![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
191 Cards in this Set
- Front
- Back
|
What is the superior boundary of the axilla for dissection? |
Axillary vein
|
|
|
What is the posterior boundary of the axilla for dissection?
|
Long thoracic nerve
|
|
|
What is the lateral boundary of the axilla for dissection?
|
Latissimus dorsi muscle
|
|
|
What is the medial boundary of the axilla for dissection?
|
Lateral to, deep to, or medial to pectoral minor muscle, depending on level of nodes taken
|
|
|
What four nerves must the surgeon be aware of during an axillary dissection?
|
1. Long thoracic nerve2. Thoracodorsal nerve3. Medial pectoral nerve4. Lateral pectoral nerve
|
|
|
What is the location and innervation to of the long thoracic nerve?
|
- Courses along lateral chest wall in midaxillary line on serratus anterior muscle- Innervates serratus anterior muscle
|
|
|
What is the location and innervation to of the thoracodorsal nerve?
|
- Courses lateral to long thoracic nerve on latissimus dorsi muscle- Innervates latissimus dorsi muscle
|
|
|
What is the location and innervation to of the medial pectoral nerve?
|
- Runs lateral to or through the pectoral minor muscle, actually lateral to the lateral pectoral nerve- Innervates the pectoral minor and pectoral major muscles
|
|
|
What is the location and innervation to of the lateral pectoral nerve?
|
- Runs medial to the medial pectoral nerve (names describe orientation from brachial plexus!)- Innervates the pectoral major
|
|
|
If the medial pectoral nerve is lateral to the lateral pectoral nerve why are they named as such?
|
Names describe the orientation in the brachial plexus
|
|
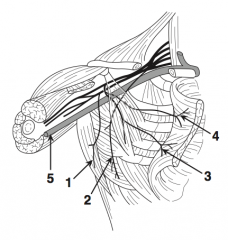
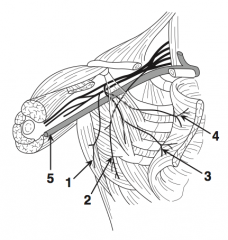
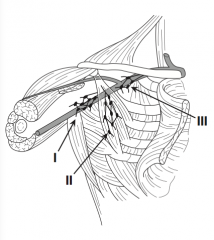
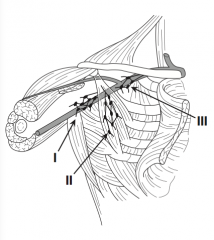
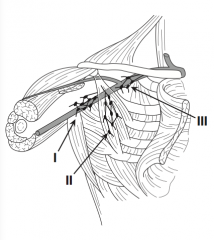
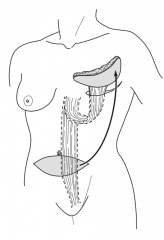
What is nerve 1?
|
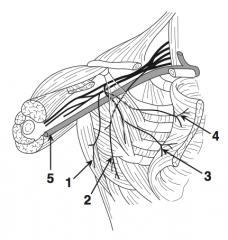
Thoracodorsal nerve (1) |
|
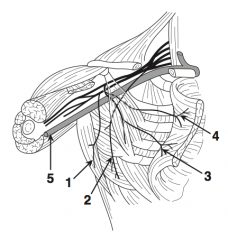
What is nerve 2?
|
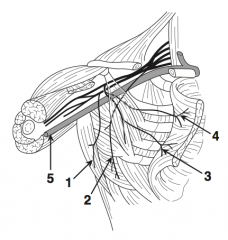
Long thoracic nerve (2)
|
|
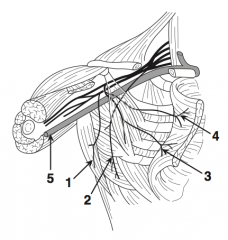
What is nerve 3?
|
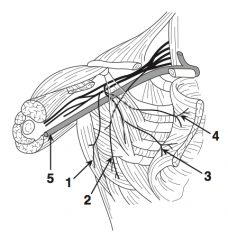
Medial pectoral nerve (3)
|
|
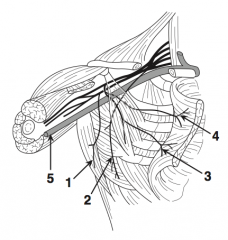
What is nerve 4?
|
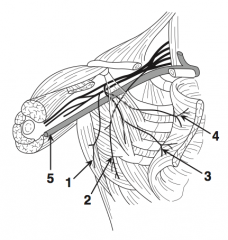
Lateral pectoral nerve (4)
|
|
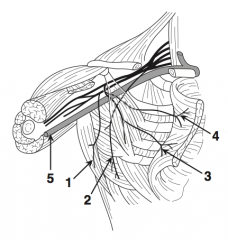
What is structure 5?
|
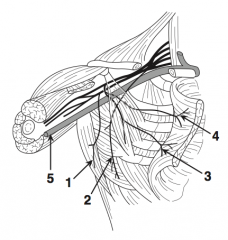
Axillary vein (5)
|
|
What is the name of the deformity if you cut the long thoracic nerve (2)? |
"Winged scapula" |
|
|
What is the name of the cutaneous nerve that crosses the axilla in a transverse fashion? (Many surgeons try to preserve this nerve)
|
Intercostobroachial nerve
|
|
|
What is the name of the large vein that marks the upper limit of the axilla?
|
Axillary vein
|
|
|
What is the lymphatic drainage of the breast?
|
- Lateral: axillary lymph nodes- Medial: parasternal nodes that run with internal mammary artery
|
|
|
What are the levels of axillary lymph nodes?
|
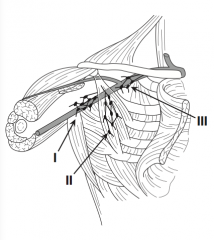
- Level 1 (low): lateral to pectoral minor - Level 2 (middle): deep to pectoral minor - Level 3 (high): medial to pectoral minor
|
|
|
Where are "level I" lymph nodes?
|
"Low": lateral to pectoral minor
|
|
|
Where are "level II" lymph nodes?
|
"Middle": deep to pectoral minor
|
|
|
Where are "level III" lymph nodes?
|
"High": medial to pectoral minor
|
|
|
What does the levels of axillary lymph node involvement tell you?
|
The higher level of involvement has a worse prognosis, but the level of involvement is less important than the number of positive nodes
|
|
|
What are Rotter's nodes?
|
Nodes between the pectoralis major and minor muscles; not usually removed unless they are enlarged or feel suspicious intraoperatively
|
|
|
What are the suspensory breast ligaments called?
|
Cooper's ligaments
|
|
|
What is the mammary "milk line"?
|
Embryological line from shoulder to thigh where "supernumerary" breast areolar and/or nipples may be found
|
|
|
What is the "tail of Spence"?
|
"Tail" of breast tissue that tapers into the axilla
|
|
|
Which hormone is mainly responsible for breast milk production?
|
Prolactin
|
|
|
What is the incidence of breast cancer?
|
12% lifetime risk
|
|
|
What percentage of women with breast cancer have no known risk factor?
|
75%
|
|
|
What percentage of all breast cancers occur in women younger than 30 years?
|
~2%
|
|
|
What percentage of all breast cancers occur in women older than 70 yeras?
|
33%
|
|
|
What are the major cancer susceptibility genes?
|
BRCA1 and BRCA2 (BReast CAncer)
|
|
|
What option exists to decrease the risk of breast cancer in women with BRCA?
|
Prophylactic bilateral mastectomy
|
|
|
What is the most common motivation for medicolegal cases involving the breast?
|
Failure to diagnose a breast carcinoma
|
|
|
What is the "Triad of Error" for misdiagnosed breast cancer?
|
1. Age <45 years2. Self-diagnosed mass3. Negative mammogram Note: 75% of cases of misdiagnosed breast cancer have these three characteristics
|
|
|
What are the history risk factors for breast cancer?
|
NAACP:- Nulliparity- Age at menarche (<13 years)- Age at menopause (>55 years)- Cancer of the breast (in self or family)- Pregnancy with first child (>30 years)
|
|
|
What are physical / anatomic risk factors for breast cancer?
|
CHAFED LIPS:- Cancer in the breast (3% synchronous contralateral cancer)- Hyperplasia (moderate/florid) (2x risk)- Atypical hyperplasia (4x)- Female (100x male risk)- Elderly- DCIS - LCIS- Inherited genes (BRCA I and II)- Papilloma (1.5x)- Sclerosing adenosis (1.5x)
|
|
|
What is the relative risk of hormone replacement therapy for getting breast cancer?
|
1-1.5
|
|
|
Is "run of the mill" fibrocystic disease a risk factor for breast cancer?
|
No
|
|
|
What are the possible symptoms of breast cancer?
|
- No symptoms- Mass in breast- Pain (most are painless)- Nipple discharge- Local edema- Nipple retraction- Dimple- Nipple rash
|
|
|
Why does skin retraction occur with breast cancer?
|
Tumor involvement of Cooper's ligaments and subsequent traction on ligaments pull skin inward
|
|
|
What are the signs of breast cancer?
|
- Mass (1 cm is usually the smallest lesion that can be palpated on exam)- Dimple- Nipple rash- Edema- Axillary / supraclavicular nodes
|
|
|
What is the most common site of breast cancer?
|
Approximately 1/2 of cancers develop in the upper outer quadrants
|
|
|
What are the different types of invasive breast cancer? How common is each?
|
- Infiltrating Ductal Carcinoma (~75%)- Medullary Carcinoma (~15%)- Infiltrating Lobular Carcinoma (~5%)- Tubular Carcinoma (~2%)- Mucinous Carcinoma (colloid) (~1%)- Inflammatory Breast Cancer (~1%)
|
|
|
What is the most common type of breast cancer?
|
Infiltrating Ductal Carcinoma
|
|
|
What is the differential diagnosis for breast cancer?
|
- Fibrocystic disease of the breast- Fibroadenoma- Intraductal papilloma- Duct ectasia- Fat necrosis- Abscess- Radial scar- Simple cyst
|
|
|
Describe the appearance of the edema of the dermis in inflammatory carcinoma of the breast?
|
Peau d'orange (orange peel)
|
|
|
What are the screening breast exam recommendations?
|
- Self-exam of breasts monthly- Ages 20-40 years: breast exam every 2-3 years by a physician- >40 years: annual breast exam by physician
|
|
|
What are the screening mammogram recommendations?
|
Recommendations are controversial, but most experts say:- Baseline mammogram between 35-40 years- Mammogram every year or every other year between 40-50 years- Mammogram yearly after age 50
|
|
|
What is the best time for breast self-exams?
|
1 week after menstrual period
|
|
|
Why is mammography a more useful diagnostic tool in older women than younger?
|
Breast tissue undergoes fatty replacement with age, making masses more visible; younger women have more fibrous tissue, which makes mammograms harder to interpret
|
|
|
What are the radiographic tests for breast cancer?
|
- Mammography - Breast ultrasound - MRI |
|
|
What is the classic picture of breast cancer on mammogram?
|
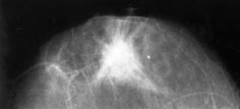
Spiculated mass
|
|
|
What option is best to evaluate a breast mass in a woman younger than 30 years?
|
Breast ultrasound
|
|
|
What are the methods for obtaining breast tissue for pathologic examination?
|
- Fine needle aspiration (FNA)- Core biopsy (larger needle core sample)- Mammotome stereotactic biopsy- Open biopsy - incisional (cutting a piece of mass) or excisional (cutting out entire mass)
|
|
|
What are the indications for biopsy of breast tissue?
|
- Persistent mass after aspiration- Solid mass- Blood in cyst aspirate- Suspicious lesion by mammography / US / MRI- Bloody nipple discharge- Ulcer or dermatitis of nipple- Patient's concern of persistent breast abnormality
|
|
|
What is the process for performing a biopsy when a non-palpable mass is seen on mammogram?
|
Stereotactic (mammotome) biopsy or needle localization biopsy
|
|
|
What is a needle loc biopsy (NLB)?
|
Needle localization by radiologist, followed by biopsy; removed breast tissue must be checked by mammogram to ensure all suspicious lesion has been excised
|
|
|
What is a mammotome biopsy?
|
Mammogram-guided computerized sterotactic core biopsies
|
|
|
What is obtained first, the mammogram or the biopsy?
|
Mammogram is obtained first; otherwise, tissue extraction (core or open) may alter the mammographic findings (FNA may be done prior to mammogram because fine needle usually will not affect the findings)
|
|
|
What would be suspicious mammographic findings?
|
Mass, microcalcifications, stellate / spiculated mass
|
|
|
What is a "radial scar" seen on mammogram?
|
Spiculated mass with central lucency, +/- microcalcifications
|
|
|
What tumor is associated with a radial scar?
|
Tubular carcinoma; thus biopsy is indicated
|
|
|
What is the workup for a breast mass?
|
1. Clinical breast exam2. Mammogram or breast ultrasound3. Fine needle aspiration, core biopsy, or open biopsy
|
|
|
How do you proceed if the mass appears to be a cyst?
|
Aspirate it with a needle
|
|
|
Is the fluid from a breast cyst sent for cytology?
|
Not routinely; bloody fluid should be sent though
|
|
|
When do you proceed to open biopsy for a breast cyst?
|
1. In the case of a second cyst recurrence2. Bloody fluid in the cyst3. Palpable mass after aspiration
|
|
|
What is the pre-op staging workup in a patient with breast cancer?
|
- B/l mammogram (cancer in one breast is a risk factor for cancer in contralateral breast - CXR (to check for lung metastasis) - LFTs (to check for liver metastasis) - Serum calcium level, alkaline phosphatase (if these tests indicate bone metastasis / "bone pain", proceed to bone scan) - Other tests depending on signs/symptoms (eg, head CT if pt has focal neuro deficit, to look for brain metastasis) |
|
|
What hormone receptors must be checked for in biopsy specimen?
|
Estrogen and progesterone receptors - this is key for determining adjuvant treatment; must be obtained on all specimens (including fine needle aspirates)
|
|
|
What staging system is used for breast cancer? |
TMN: Tumor / Metastases / Nodes (AJCC) |
|
|
What is "stage I" breast cancer? |
Tumor ≤ 2 cm in diameter without metastases, no nodes |
|
|
What is "stage IIA" breast cancer? |
- Tumor ≤ 2 cm in diameter with mobile axillary nodes OR - Tumor 2-5 cm in diameter with no nodes |
|
|
What is "stage IIB" breast cancer? |
- Tumor 2-5 cm in diameter with mobile axillary nodes OR - Tumor >5 cm with no nodes |
|
|
What is "stage IIIA" breast cancer? |
- Tumor >5 cm with mobile axillary nodes OR - Any size tumor with fixed axillary nodes, no metastases |
|
|
What is "stage IIIB" breast cancer? |
- Peau d'orange (skin edema) OR - Chest wall invasion / fixation OR - Inflammatory cancer OR - Breast skin ulceration OR - Breast skin satellite metastases OR - Any tumor and + ipsilateral internal mammary lymph nodes |
|
|
What is "stage IIIC" breast cancer? |
- Any size tumor, no distant mets - Positive: supraclavicular, infraclavicular, or internal mammary lymph nodes |
|
|
What is "stage IV" breast cancer? |
Distant metastases (including ipsilateral supraclavicular nodes) |
|
|
What are the sites of metastases of breast cancer? |
- Lymph nodes (most common) - Lung / pleura - Liver - Bones - Brain |
|
|
What are the major treatments of breast cancer? |
- Modified radical mastectomy - Lumpectomy and radiation + sentinel lymph node dissection - Both treatments either +/- postop chemotherapy / tamoxifen |
|
|
What are the indications for radiation therapy after a modified radical mastectomy? |
- Stage IIIA - Stage IIIB - Pectoral muscle / fascia invasion - Positive internal mammary LN - Positive surgical margins - ≥ 4 positive axillary LNs post-menopausal |
|
|
What breast carcinomas are candidates for lumpectomy and radiation (breast-conserving therapy)? |
Stage I and II (tumors <5 cm) |
|
|
What approach may allow a patient with stage IIIA cancer to have breast conserving surgery? |
NEOadjuvant chemotherapy - if the pre-op chemo shrinks the tumor |
|
|
What is the treatment of inflammatory carcinoma of the breast? |
Chemotherapy first! Then often followed by radiation, mastectomy, or both |
|
|
What is a "lumpectomy and radiation"? |
- Lumpectomy (segmental mastectomy: removal of a part of the breast) - Axillary node dissection - Course of radiation therapy after operation, over a period of several weeks |
|
|
What is the major absolute contraindication to lumpectomy and radiation? |
Pregnancy |
|
|
What are other contraindications to lumpectomy and radiation? |
- Previous radiation to the chest - Positive margins - Collagen vascular disease (eg, scleroderma) - Extensive DCIS (often seen as diffuse microcalcification)
Relative contraindications: - Lesion that cannot be seen on the mammograms (ie, early recurrence will be missed on follow-up mammograms) - Very small breast (no cosmetic advantage) |
|
|
What is a modified radical mastectomy? |
- Breast, axillary nodes (level II, I), and nipple-areolar complex are removed - Pectoralis major and minor muscles are not removed (Auchincloss modification) - Drains are placed to drain lymph fluid |
|
|
Where are the drains placed with a modified radical mastectomy (MRM)? |
1. Axilla 2. Chest wall (breast bed) |
|
|
When should the drains be removed? |
<30 cc / day drainage |
|
|
What are the potential complications after a modified radical mastectomy? |
Ipsilateral arm lymphedema, infection, injury to nerves, skin flap necrosis hematoma / seroma, phantom breast syndrome |
|
|
During an axillary dissection, should the patient be paralyzed? |
No, because the nerves (long thoracic / thoracodorsal) are stimulated with resultant muscle contraction to help identify them |
|
|
How can the long thoracic and thoracodorsal nerves be identified during an axillary dissection? |
Nerves can be stimulated with a forceps, which results in contraction of the latissimus dorsi (thoracodorsal nerve) or anterior serratus (long thoracic nerve) |
|
|
When do you remove the drains after an axillary dissection? |
When there is <30 cc of drainage per day, or on POD #14 (whichever comes first) |
|
|
What is a sentinel node biopsy? |
Instead of removing all the axillary lymph nodes, the primary draining or "sentinel" lymph node is removed |
|
|
How is the sentinel lymph node found? |
Inject blue dye and/or technetium-labeled sulfur colloid (best results with both) |
|
|
What follows a positive sentinel node biopsy? |
Removal of the rest of the axillary lymph nodes |
|
|
What is now considered the standard of care for lymph node evaluation in women with T1 or T2 tumors (stages I and IIA) and clinically negative axillary lymph nodes? |
Sentinel lymph node dissection |
|
|
What do you do with a mammotome biopsy that returns as "atypical hyperplasia"? |
Open needle loc biopsy as many will have DCIS or invasive cancer |
|
|
How does tamoxifen work? |
It binds estrogen receptors |
|
|
What is the treatment for local recurrence in breast after lumpectomy and radiation? |
"Salvage" mastectomy |
|
|
Can tamoxifen prevent breast cancer? |
Yes - in the breast cancer prevention trial of 13,000 women at increased risk of developing breast cancer, tamoxifen reduced risk by ~50% across all ages |
|
|
What are common options for breast reconstruction? |
- TRAM flap - Implant - Latissimus dorsi flap |
|
|
What is a TRAM flap? |
Transverse Rectus Abdominis Myocutaneous flap |
|
|
What are the side effects of tamoxifen? |
- Endometrial cancer (2.5x relative risk) - DVT - PE - Cataracts - Hot flashes - Mood swings |
|
|
In high-risk women, is there a way to reduce the risk of developing breast cancer? |
Yes, tamoxifen for 5 years will lower the risk by up to 50%, but, with an increased risk of endometrial cancer and clots, it must be an individual patient determination |
|
|
What is the common adjuvant therapy for a premenopausal patient with node +, ER - breast cancer? |
Chemotherapy |
|
|
What is the common adjuvant therapy for a premenopausal patient with node+, ER + breast cancer? |
Chemotherapy + Tamoxifen |
|
|
What is the common adjuvant therapy for a premenopausal patient with node -, ER + breast cancer? |
Tamoxifen |
|
|
What is the common adjuvant therapy for a postmenopausal patient with node +, ER + breast cancer? |
Tamoxifen, +/- chemotherapy |
|
|
What is the common adjuvant therapy for a post-menopausal patient with node +, ER - breast cancer? |
Chemotherapy, +/- tamoxifen |
|
|
What type of chemotherapy is usually used for breast cancer? |
- CMF (Cyclophosphamide, Methotrexate, 5-Fluorouracil) OR - CAF (Cyclophosphamide, Adriamycin, 5-Fluorouracil) |
|
|
Chemotherapy for high-risk tumors with negative lymph nodes should be considered. What makes a tumor "HIGH RISK"? |
High risk: - >1 cm in size - Lymphatic / vascular invasion - Nuclear grade (high) - S phase (high) - ER negative - HER-2 / neu over-expression |
|
|
What does DCIS stand for? |
Ductal Carcinoma In Situ |
|
|
What is DCIS also known as? |
Intraductal Carcinoma |
|
|
Describe DCIS? |
Cancer cells in the duct without invasion (in situ: cells do not penetrate the basement membrane) |
|
|
What are the signs / symptoms of DCIS? |
Usually none; usually non-palpable |
|
|
What are the mammographic findings of DCIS? |
Microcalcifications |
|
|
How is the diagnosis of DCIS made? |
Core or open biopsy |
|
|
What is the most aggressive histologic type of DCIS? |
Comedo |
|
|
What is the risk of lymph node metastasis with DCIS? |
<2% (usually when microinvasion is seen) |
|
|
What is the major risk with DCIS? |
Subsequent development of infiltrating ductal carcinoma in the same breast |
|
|
What is the treatment for DCIS with a tumor <1 cm (low grade)? |
Remove with 1 cm margins +/- XRT |
|
|
What is the treatment for DCIS with a tumor >1 cm (low grade)? |
Perform lumpectomy with 1 cm margins and radiation or total mastectomy (no axillary dissection) |
|
|
What is a total (simple) mastectomy? |
Removal of the breast and nipple without removal of the axillary nodes (always remove nodes with invasive cancer) |
|
|
When must a simple mastectomy be performed for DCIS? |
Diffuse breast involvement (eg, diffuse microcalcifications), >1 cm and contraindicatiosn to radiation |
|
|
What is the role of axillary node dissection with DCIS? |
No role in true DCIS (ie, without microinvasion); some perform a sentinel lymph node dissection for high-grade DCIS |
|
|
What is adjuvant for DCIS? |
1. Tamoxifen 2. Post-lumpectomy XRT |
|
|
What ist he role of tamoxifen in DCIS? |
Tamoxifen for 5 years will lower the risk up to 50%, but with increased risk of endometrial cancer and clots; it must be an individual patient determination |
|
|
What is a memory aid for the breast in which DCIS breast cancer arises? |
Cancer arises in the same breast as DCIS (DCIS = Directly in same breast) |
|
|
What is LCIS? |
Lobular Carcinoma In Situ (carcinoma cells in lobules of the breast without invasion) |
|
|
What are the signs / symptoms of LCIS? |
There are none |
|
|
What are the mammographic findings of LCIS? |
There are none |
|
|
How is the diagnosis of LCIS made? |
LCIS is found incidentally on biopsy |
|
|
What is the major risk of LCIS? |
Carcinoma of either breast |
|
|
Which breast is most at risk for developing an invasive carcinoma? |
Equal risk in both breasts! Think of LCIS as a risk marker for future development of cancer in either breast. |
|
|
What percentage of women with LCIS develop an invasive breast carcinoma? |
~30% in 20 years after diagnosis of LCIS |
|
|
What type of invasive breast cancer do patients with LCIS develop? |
Most commonly, infiltrating ductal carcinoma, with equal distribution in the contralateral and ipsilateral breasts |
|
|
What medication may lower the risk of developing breast cancer in LCIS? |
Tamoxifen for 5 years will lower the risk up to 50%, but with an increased risk of endometrial cancer and clots; it must be an individual patient determination |
|
|
What is the treatment of LCIS? |
Close follow-up (or bilateral simple mastectomy in high-risk patients) |
|
|
What is the major difference in the subsequent development of invasive breast cancer with DCIS and LCIS? |
LCIS cancer develops in either breast; DCIS cancer develops in the ipsilateral breast |
|
|
How do you remember which breast is at risk for invasive cancers in patients with LCIS? |
Think: LCIS = Liberally in either breast |
|
|
What is the most common cause of bloody nipple discharge in a young woman? |
Intraductal papilloma |
|
|
What is the most common breast tumor in patients younger than 30 years? |
Fibroadenoma |
|
|
What is Paget's disease of the breast? |
Scaling rash / dermatitis of the nipple caused by invasion of skin by cells from a ductal carcinoma |
|
|
What are the common options for breast reconstruction after a mastectomy? |
- Saline implant - TRAM flap |
|
|
What is the incidence of breast cancer in men? |
<1% of all breast cancer cases (1/150) |
|
|
What is the average age at diagnosis of breast cancer in males? |
65 years of age |
|
|
What are the risk factors for male breast cancer? |
- Increased estrogen - Radiation - Gynecomastia from increased estrogen - Estrogen therapy - Klinefelter's syndrome (XXY) - BRCA2 carriers |
|
|
Is benign gynecomastia a risk factor for male breast cancer? |
No |
|
|
What type of breast cancer do men develop? |
Nearly 100% of cases are ductal carcinoma (men do not usually have breast lobules) |
|
|
What are the signs / symptoms of breast cancer in men? |
- Breast mass (most are painless) - Breast skin changes (ulcers, retraction) - Nipple discharge (usually blood or a blood-tinged discharge) |
|
|
What is the most common presentation of male breast cancer? |
Painless breast mass |
|
|
How is breast cancer in men diagnosed? |
Biopsy and mammogram |
|
|
What is the treatment of male breast cancer? |
1. Mastectomy 2. Sentinel LN dissection of clinically negative axilla 3. Axillary dissection if clinically positive axillary LN |
|
|
What is the most common cause of green, straw-colored, or brown nipple discharge? |
Fibrocystic disease |
|
|
What is the most common cause of breast mass after breast trauma? |
Fat necrosis |
|
|
What is Mondor's disease? |
Thrombophlebitis of superficial breast veins |
|
|
What must be ruled out with spontaneous galactorrhea (+/- amenorrhea)? |
Prolactinoma (check pregnancy test and prolactin level) |
|
|
What is cystosarcoma phyllodes? |
Mesenchymal tumor arising from breast lobular tissue; most are benign
Note: "sarcoma" is a misnomer, as the vast majority are benign, 1% of breast cancers |
|
|
What is the usual age of the patient with cystosarcoma phyllodes? |
35-55 years (usually older than the patient with fibroadenoma) |
|
|
What are the signs/symptoms of cystosarcoma phyllodes? |
Mobile, smooth breast mass that resembles a fibroadenoma on exam, mammogram / ultrasound findings |
|
|
How do you diagnose cystosarcoma phyllodes? |
Through core biopsy or excision |
|
|
What is the treatment of cystosarcoma phyllodes? |
- If benign, wide local excision - If malignant, simple total mastectomy |
|
|
What is the role of axillary dissection with cystosarcoma phyllodes tumor? |
Only if clinically palpable axillary nodes, as the malignant form rarely spreads to nodes (most common site of metastasis is the lung) |
|
|
Is there a role for chemotherapy with cystosarcoma phyllodes? |
Consider it if large tumor (>5 cm) and "stromal overgrowth" |
|
|
What is fibroadenoma? |
Benign tumor of the breast consisting of stromal overgrowth, collagen arranged in "swirls" |
|
|
What is the clinical presentation of a fibroadenoma? |
Solid, mobile, well-circumscribed round breast mass, usually <40 years of age |
|
|
How is fibroadenoma diagnosed? |
- Negative needle aspiration looking for fluid - Ultrasound - Core biopsy |
|
|
What is the treatment for fibroadenoma? |
Surgical resection for large or growing lesions; small fibroadenomas can be observed closely |
|
|
What is a fibroadenoma's claim to fame? |
Most common breast tumor in women <30 years |
|
|
What is fibrocystic disease of the breast? |
Common benign breast condition consisting of fibrous (rubbery) and cystic changes in the breast |
|
|
What are the signs / symptoms of fibrocystic disease of the breast? |
Breast pain or tenderness that varies with the menstrual cycle; cysts; and fibrous ("nodular") fullness |
|
|
How is fibrocystic disease of the breast diagnosed? |
Through breast exam, history, and aspirated cysts (usually straw-colored or green fluid) |
|
|
What is the treatment for symptomatic fibrocystic disease? |
- Stop caffeine - Pain meds (NSAIDs) - Vitamin E, evening primrose oil (danazol and OCP as last resort) |
|
|
What is done if the patient has a breast cyst? |
- Needle drainage: if aspirate is bloody or a palpable mass remains after aspiration, an open boipsy is performed - If the aspirate is straw colored or green, the patient is followed closely; then, if there is recurrence, a second aspiration is performed - Re-recurrence usually requires open biopsy |
|
|
What is mastitis? |
Superficial infection of the breast (cellulitis) |
|
|
In what circumstances does mastitis most often occur? |
Breast-feeding |
|
|
What bacteria are most commonly causing mastitis? |
S. aureus |
|
|
How is mastitis treated? |
Stop breast-feeding and use a breast pump instead; apply heat; administer antibiotics |
|
|
Why must the patient with mastitis have close follow-up? |
To make sure that she does not have inflammatory breast cancer! |
|
|
What are the causes of breast abscesses? |
- Mammary ductal ectasia (stenosis of breast duct) - Mastitis |
|
|
What is the most common bacteria to cause breast abscess? |
- Nursing = S. aureus - Non-lactating = mixed infection |
|
|
What is the treatment of breast abscess? |
- Antibiotics (Eg, dicloxacillin) - Needle or open drainage with cultures taken - Resection of involved ducts if recurrent - Breast pump if breast-feeding |
|
|
What is lactational mastitis? |
Infection of the breast during breastfeeding - most commonly caused by S. aureus; treat with antibiotics and follow for abscess formation |
|
|
What must be ruled out with a breast abscess in a non-lactating woman? |
Breast cancer! |
|
|
What is male gynecomastia? |
Enlargement of the male breast |
|
|
What are the causes of male gynecomastia? |
- Meds - Illicit drugs (marijuana) - Liver failure - Increased estrogen - Decreased testosterone |
|
|
What is the major differential diagnosis for male gynecomastia in the older patient? |
Male breast cancer |
|
|
What is the treatment of male gynecomastia? |
- Stop or change medications - Correct underlying cause if there is a hormonal imbalance - Perform biopsy or subcutaneous mastectomy (ie, leave nipple) if refractory to conservative measures and time |

