![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
How common is clinically significant weight loss?
|
~4%
|
|
|
In an elderly patient with weight loss, what are the most common causes?
|
- Cancer
- Psychiatric problems - GI disorders - Med effects |
|
|
What is considered clinically significant unintentional weight loss?
|
Loss of 10 pounds or >5% of baseline body weight in 6-12 months
|
|
|
What do you need to establish first in a patient who has unintentional weight loss?
|
- Is it intentional (dieting?)
- Is the patient's food intake less (weight loss due to reduced caloric intake) or the same/increased (implies hypermetabolic state or absorption problem) |
|
|
What is the differential for weight loss?
|
DECREASED BODY MASS:
- Depression - Endocrinopathy (thyroid, adrenal insufficiency) - Cancer - Renal failure - Enteric (Crohn’s, chronic mesenteric ischemia) - Access to food (financial, transportation) - Systemic inflammatory dz (SLE, temporal arteritis) - Eating difficulty (tremor, dentures, dysphagia) - Diabetes Mellitus - Bulimia & Anorexia - Opportunistic Infection (HIV, TB, helminths) - Dementia - Yucky food (low salt, low fat, institutionalized) - Medication side effects/Substance Induced - Aging - Systemic chronic disease (CHF, COPD, cirrhosis) - Schizophrenia/Psychosis |
|
|
What is the most common medication to cause decreased eating? Why?
|
Digitalis / Digoxin - gives weird taste in mouth
|
|
|
Case 1:
Mrs. Twiggy Gaunt, a 45 y/o F presents to her PCP with 20 pound weight loss and fatigue for about a year. She states she was not intentionally attempting to lose weight. What is the next question that you should ask to begin to develop your differential? a) Whether her appetite has been diminished or if her food intake has been the same/increased b) If she is a member of NutriSystem, Jenny Craig or WeightWatchers c) If you can have that super cute dress she was wearing at her last visit since it is probably too big for her now d) If she wants to drink Boost or Ensure in chocolate, vanilla or strawberry |
Whether her appetite has been diminished or if her food intake has been the same/increased
|
|
|
Case 1:
- Mrs. Gaunt reports appetite and food intake hasn't changed - although maybe she gets full more quickly when eating - Feeling tired, denies other symptoms including depression, change in bowel habits, polyuria, or joint pains - She has enlarged spleen What should you consider first? |
Hematologic malignancy: lymphoma or leukemia
- She has no signs of liver disease and prevalence of EBV is low among married middle aged women |
|
|
What is a lymphoma? Types?
|
Malignancy of white blood cells arising in the lymph nodes
- Hodgkin's or Non-Hodgkin's Lymphoma |
|
|
What is a leukemia? Types?
|
Lymphoid neoplasms with widespread involvement of bone marrow. Tumor cells are usually found in peripheral blood.
• Acute Myelogenous Leukemia (AML) • Acute Lymphoblastic Leukemia (ALL) • Chronic Lymphocytic Leukemia (CLL) • Chronic Myeloid Leukemia (CML) • (Other) Hairy Cell Leukemia |
|
|
What should you think of if you see an African patient with a jaw mass?
|
Burkitt's (Non-Hodgkin) Lymphoma
|
|
|
What translocation is seen in Mantle Cell (Non-Hodgkin) Lymphoma? Cell marker? Prognosis?
|
t(11;14) - deactivation of cyclin D regulatory gene, CD5+,
- Poor prognosis |
|
|
What translocation is seen in Follicular (Non-Hodgkin) Lymphoma? Cell marker? Prognosis?
|
t(14;18) - bcl-2 expression, which inhibits apoptosis
- Indolent course, but difficult to cure |
|
|
What should you think of when you see a child with a mediastinal mass?
|
Lymphoblastic T cell (ALL)
|
|
|
Which non-Hodgkin Lymphoma is associated with mycosis fungoides?
|
Cutaneous T cell Lymphoma
|
|
|
Which non-Hodgkin Lymphoma is associated with HTLV-1 infection?
|
Adult T cell Lymphoma
|
|
|
Which non-Hodgkin Lymphoma is associated with H. pylori infection?
|
Marginal Cell MALToma
|
|
|
Which cancer has a "starry sky" histology? What is this?
|
Highly aggressive B cell non-Hodgkin lymhoma
- Sheets of lymphocytes with interspersed macrophages |
|
|
Who gets Burkitt's Lymphoma?
|
- Children and young adults, sporadically or associated with HIV
- In Africa, associated with EBV and presents as maxillary/mandibular mass |
|
|
What is the translocation associated with Burkitt's Lymphoma? Implications? Markers?
|
t(8;14) - c-MYC gene originally on chr 8
- Places c-MYC proto-oncogene adjacent to Ig heavy chain locus on 14w over-expression of the transcription factor c-MYC that leads to increased cell growth - CD20, CD10, and BCL-6 positive |
|
|
What are the complications of treating Burkitt's Lymphoma?
|
Treatment may lead to tumor lysis syndrome low phos, low calcium, increased uric acid, increased potassium and AKI, preventable w hydration and allopurinol
|
|
|
What are the symptoms that occur in Hodgkin's Lymphoma?
|
- B symptoms: weight loss, fevers, night sweats
- Patients sometimes itch - Node doesn't hurt |
|
|
What is the histologic sign of Hodgkin's Lymphoma?
|
Reed-Sternberg cells = cells are formed from germinal B cell centers
|
|
|
What are the markers positive in Hodgkin's Lymphoma?
|
CD15+ and CD30+
|
|
|
How do you treat Hodgkin's Lymphoma? Prognosis?
|
- Curable
- Excision - +XRT or advanced ABVD chemo: Adriamycin (doxorubicin), Bleomycin, Vinblastine, Dacarbazine) |
|
|
What are the subtypes (which are most common) of Hodgkin's Lymphoma?
|
- Nodular sclerosis (most common - 70%)
- Lymphocyte predominance (6% - popcorn cells) - Lymphocyte rich (40% - assoc. with EBV) - Lymphocyte depleted (HIV) - Mixed cellularity (25% - older patients with EBV) |
|
|
Which subtype of Hodgkin's Lymphoma is the most common version?
|
Nodular Sclerosis (70%)
|
|
|
Which subtype of Hodgkin's Lymphoma is described as having "popcorn cells"?
|
Lymphocyte Predominant (6%)
|
|
|
Which subtype of Hodgkin's Lymphoma is associated with EBV?
|
- Lymphocyte rich (40%)
- Mixed cellularity (older patients with EBV - 25%) |
|
|
Which subtype of Hodgkin's Lymphoma is associated with HIV?
|
Lymphocyte depleted
|
|
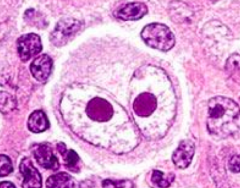
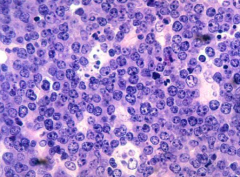
What is this?
|
Reed-Sternberg Cells looks like Owl's eyes
- Sign of Hodgkin's Lymphoma |
|
|
What is the mechanism of Vincristine? Most important side effect?
|
- M phase specific, blocks polymerization of microtubules so mitotic spindle cannot form
** Causes neuropathy (peripheral neuritis, areflexia, paralytic ileus) |
|
|
What is Vincristine used for? Most important side effect?
|
- Used in acute leukemia, Hodgkin's , Wilms tumor, choriocarcinoma
- Part of MOPP regimen for Hodgkin lymphoma ** Causes neuropathy (peripheral neuritis, areflexia, paralytic ileus) |
|
|
Case 1:
- Your preceptor tells you to go back and do a thorough lymph node exam - You cannot find a painlessly, enlarged submental, submandibular, anterior or posterior cervical, pre or post auricular, suboccipital, supraclavicular, axillary, epitrochelear, or even a medistinal node using your x ray vision and Twiggy refuses a groin exam What should you consider / do next? |
- Consider Leukemia
- Order a CBC |
|
|
What are the signs and symptoms of leukemia?
|
Unregulated growth of leukocytes in BM
- Bone pain - Decreasing working WBC → infections, especially cellulitis - Decreased Hgb & HCT → fatigue, dyspnea on exertion, pallor on exam - Decreased platelets → bleeding gums, epistaxis, petechiae - Hepatosplenomegaly (d/t leukemic infiltrates in liver, spleen, or lymph nodes) |
|
|
What are the signs of decreasing working WBCs in leukemia?
|
Infections, especially cellulitis
|
|
|
What are the signs of decreasing Hgb and HCT in leukemia?
|
- Fatigue
- Dyspnea on exertion - Pallor on exam |
|
|
What are the signs of decreasing platelets in leukemia?
|
- Bleeding gums
- Epistaxis - Petechiae |
|
|
Case 1:
Initial blood tests: • CBC: WBC 167,000; Hgb 11.5, HCT 33, MCV 99; Platelets 625,000 (Leukocytosis, normocytic/macrocytic anemia, thrombocytosis) • Blood smear many late granulocytic precursor cells, eosinophils and basophils, few metamyelocytes • Very low LAP leukocyte alkaline phosphatase (due to immature granulocytes) What additional testing should she get? |
Philadelphia chromosome testing
|
|
|
What is the translocation in the Philadelphia Chromosome? What disease is it seen in?
|
CML: Chronic Myelogenous Leukemia
- t(9;22) - forms BCR-ABL fusion gene, translocation of ABL proto-oncogene to BCR - BCR-ABL fusion protein results in constitutively active Abl tyrosine kinase in the Ras/Raf/MEK/MAPK pathway - Leads to apoptosis and unregulated cell division |
|
|
What translocation is responsible for CML (Chronic Myelogenous Leukemia)?
|
- t(9;22) - forms BCR-ABL fusion gene, translocation of ABL proto-oncogene to BCR
- BCR-ABL fusion protein results in constitutively active Abl tyrosine kinase in the Ras/Raf/MEK/MAPK pathway - Leads to apoptosis and unregulated cell division |
|
|
What is the average age of onset of Chronic Myelogenous Leukemia (CML) and symptoms?
|
- 35-55 years
- Splenomegaly, hepatomegaly, and lymphadenopathy - Leukocytosis and normocytic to macrocytic anemia - Platelet derangement either thrombocytosis during active phase or thrombocytopenia in spent phase - BM is hypercellular |
|
|
What is the histologic appearance of Chronic Myelogenous Leukemia (CML)?
|
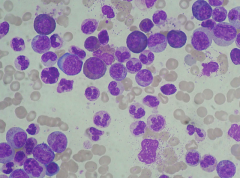
Promyelocytes
- Big cells and big nuclei - Coarse grains in cytoplasm - Basophilic |
|
|
Twiggy Gaunt your 45 y/o F patient presenting with weight loss, fatigue and splenomegaly tests positive for the Philadelphia chromosome. What is her most likely diagnosis?
a) Polycythemia vera b) Chronic myelogenous leukemia c) Acute myeloblastic leukemia d) Pernicious anemia e) Chronic lymphocytic leukemia |
Chronic myelogenous leukemia
|
|
|
What drug is used for CML? Significant side effects?
|
- Hydroxyurea
- Busalfan (Pulmonary Fibrosis) - Imatinib / Gleevac |
|
|
What is the mechanism of Imatinib / Gleevac?
|
Highly specific Bcr-Abl tyrosine kinase competitive inhibitor
- Blocks proliferation, induces apoptosis in Bcr-Abl positive cell lines and fresh leukemic cells |
|
|
30
|
30
|

