![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
127 Cards in this Set
- Front
- Back
|
Case 1:
- 25 yo mom delivers first infant at 30 weeks - Baby is grunting and retracting (signs of respiratory distress) - Pulse ox shows 72% - Infant diagnosed with respiratory distress syndrome (RDS) What is the primary underlying etiology of this baby’s hypoxia? a) Abnormal diffusion of oxygen b) Inadequate inspired oxygen c) Increased oxygen demand d) Developmental deficiency of surfactant e) Inability to unload oxygen in tissues |
Developmental deficiency of surfactant
|
|
|
What puts an infant at risk for Respiratory Distress Syndrome?
|
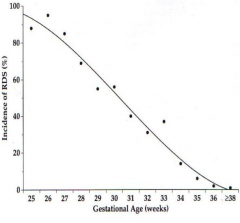
- Male predominance
- Low gestational age - Maternal diabetes - Perinatal asphyxia |
|
|
What is the source of surfactant?
|
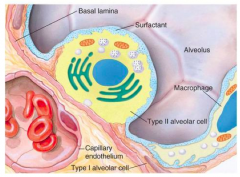
Type II Pneumocytes
|
|
|
What is the function of Surfactant?
|
- Reduces surface tension by spreading over the surface of alveoli (prevents collapse of alveoli)
- Hydrophilic and hydrophobic ends |
|
|
How does the size of the alveolus affect its collapsing pressure?
|

Larger alveolus -> low collapsing pressure
Small alveolus -> high collapsing pressure Small alveolus + Surfactant -> low collapsing pressure |
|
|
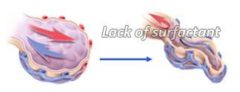
What causes Respiratory Distress Syndrome of the Newborn?
|
Decreased production and secretion of surfactant
|
|
|
What happens if there is a decreased production and secretion of surfactant?
|
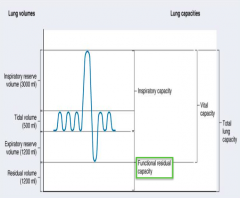
Failure to develop functional residual capacity (FRC), thus alveoli tend to collapse (atelectasis)
|
|
|
What should you do if you think a mom is going into labor prematurely?
|
Give mom steroids / dexamethasone helps to mature the infant lungs (give to moms who are going into labor prematurely), decreases incidence of RDS and morbidity/mortality
|
|
|
You begin oxygen supplementation but the baby remains somewhat desaturated (hypoxic). What is the appropriate next intervention to improve oxygenation?
a) Antibiotics b) Diuretics to remove excess fluid c) Intravenous steroids to accelerate lung development d) Continuous positive airway pressure |
Continuous positive airway pressure - this will acutely help them get oxygenated - keeps airway open even when exhaling
(Don't give baby steroids - you give it to mom; if you give steroids to baby it may affect their neurologic development) |
|
|
What are the possible causes of hypoxia?
|
- Decreased inspired oxygen (eg, high altitude)
- Hypoventilation - Diffusion abnormality - V/Q mismatch (ventilation / perfusion mismatch) - Inadequate oxygen carrying capacity (eg, abnormal hemoglobin, CO) |
|
|
What is the goal of treating hypoxia?
|
Identify and correct the specific abnormality
|
|
|
How can you calculate the alveolar partial pressure of O2 (PAO2)?
|
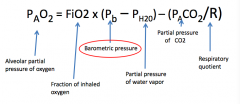
PAO2 = FiO2 * (Pb - Ph2o) - (PACO2 / R)
FiO2 = fraction of inhaled O2 Pb = barometric pressure Ph2o = partial pressure of water vapor PACO2 = partial pressure of CO2 R = respiratory quotient, normally 0.8 (>1 if you overfeed) |
|

How do you treat a patient with decreased inspired oxygen?
|
Provide additional O2 (return to lower altitude)
|
|
|
Why does hypoventilation cause hypoxia?
|
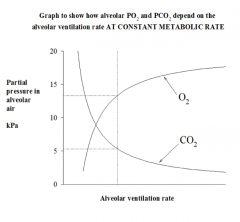
- The total pressure of gases in alveolus is relatively fixed
- Dalton's law states that the total pressure = sum of partial pressures - As partial pressure of CO2 rises, partial pressure of O2 must decrease |
|
|
What can cause hypoventilation / apnea in infants?
|
- Asphyxia
- Drugs - narcotic overdose (if mom is taking) - Sepsis / infection - Seizures - CNS bleeds - Metabolic abnormalities: hypoglycemia and hypoxia |
|
|
What layers do gases diffuse through to get into blood?
|
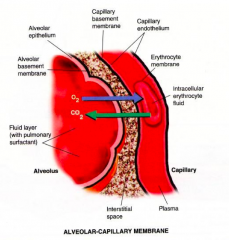
- Alveolar epithelium (coated with surfactant)
- Capillary endothelium |
|
|
What is Fick's Law of Diffusion?
|
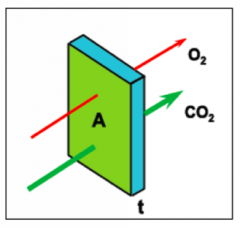
- Gas flux across thin membranes
- Follows partial pressure gradient Vgas = D * (A/t) * (P1 - P2) D = sol / √MW A = 85 m^2 per lung (area of alveolar membrane) t = 0.5 µm (thickness of alveolar membrane) |
|
|
Why do you see hypoxia before hypercarbia?
|
D-CO2 >> D-O2
- Hypoxia is a big drive to breathe, so you would be hyperventilating which would lead you to blowing off your excess CO2 - CO2 can diffuse more easily than O2 |
|
|
What can cause diffusion abnormalities of gases?
|
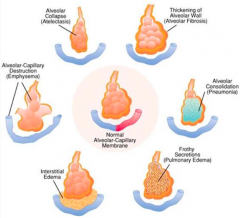
- Increased thickness of alveolar membrane (alveolar fibrosis): pulmonary edema and scarring of alveolar membrane
- Alveolar collapse: atelectasis - Alveolar-capillary destruction: emphysema - Interstitial edema - Frothy secretions: pulmonary edema - Alveolar consolidation: pneumonia |
|
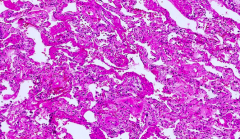
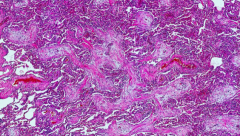
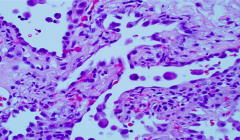
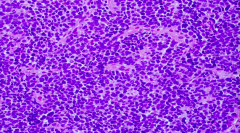
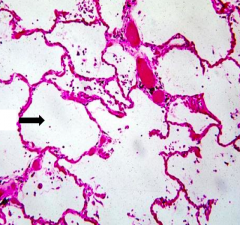
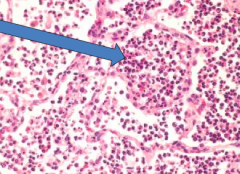
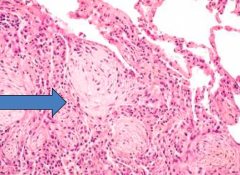
What does this slide show?
|
Hyaline membrane disease - dense pink membranous structures that are covering most of the alveolar surface
|
|
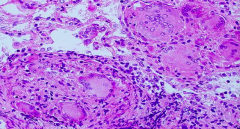
What does this slide show?
|
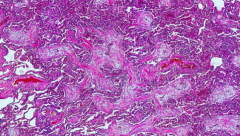
Organizing pneumonia
- Characterized by fibroblastic plugs (balls of fibroblastic tissue fills alveolar spaces) |
|
|
What causes Acute Respiratory Distress Syndrome in premature infants and others?
|
- Premature infants: developmental lack of surfactant
- In others (children and adults): inflammatory response to acute injury of lung tissue • Sepsis • Pneumonia • Trauma • Aspiration • Massive Transfusion • Near Drowning • Etc |
|
|
What is the pathogenesis leading to Acute Respiratory Distress Syndrome (ARDS)?
|
- Acute injury to alveolar epithelial or endothelial cells
- Alveolar macrophages and other cells release cytokines • Neutrophilic chemotaxis • Transmigration of neutrophils from capillaries into alveoli • Leakage of protein (fibrin) rich exudate forming HYALINE MEMBRANES • Damage to pneumocytes causing surfactant deficiency leading to atelectasis - Repair by type 2 pneumocytes - Progressive interstitial fibrosis |
|
|
What happens to a patient's lungs with Acute Respiratory Distress Syndrome (ARDS), if they survive?
|
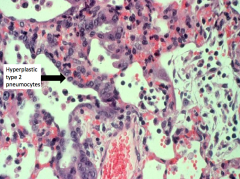
- Repair by type 2 pneumocytes (hyperplasia is due to diffuse alveolar damage)
- Progressive interstitial fibrosis |
|
|
What is the prognosis of Acute Respiratory Distress Syndrome (ARDS)?
|
Poor (~40-50% mortality rate)
|
|
|
What causes atelectasis in patients with Acute Respiratory Distress Syndrome (ARDS)?
|
Damage to pneumocytes causes a surfactant deficiency
|
|
|
What happens in diffuse alveolar damage?
|
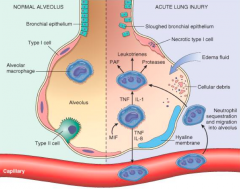
- Damage to epithelial cells lining alveoli
- Damage to endothelial cells - As a result of damage, there is necrosis of type 1 alveolar cells - Leakage of neutrophils and edema / fluid into alveolar spaces - Leads to cytokine release that perpetuate the process - Formation of hyaline membrane that lines alveolar wall |
|
|
What happens in the first 24 hours following diffuse alveolar damage?
|
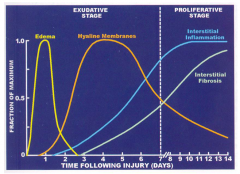
Edema
|
|
|
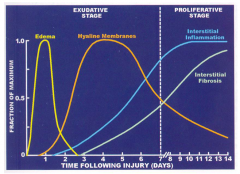
What happens in the first week following diffuse alveolar damage?
|
Exudative stage
- Edema (first 24 hours) - Hyaline membrane formation |
|
|
What happens after the first week following diffuse alveolar damage?
|
Proliferative stage
- Interstitial inflammation - Interstitial fibrosis |
|
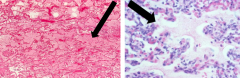
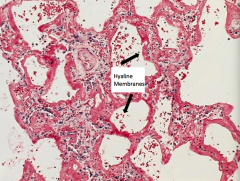
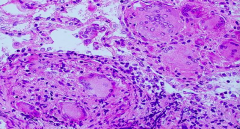
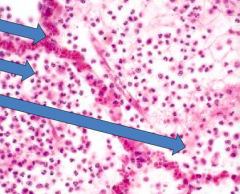
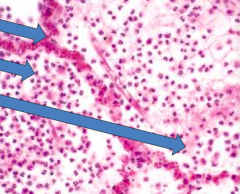
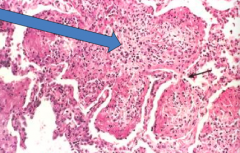
What do these images show?
|
Alveolar edema (occurs in first 24 hours following diffuse alveolar damage)
|
|
|
What causes endothelial or epithelial injury to the lungs?
|
- Initiated by numerous factors
- Non-heritable and heritable (response and survival depends on multiple loci on different chromosomes) - Mediators: cytokines, oxidants, growth factors - TNF, IL-1, IL-6, IL-10, TGF-β |
|
|
What should you see in a patient presenting acutely with Acute Respiratory Distress Syndrome (ARDS)?
|
Pulmonary edema (ground glass appearance)
|
|
|
Why if there is damage to the lungs does the peripheral WBC count decrease? Implications?
|
The WBCs are all in the lung, exacerbating the damage (damages type II cells which causes a surfactant deficiency)
|
|
|
Why don't we give surfactant to patients with ARDS?
|
We have tried, you can't get enough into the different spaces, it doesn't seem effective
|
|
|
How do you give surfactant to an infant?
|
Intubate patient and provide it through intubation, have to move them around to get it all around
|
|
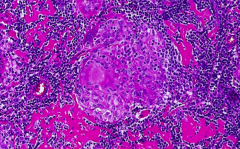
What does this slide show?
|
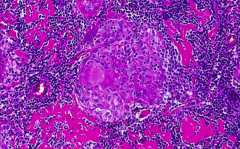
Granuloma - collection of histiocytes
|
|
What does this slide show?
|
Adenocarcinoma malignancy - neoplastic cells
- None of this looks normal |
|
|
What is the concept of V/Q match or mismatch?
|
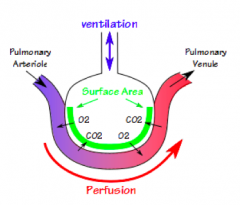
V = Ventilation
Q = Perfusion Want the areas getting lots of ventilation to get more perfusion |
|
|
How can V/Q Mismatch cause hypoxia?
|
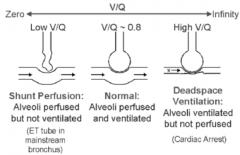
Low V/Q:
- Shunt perfusion - Alveoli perfused but not ventilated - Eg, ET tube in mainstem bronchus High V/Q: - Deadspace ventilation - Alveoli ventilated but not perfused - Eg, Cardiac arrest |
|
|
What is the normal V/Q ratio?
|
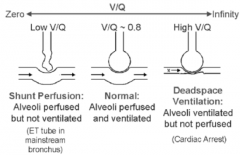
~0.8
- Alveoli are perfused and ventilated |
|
|
What are some causes of V/Q mismatch?
|
Impaired Ventilation:
- Obstruction of airways • Lower airway obstruction (asthma, COPD, inflammation) • Atelectasis (large area) • Pulmonary edema - Dereased respiratory drive • Narcotics • Injury to respiratory center Impaired perfusion - Decreased cardiac output - Obstruction of pulmonary blood flow (eg, Pulmonary Embolism) |
|
|
What can obstruct the airway? Implications?
|
Impairs ventilation - causes V/Q mismatch
• Lower airway obstruction (asthma, COPD, inflammation) • Atelectasis (large area) • Pulmonary edema |
|
|
What can decrease the respiratory drive? Implications?
|
Impairs ventilation - causes V/Q mismatch
• Narcotics • Injury to respiratory center |
|
|
What can decrease perfusion? Implications?
|
Causes V/Q mismatch
- Decreased cardiac output - Obstruction of pulmonary blood flow (eg, Pulmonary Embolism) |
|

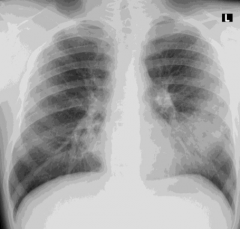
What do these chest x-rays show?
|
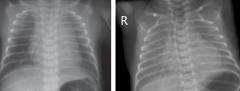
V/Q Mismatch
- Ground glass appearance |
|
|
How do you treat V/Q mismatch if there is an abnormality in ventilation?
|
- Oxygen
- Open airways by applying pressure - Diuretics if problem with pulmonary edema |
|
|
How do you treat V/Q mismatch if there is an abnormality in perfusion?
|
Increase CO
- Give volume - Vasodilators (if pulmonary vasoconstriction is issue) - Vasopressors (to increase output) Remove obstruction - TPA or embolectomy (if needed) |
|
|
What kind of drug would you use if pulmonary vasoconstriction is causing abnormalities in perfusion, leading to V/Q mismatch?
|
Vasodilators
|
|
|
How do you determine the Alveolar to arterial difference? Normal?
|
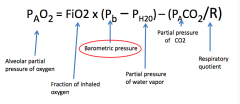
Alveolar to arterial gradient = PAO2 - PaO2 (measured)
- Normal: <10-50 torr (varies with age) PAO2 = FiO2 * (Pb - Ph2o) - (PACO2 / R) FiO2 = fraction of inhaled O2 Pb = barometric pressure Ph2o = partial pressure of water vapor PACO2 = partial pressure of CO2 R = respiratory quotient, normally 0.8 (>1 if you overfeed) |
|
|
What does a higher Alveolar to arterial difference indicate?
|
Pulmonary disease
- The higher the A-a gradient, the "worse" the pulmonary disease |
|
|
How do you determine the cause of hypoxemia?
|
- Give 100% O2
- If PaO2 goes up, then you know the ventilation is low (lung disease) - If PaO2 has no response, then the baby most likely has a R→L cardiac shunt |
|
|
What is methemoglobin?
|
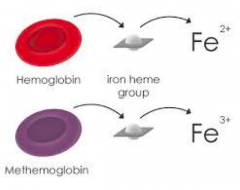
Heme group with Fe3+ (instead of Fe2+ which is found in normal hemoglobin)
|
|
|
What is the effect of methemoglobin on the O2-Hb dissociation?
|
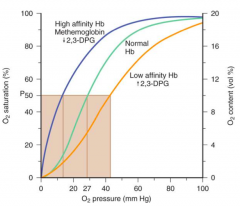
Methemoglobin increases affinity for O2 (harder to release)
|
|
|
What is the effect of 2,3-DPG on O2-hemoglobin dissociation?
|
- Shifts curve to right
- In tissues, releases O2 more easily |
|
|
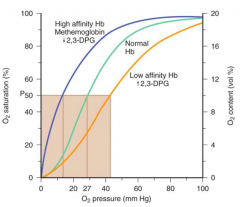
What is the effect of fetal hemoglobin on the O2-hemoglobin dissociation?
|
Fetal blood has a greater affinity for O2 than adult blood, so it can grab the O2 from the mom's hemoglobin
|
|
|
What shifts the O2-hemoglobin dissociation curve to the right?
|
- Increased temperature
- Decreased pH (increased H+) - More 2,3-DPG |
|
|
What are the consequences of hypoxia?
|
- Respiratory stimulation → tachypnea (↑ RR)
- Decreased O2 delivery → ↑ CO → tachycardia (↑ HR) - Closed airways → attempts to maintain patent airways → cough, retractions, grunting - Desaturated hemoglobin → cyanosis (requires 5g of desaturated hemoglobin) |
|
|
What happens if your hypoxia is caused by decreased respirations?
|
Respiratory stimulation → tachypnea (↑ RR)
|
|
|
What happens if your hypoxia is caused by decreased O2 delivery?
|
↑ CO → Tachycardia (↑ HR)
|
|
|
What happens if your hypoxia is caused by closed airways?
|
Attempts to maintain patent airways → retractions, grunting
|
|
|
What happens if your hypoxia is caused by desaturated hemoglobin?
|
Cyanosis (requires 5g of desaturated hemoglobin)
|
|
|
Who looks blue / cyanotic faster (patients with more or less hemoglobin)?
|
The more hemoglobin you have, the sooner you appear cyanotic because you only need 5g of desaturated hemoglobin, which will occur at a higher O2 saturation for someone with more hemoglobin
|
|
|
Which of the following interventions will likely decrease oxygen consumption in peripheral tissues of this ill neonate to attempt to match oxygen delivery?
a) Increased inspired O2 b) Transfuse with packed red blood cells c) Administer a paralytic agent and initiate mechanical ventilation d) Begin an inotrope to improve cardiac output e) Give a fluid bolus to improve venous return |
Administer a paralytic agent and initiate mechanical ventilation
|
|
|
What is "Oxygen Content"?
|

Amount of O2 bound to hemoglobin plus amount dissolved in arterial blood
|
|
|
What is "Oxygen Delivery"?
|
Amount of O2 transported from lungs to tissue
|
|
|
What is the "Mixed Venous Blood Oxygen Content"?
|
Amount of O2 bound to Hb + amount dissolved in mixed venous blood
|
|
|
Does the SVC or IVC have a lower mixed venous blood O2 content? Why?
|
SVC has a lower value because the brain extracts the most O2
|
|
|
What is "Oxygen Consumption"?
|
The rate at which O2 is removed from the blood for use by tissues
|
|
|
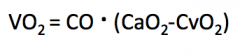
What is the relationship of VO2 (oxygen consumption) to exercise intensity?
|
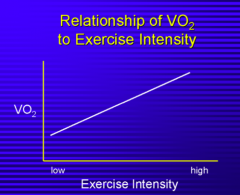
As exercise intensity increases, VO2 increases
|
|
|
What is O2 consumption proportional to?
|
- O2 delivery
- O2 extraction |
|
|
What is O2 extraction?
|
Proportion of O2 that is removed from the blood as it transverses the microcirculation
|
|
|
What happens to O2 consumption at rest?
|
Remains constant
|
|
|
What happens to O2 extraction as O2 delivery decreases?
|
O2 extraction from blood increases
|
|
|
What is the "critical DO2" (oxygen delivery)?
|
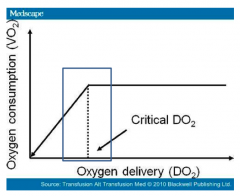
Threshold value of DO2 (oxygen delivery) below which VO2 (oxygen consumption) falls
|
|
|
What happens to the O2 delivery or O2 consumption / demand during pathology (eg, fever)?
|
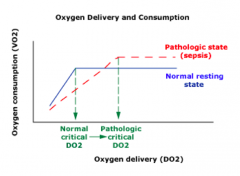
- Decreased O2 delivery
- Increased O2 consumption or demand (elevated in critically ill patients - respiratory distress, sepsis, septic shock, fever) |
|
|
What can cause decreased O2 delivery?
|
CO decreases
- Cardiac disease - Hypovolemia Arterial O2 content falls - Anemia - Poor oxygenation (hypoventilation, V/Q mismatch, diffusion, R→L shunt, abnormal hemoglobin) |
|
|
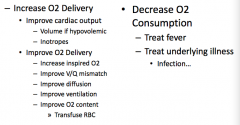
How do you treat a patient that has is not getting enough O2 delivery or has increased O2 consumption?
|
|
|
|
What happens if you decrease the work of breathing?
|
Decrease O2 demand / consumption
|
|
|
What are some other ways to increase O2 delivery?
|
Increase inspired O2 → move up O2 curve
- Improves O2 delivery to tissue Transfusion - Improves O2 content by increasing O2 carrying capacity (improves O2 delivery) |
|
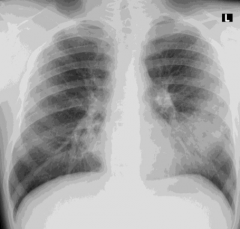
Case 2
- 18 yo previously healthy presents w/ SOB and fever - HR 94, RR 20, BP 118/74, T 39°C, SaO2 94% - He has rhonchi heard best in L base - Chest x-ray obtained - Albuterol (β2 agonist) inhalation treatment is ordered by intern and SaO2 drops to 85% What is the most likely reason for a drop in oxygen saturation following albuterol treatment? a) Inadequate oxygen supplementation b) Blunting of hypoxic pulmonary vasoconstriction c) Increase oxygen demand d) Inability to unload oxygen in the tissue e) Change in cardiac output caused by albuterol |
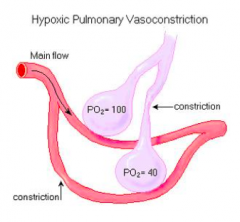
Blunting of hypoxic pulmonary vasoconstriction
|
|
Case 2:
You diagnose your patient with pneumonia. After the effects of albuterol wear off, you find he remains hypoxic, requiring oxygen supplementation. What is the most likely reason for his continued hypoxia? a) Abnormal diffusion of oxygen b) Inadequate inspired oxygen c) Increased oxygen demand d) Developmental deficiency of surfactant e) Inability to unload oxygen in tissues |
Abnormal diffusion of oxygen
Might also have increased O2 demand, but more importantly he has consolidation in his lungs causing a diffusion abnormality |
|
|
What is the likely etiology of his pneumonia?
a) Mycoplasma pneumoniae b) Haemophilus influenza c) Staphylococcus aureus d) Klebsiella pneumoniae e) Streptococcus pneumonia |
Streptococcus pneumonia
|
|
|
What are the most common causes of Community Acquired Pneumonia (CAP)?
|
85% of causes:
- S. pneumonia - H. influenza (decreasing since immunization available) - M. catarrhalis |
|
|
What are the potential causes of pneumonia that are not common in otherwise healthy patients?
|
- S. aureus (secondary infection following influenza)
- Klebsiellae (in chronic alcoholics) - Pseudomonas (in patients with CF or bronchiectasis |
|
|
Which cause of pneumonia is more common as a secondary infection following influenza?
|
S. aureus
|
|
|
Which cause of pneumonia is more common in chronic alcoholics?
|
Klebsiella
|
|
|
Which cause of pneumonia is more common in patients with CF or bronchiectasis?
|
Pseudomonas
|
|
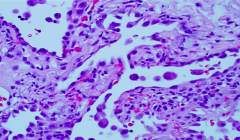
What does this slide represent?
|
This is consistent with case 2 (community acquired pneumonia)
|
|
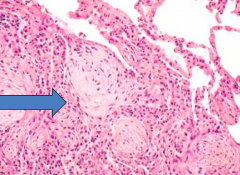
What does this slide represent?
|
Interstitial fibrosis - interstitial lung disease - some interstitial expansion with a bit of fibrosis and inflammation (not an interalveolar process)
|
|
What does this slide represent?
|
Granulomatous condition
|
|
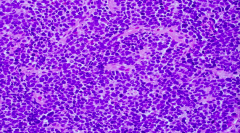
What does this slide represent?
|
Small cell carcinoma / malignancy
|
|
|
How do you acquire a typical community acquired pneumonia (CAP)?
|
- Majority by bacterial pathogens
- Usually due to aerosol inhalation from infected patient (can occur with aspiration of nasopharyngeal flora during sleep) |
|
|
Are there symptoms that are representative of community acquired pneumonia (CAP)?
|
No combination of symptoms or signs allows pneumonia to be definitively diagnosed or excluded
|
|
|
What are the possible patterns of gross morphology in pneumonia?
|
- Lobar pneumonia (entire lobe involved)
- Bronchopneumonia (patchy areas around bronchioles) |
|
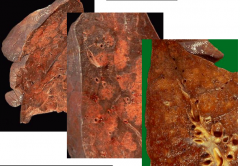
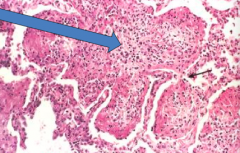
What do these images show?
|
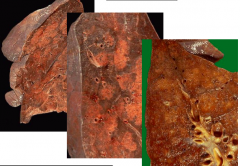
Bronchopneumonia (patchy areas around bronchioles)
|
|
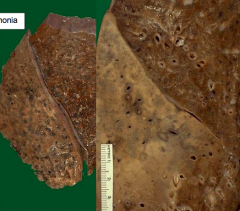
What do these images show?
|
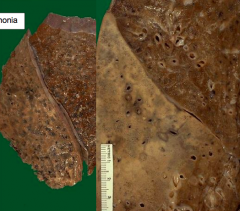
Lobar Pneumonia (entire lobe involved)
|
|
|
What are the stages of Lobar Pneumonia?
|
1. Congestion (first 24 hours)
2. Red hepatization (2-3 days) 3. Gray hepatization (2-3 days after red hepatization) 4. Resolution |
|
|
What happens in the first 24 hours of lobar pneumonia?
|
Congestion
|
|
|
What happens 2-3 days into a case of lobar pneumonia?
|
Red hepatization
|
|
|
What happens 2-3 days after red hepatization in a case of lobar pneumonia?
|
Gray hepatization
|
|
|
What happens after gray hepatization?
|
Resolution
|
|
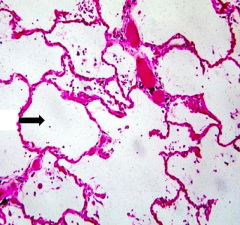
What does this image show?
|
Normal alveoli
|
|
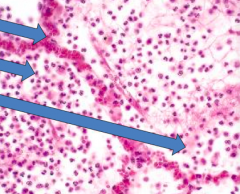
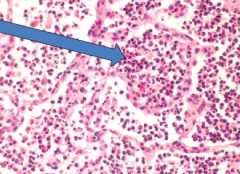
What does this image show?
|
Congestion (first 24 hours)
- Top arrow: vascular engorgement - Middle arrow: neutrophil migration - Bottom arrow: intra-alveolar fluid |
|
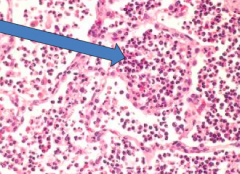
What does this image show?
|
Red Hepatization (2-3 days)
- Confluent exudate w/ RBCs and neutrophils - Red, firm and airless lung - "Liver-like" consistency |
|
What does this image show?
|
Gray Hepatization (2-3 days after red hepatization)
- Fibrinosuppurative exudate - Disintegration of RBCs |
|
What does this image show?
|
Resolution
- Resorption - Expectoration - Macrophage ingestion - Fibroblastic organization |
|
|
What is pleuritis?
|

Pleural fibrinous reaction to underlying inflammation
- Fibrinous organization (plaque formation)- |
|
|
What are the possible complications of pleuritis?
|
- Abscess
- Empyema (spreads into pleural space) - Organization (organizing pneumonia) - Bacteremic dissemination (septic emboli, endocarditis, arthritis, etc) |
|
|
What is a lung abscess?
|
Localized suppurative process within the lung, characterized by necrosis of lung tissue
|
|
|
What is the typical size/location of lung abscesses? Contents?
|
- Cavitary lesion: few mm to 6 cm or larger
- Cavity filled with suppurative material - neutrophils and necrotic debris - More common in R lung d/t angle of bronchi |
|
|
What bugs typically cause lung abscesses?
|
Anaerobes (most commonly)
- Peptostreptococcus species - Bacteroides species - Fusobacterium species - Microaerophilic streptococci Think ORAL flora (anaerobes that grow in your gingiva) |
|
|
What are the most common aerobes that can cause lung abscesses (although more commonly they are anaerobes)?
|
- Staphylococcus aureus
- Streptococcus pyogenes - Klebsiella pneumoniae - Haemophilus influenzae - Actinomyces species - Nocardia species - G- bacilli - Streptococcus pneumnoniae (rarely) |
|
|
What is a pleural effusion?
|
Abnormal fluid collection between pleura and lung
|
|
|
What can cause pleural effusions?
|
• Altered permeability of membranes, capillary bed: infection, malignancy
• Decreased oncotic vascular pressure: hypoalbuminemia • Increased vascular hydrostatic pressure: congestive heart failure • Disruption of blood or lymphatic vessels: hemothorax (trauma, blood) or chylothorax (lymphatic fluid) |
|
|
What is a hemothorax vs chylothorax?
|
Types of pleural effusions
- Hemothorax: blood in effusion - Chylothorax: lymphatic fluid in effusion |
|
|
What is the difference in causes between transudate and exudate?
|
Transudate
- Imbalance of hydrostatic or oncotic pressures - Eg, hypoalbuminemia, CHF, CSF leak (from ventricular shunt) Exudate - Inflammation - Disruption of lymphatic flow - Malignancy |
|
|
How can you determine if a patient has a transudate or exuate?
|
Thoracentesis
|
|
|
What are the criteria for exudates?
|
If any of the following:
- Pleural fluid / serum protein >0.5 - Pleural fluid / serum LDH >0.6 - Pleural fluid LDH >2/3 upper limits of normal for serum (requires simultaneous serum LDH and protein measurements) |
|
|
What other pleural fluid studies can you do?
|
- Glucose
- pH - Cell count, gram stain, culture, and cytology |
|
|
What does the pleural fluid glucose tell you?
|
Glucose <30-50:
- Malignancy, TB, esophageal rupture, lupus pleurisy Glucose <30: - Empyema, rheumatoid pleurisy |
|
|
What does the pleural fluid pH tell you?
|
In patients with empyema, if:
- pH 7.1-7.2 → drain - pH >7.3 → treat with antibiotics |
|
|
When should you treat an empyema by draining it?
|
If pH is between 7.1-7.2
|
|
|
When should you treat an empyema with antibiotics, instead of draining it?
|
If pH is >7.3
|
|
|
What does the pleural fluid cell count tell you?
|
- >85% lymphocytes → TB, sarcoidosis, lymphoma, chylothorax
- 50-70% lymphocytes → malignancy |
|
|
What does the pleural fluid gram stain tell you?
|
May identify organism
|
|
|
What does the pleural fluid cytology tell you?
|
Used for malignancies
|

