![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
What do you need to ask about for a patient with abdominal pain?
|
- Location
- Quality - Severity - Timing / duration - Context - Modifying factors - Associated signs & symptoms |
|
|
What are the most common differential diagnoses for abdominal pain in the RUQ?
|
Cholecystitis
Cholangitis Pancreatitis Pneumonia/empyema Pleurisy/pleurodynia Subdiaphragmatic abscess Hepatitis Budd-Chiari syndrome |
|
|
What are the most common differential diagnoses for abdominal pain in the RLQ?
|
Appendicitis
Salpingitis Inguinal hernia Ectopic pregnancy Nephrolithiasis Inflammatory bowel disease Mesenteric lymphadenitis Typhlitis |
|
|
What are the most common differential diagnoses for abdominal pain in the LUQ?
|
Splenic infarct
Splenic rupture Splenic abscess Gastritis Gastric ulcer Pancreatitis Subdiaphragmatic abscess |
|
|
What are the most common differential diagnoses for abdominal pain in the LLQ?
|
Diverticulitis
Salpingitis Inguinal hernia Ectopic pregnancy Nephrolithiasis Irritable bowel syndrome Inflammatory bowel disease |
|
|
What are the most common differential diagnoses for abdominal pain in the epigastric region?
|
Peptic ulcer disease
Gastritis GERD Pancreatitis Myocardial infarction Pericarditis Ruptured aortic aneurysm Esophagitis |
|
|
What are the most common differential diagnoses for abdominal pain in the periumbilical region?
|
Early appendicitis
Gastroenteritis Bowel obstruction Ruptured aortic aneurysm |
|
|
What are the most common differential diagnoses for abdominal pain that is diffuse and non-localized?
|
Mesenteric ischemia
Bowel obstruction Irritable bowel syndrome Peritonitis |
|
|
What extra-abdominal sources can refer pain to the abdomen?
|
Cardiac (MI, pericarditis)
Pulmonary (Pneumonia, PE, Pneumothorax) Esophageal (spasm, rupture, inflammation) Genitalia (Torsion of the testis) |
|
|
What is the difference between pain and tenderness?
|
- Pain is a symptom
- Tenderness is a sign (something found on physical exam, such as when you press on abdomen) |
|
|
What are some alternative ways to assess for rebound tenderness?
|
- Cough
- Sneeze - Heel slap/drop - Assess for guarding |
|
|
Where can pancreatitis have referred pain?
|
Back
|
|
|
Where can the diaphragm have referred pain?
|
Shoulder
|
|
|
Case 1:
- 19 yo female - 6 months of weight loss (30 lbs) - frenemies insist she is anorexic - Abdominal pain, diarrhea, sore butt and dirty underwear - Tired all of the time What is the differential diagnosis? |
- Inflammatory Bowel Disease
- Irritable Bowel Syndrome - Cancer - Chronic infection / parasites - Celiac Disease - Laxative use / Bulimia / Feeding disorder - Pelvic Inflammatory Disorder |
|
|
Case 1:
- 19 yo female - Peri-umbilical and "around like a belt" - Crampy pain, then eases off / comes back - "Can double me over" - Lasts 20 min or all night - Occurs 20 min after meals, "especially corn" - Appendectomy at 15, sister just diagnosed with MS - Lies down in fetal position to relieve pain - 30# weight loss, nausea when bad, night sweats, "sore butt" with "seepage", "exhausted all the time", diarrhea, "in the bathroom a dozen times yesterday" How does this additional information affect our differential diagnosis? |
- Inflammatory Bowel Disease - yes
- Irritable Bowel Syndrome - no - Cancer - possible - Chronic infection / parasites - this appears more severe - Celiac Disease - less likely, but seeing more systemic inflammation - Laxative use / Bulimia / Feeding disorder - seems more organic - Pelvic Inflammatory Disorder - yes |
|
|
Case 1:
- 19 yo female - Thin, slightly pale, Trochar scars, skin/mouth normal - Points to pain in peri-umbilical or "belt" region - BS slightly hyperactive - RLQ contains 4cm oval mass, firm, moderately tender (somewhat mobile with guarding and mild "rebound") - Pelvic: R adnexal motion tenderness - Rectal exam: tender/spastic sphincter, trace blood, small hole or deep dimple at 2:00, expressible brown/grey fluid, really, really tender What are the most likely diagnoses? |
- IBD
- PID - Cancer |
|
|
Case 1:
Now that you have your prioritized DDx, how will you nail this down? a) Labs b) CT c) MRI d) Colonoscopy e) Surgical exploration |
Colonoscopy
(although you will probably get a lot of these) (Colonoscopy takes a while to get because they have to prep, so in the mean time you will probably do labs) |
|
|
Case 1:
- What labs would you do for this patient? |
Inflammation:
- ESR 88 (elevated, normally ~10) - CRP 2.5 (good inflammatory marker, 15% do not respond appropriately with CRP, this is normal, but does not mean there is no inflammation) - Plt 505K (slightly elevated, goes along with inflammation) - WBC 8.1K (normal, tells you if acute infection, but doesn't tell you about chronic infection) Nutrition: - Albumin 2.6 (low, normal 3.5-4.5, t1/2 = 21 days) - Pre-Albumin 18 (normal, t1/2 = 7 days) - Total Lymphocyte Count 1.1K Enteric Loss: – Hgb 9.1 - Alb 2.6 - α1AT pending |
|
|
How do you evaluate the ESR?
|
- Take blood and anti-coagulate, then put in column 200 cm tall and set timer, see how many mL it has settled
- Max value is 100 because ~50% hematocrit - Normal is ~10 |
|
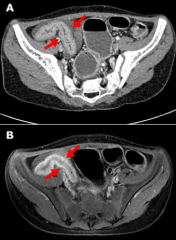
What kind of imaging is this? Why was this chosen?
|
MRI
- This is a young person, if this is a chronic problem, you don't want to be giving them tons of CTs - Also quality of MRIs is on par with CTs |
|
|
Case 1:
What history point is MOST specific to IBD? a) “Can double me over” b) Lie down in fetal position c) Sister was just diagnosed with MS d) 30# weight loss e) Bad diarrhea yesterday |
Sister was just diagnosed with MS
- For reasons we don't know, people who have IBD, have a 10% chance of having a relative with MS or IBD - People with MS have a 10% chance of having a relative with MS or IBD - Different manifestations of the same genetic issue |
|
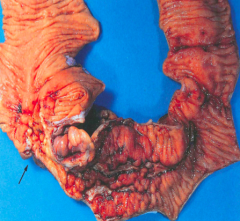
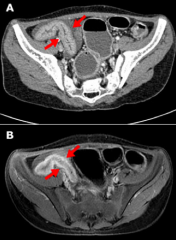
What is this pathology associated with?
|
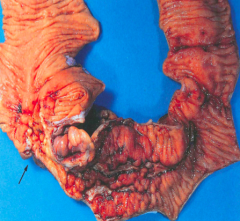
Crohn's Disease
- Transmural inflammation → fistulas - Cobblestone mucosa, creeping fat, bowel wall thickening, linear ulcers, fissures |
|
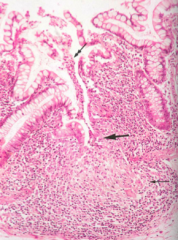
What is this pathology associated with?
|
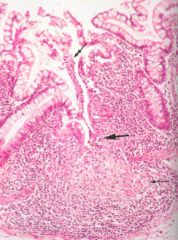
Noncaseating granulomas and lymphoid aggregates (Th1 mediated)
|
|
|
What are the complications of Crohn's Disease?
|
- Strictures (leading to obstruction)
- Fistulas - Perianal disease - Malabsorption - Nutritional depletion - Colorectal cancer - Gallstones |
|
|
What are the abdominal exam pearls?
|
- Epithelium = epithelium (ie, skin can reflect mucosa)
- Imaging / labs are very important - Rectal & pelvic = only direct access |
|

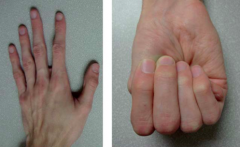
What is this?
|

Blue Rubber Bleb Nevus Syndrome
|
|
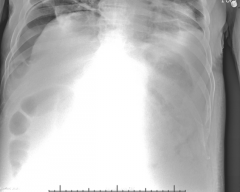
What is wrong here?
|
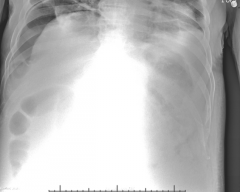
- Gas in abdomen = pneumoperitoneum
- Liver falls away on upright film |
|
|
Case 2:
- 26 yo female presents with sudden onset peri-umbilical abdominal pain that began about 1 hour prior to arrival - Started when she was out in her yard gardening - Has continued to worsen and has migrated tot he right mid and lower abdomen What other questions should we ask? |
- Mild back pain
- Nausea, but no vomiting - Normal BMs - No urinary symptoms - No vaginal bleeding or discharge - Last menstrual period was 4 weeks ago, she is d/t start in next few days - Denies being pregnant, does not have any children - Initially thought the pain was menstrual cramps, but it kept worsening - PMH: little is known; she is adopted, but was told her biologic father had “heart problems”; she was told by a doctor once she might have a murmur, but she never followed up; has not seen a doctor since she turned 18 y/o. ∗ PSH: None ∗ All: None ∗ Meds: None ∗ Social: Occasional alcohol; no smoking or drugs; single, works as a librarian ∗ FH: Unknown since she is adopted |
|
|
Case 2:
What physical exam things should you look for? |
∗ Awake and alert, uncomfortable appearing; tall and slender
∗ HEENT/Neck: unremarkable ∗ Chest: pectus excavatum ∗ Heart: II/VI Decrescendo diastolic murmur ∗ Lungs: Clear to auscultation ∗ Abdomen: TTP mid abdomen and RLQ; mild TTP on LLQ; no hepato or splenomegaly; no bruits; easily palpated aortic pulsations due to body habitus; no bruits; back normal ∗ Ext: no edema or swelling; normal strength; long fingers ∗ Skin: Striae on the lower abdomen and flanks; no rash |
|
|
Case 2:
- BP 86/65 - HR 122 - RR 24 - T 98.3 - O2 Sat: 99% on RA What is abnormal? |
- BP: low
- HR: elevated to compensate for BP - RR: elevated (maybe nervous) |
|
|
Case 2:
What are our priorities for treating this patient? |
Stabilization
- Give fluids / volume resuscitation - Need 3L of crystalloid to match blood, peripheral IV - Increase BP - Decrease HR - Continuous monitoring Establish Diagnosis and Treatment |
|
|
Case 2:
What tests can we do to "rule out" some of our differential diagnoses at the bedside? |
- Urine pregnancy
- Bedside ultrasound (Abdominal Aorta, Free Fluid - FAST, Intrauterine Pregnancy, Gallbladder) - Lateral decubitus x-ray |
|
|
What do you look for on FAST exam?
|
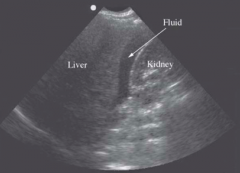
Look for fluid between liver and kidney
|
|
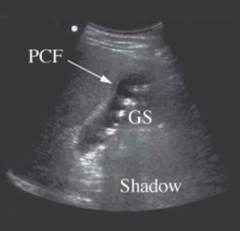
What does this show?
|
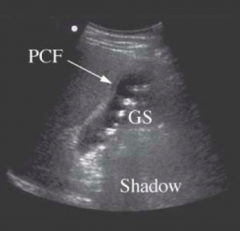
Gallstones
|
|
|
Case 2:
Which differential diagnoses have we not ruled out? |
- Pancreatitis
- Appendicitis - Ectopic pregnancy (still waiting on pregnancy test results) - Nephrolithiasis - Ruptured aortic aneurysm - Mesenteric ischemia (maybe) - Acute MI |
|
|
In addition to abdominal pain, the patient also had back pain. All of the following are retroperitoneal structures, and therefore can cause back pain EXCEPT:
a) Kidneys b) Proximal duodenum c) Aorta d) Rectum e) Ascending colon |
Proximal Duodenum
|
|
|
What is the test of choice to make the diagnosis?
a) Bedside ultrasound of the abdomen b) CT angiography of the abdomen c) KUB X-Ray d) MRI of the abdomen e) Physical examination |
CT angiography of the abdomen
(The bedside ultrasound could make the diagnosis, but the surgeon will want the CT angiography to determine the course of action for surgery) |
|
|
Case 2:
- You determine this patient has an abdominal aortic aneurysm Patient taken to the OR and has a graft placed to fix the infrarenal aneurysm. The flow of which of the following blood vessels could be affected during the procedure? a) Celiac axis b) Inferior mesenteric artery c) Renal arteries d) Right or left iliac arteries e) Superior mesenteric artery |
Inferior mesenteric artery
- Usually it is below the renal arteries |
|
|
What are the catastrophic causes of abdominal pain?
|
- Sudden onset, ill-appearing, unstable
- Ruptured abdominal aortic aneurysm - Mesenteric ischemia - Perforation of GI tract (ulcer, small bowel, appendix) - Ruptured ectopic pregnancy |
|
|
How big is an AAA?
|
>3 cm in diameter
|
|
|
What are the consequences of an AAA?
|
- Common cause of sudden death
- Most are asymptomatic until they rupture - Ruptured AAA has high mortality (most die before reaching hospital, surgery saves 60% who get to OR) |
|
|
What is the best indicator of risk of rupture of an AAA?
|
Size
|
|
|
What do you do if an AAA is determined to be <5.5 cm?
|
No survival advantage with surgery, surveillance by US is safe
|
|
|
What are the treatment options of AA?
|
∗ Open surgical repair was once considered the “gold
standard” treatment of AAAs ∗ Endovascular repair now supported by evidence - Lower morbidity and a faster return to work - Reintervention often needed |
|
|
What are the risk factors for AAA?
|
∗ Age
∗ Male ∗ Smoking ∗ Hypertension ∗ Aneurysm diameter ∗ Atherosclerosis ∗ Genetic factors |
|
|
What causes Marfan Syndrome?
|
- Autosomal dominant transmission
- Defective FBN1 gene: Marfan syndrome type 1 (MFS1) - Defect in TGFBR2 gene: Marfan syndrome type 2 (MFS2) |
|
|
What are the complications of Marfan Syndrome?
|
∗ Cardiovascular complications are major cause of mortality
∗ Valvular heart disease is common (AI, MVP, MR) ∗ Multiple CV pathologic processes in same patient ∗ Many patients experience a second or third aortic event Cardiovascular abnormalities ∗ Aortic root and ascending aorta dilation (70% of cases and the majority of mortality) ∗ Aortic aneurysms (thoracic and abdominal) ∗ Aortic dissection (predominantly type A) |
|
|
What are the pearls of abdominal pain?
|
∗ “If you don’t think of it, you won’t think of it”
∗ Think serious pathology first when patient ill appearing ∗ Systematically work through your differential ∗ Use simple tests to “rule out” obvious causes ∗ Be ready to deal with what you find |

