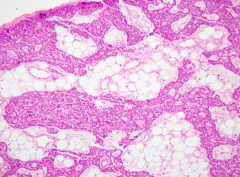
Normal parathyroid gland
- Chief cells and some oxyphil cells - Large amount of intervening stromal fat (30-70%) |
|
What kinds of cells are lighter on left? Darker on right?
|
- Left: Chief cells (make PTH)
- Right: Oxyphilic cells |
|
|
What are the gross and histologic characteristics of a Parathyroid Adenoma?
|
- Solitary nodule arising in a single parathyroid gland (0.5-5 g)
- Other glands are either normal or atrophic - Composed of sheets of chief cells with decreased stromal fat - Oxyphil cells may also be present - May show a rim of normal parathyroid at periphery |
|
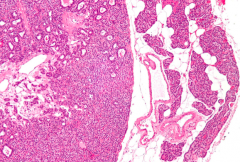
What does this histologic image show?
|
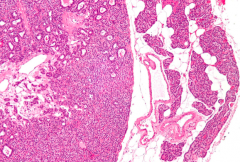
Parathyroid Adenoma
- Composed of sheets of chief cells with decreased stromal fat - Oxyphil cells may also be present - Rim of normal parathyroid at periphery (with interspersed fat) |
|
|
How do you rule out Graves' Disease?
|
Measure suppressed serum TSH (increased negative feedback inhibition of pituitary thyrotrophs)
|
|
|
How do Hashimoto thyroiditis and Graves disease compare histologically?
|
- Hashimoto's: lymphocytic infiltration
- Graves': irregular follicular borders and scalloped colloid |
|
|
How do you rule out Adrenal Insufficiency?
|
ACTH-stimulation test
|
|
|
How will the adrenals be affected in primary adrenal insufficiency vs secondary?
|
- Primary: adrenal destroyed
- Secondary: atrophied |
|
|
What can cause adrenal insufficiency (atrophy of adrenals)?
|
- Increased glucocorticoids (eg, exogenous, adrenal adenoma causing atrophy of contralateral adrenal cortex)
- Pituitary dysfunction (eg, Sheehan syndrome, panhypopituitarism) - Addison disease (autoimmune destruction) |
|
|
What do you need to evaluate if your patient has mild hypercalcemia?
|
Possible primary hyperparathyroidism
|
|
|
What is the PTH level in primary hyperparathyroidism?
|
PTH is usually in the upper part of the reference range (inappropriately not suppressed) or it may even be increased
|
|
|
What happens to Calcium in primary hyperparathyroidism?
|
Hypercalciuria may be present because the filtered load of calcium has exceeded the Tm for calcium in the kidney
|
|
|
What is the most common cause of primary hyperparathyroidism?
|
Parathyroid Adenoma
|

