![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
170 Cards in this Set
- Front
- Back
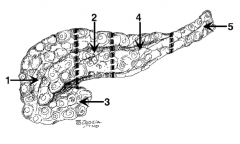
What is the name of region 1? |
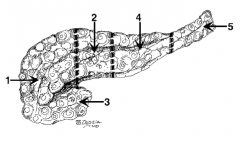
Head |
|
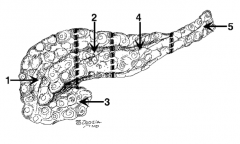
What is the name of region 2? |
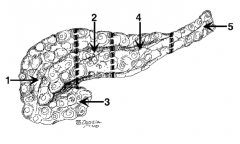
Neck (in front of the SMV) |
|
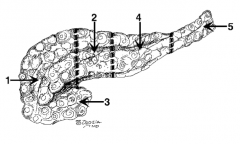
What is the name of region 3? |
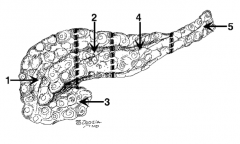
Uncinate process |
|
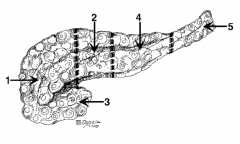
What is the name of region 4? |
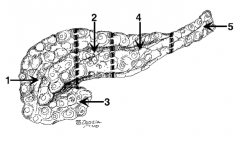
Body |
|
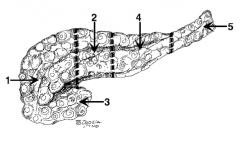
What is the name of region 5? |
Tail |
|
|
What structure is the tail of the pancreas said to "tickle"? |
Spleen |
|
|
What are the two pancreatic ducts? |
1. Wirsung duct 2. Santorini duct |
|
|
Which pancreatic duct is the main duct? |
Duct of Wirsung is the major duct Think: Santorini = Small duct |
|
|
How is blood supplied to the head of the pancreas? |
1. Celiac trunk --> gastroduodenal --> anterior superior pancreaticoduodenal artery and posterior superior pancreaticoduodenal artery
2. Superior mesentery artery --> anterior inferior pancreaticoduodenal artery and posterior inferior pancreaticoduodenal artery
3. Splenic artery --> dorsal pancreatic artery |
|
|
What is the source of the anterior superior pancreaticoduodenal artery? |
Celiac trunk --> gastroduodenal --> anterior superior pancreaticoduodenal artery |
|
|
What is the source of the posterior superior pancreaticoduodenal artery? |
Celiac trunk --> gastroduodenal --> posterior superior pancreaticoduodenal artery |
|
|
What is the source of the anterior inferior pancreaticoduodenal artery? |
Superior mesenteric artery --> anterior inferior pancreaticoduodenal artery |
|
|
What is the source of the posterior inferior pancreaticoduodenal artery? |
Superior mesenteric artery --> posterior inferior pancreaticoduodenal artery |
|
|
What is the source of the dorsal pancreatic artery? |
Splenic artery --> dorsal pancreatic artery |
|
|
Why must the duodenum be removed if the head of the pancreas is removed? |
They share the same blood supply (gastroduodenal artery) |
|
|
What is the endocrine function of the pancreas? |
Islets of Langerhans: - α-cells: glucagon - β-cells: insulin |
|
|
What is the exocrine function of the pancreas? |
Digestive enzymes: - Amylase - Lipase - Trypsin - Chymotrypsin - Carboxypeptidase |
|
|
What maneuver is used to mobilize the duodenum and pancreas and evaluate the entire pancreas? |
Kocher maneuver: incise the lateral attachments of the duodenum and then lift the pancreas to examine the posterior surface |
|
|
What is acute pancreatitis? |
Inflammation of the pancreas |
|
|
What are the most common etiologies in the US? |
1. Alcohol abuse (50%) 2. Gallstones (30%) 3. Idiopathic (10%) |
|
|
What is the acronym to remember all of the causes of pancreatitis? |
"I GET SMASHED": - Idiopathic
- Gallstones - Ethanol - Trauma
- Scorpion bite - Mumps (viruses) - Auto-immune - Steroids - Hyperlipidemia - ERCP - Drugs |
|
|
What are the symptoms of pancreatitis? |
Epigastric pain (frequently radiates to back); nausea and vomiting |
|
|
What are the signs of pancreatitis? |
- Epigastric tenderness - Diffuse abdominal tenderness - Decreased bowel sounds (adynamic ileus) - Fever - Dehydration / shock |
|
|
What is the differential diagnosis for a patient you suspect of having pancreatitis? |
- Gastritis / PUD - Perforated viscus - Acute cholecystitis - SBO - Mesenteric ischemia / infarction - Ruptured AAA - Biliary colic - Inferior MI / pneumonia |
|
|
What lab tests should be ordered for a patient you suspect of having pancreatitis? |
- CBC - LFT - Amylase and lipase - Type and cross - ABG - Calcium - Chemistry - Coags - Serum lipids |
|
|
What are the associated lab findings of pancreatitis? |
- High amylase - High lipase - High WBC |
|
|
What are the associated abdominal x-ray findings of pancreatitis? |
- Sentinel loop (most common sign) - Colon cutoff - Possibly gallstones (only 10% visible on x-ray) |
|
|
What are the associated ultrasound findings of pancreatitis? |
- Phlegmon - Cholelithiasis |
|
|
What are the associated CT findings of pancreatitis? |
- Phelgmon - Pancreatic necrosis |
|
|
What is the treatment of for pancreatitis? |
- NPO - IVF - NGT if - ± TPN vs post-pyloric tube feeds - H2 blocker / PPI - Analgesia (Demerol, not morphine - less sphincter of Oddi spasm) - Correction of coags / electrolytes - ± Alcohol withdrawal prophylaxis - "Tincture of time" |
|
|
What are the possible complications of pancreatitis? |
- Pseudocyst - Abscess / infection - Pancreatic necrosis - Splenic / mesenteric / portal vessel rupture or thrombosis - Pancreatic ascites / pancreatic pleural effusion - Diabetes - ARDS / sepsis / MOF - Coagulopathy / DIC - Encephalopathy - Severe hypocalcemia |
|
|
What is the prognosis for pancreatitis? |
Based on Ranson's criteria |
|
|
Are post-pyloric tube feeds safe in acute pancreatitis? |
Yes |
|
|
What are Ranson's criteria at presentation? |
1. Age >55 2. WBC >16,000 3. Glucose >200 4. AST >250 5. LDH >350 |
|
|
What are Ranson's criteria during the initial 48 hours? |
1. Base deficit >4 2. BUN increase >5 mg/dL 3. Fluid sequestration >6L 4. Serum Ca2+ <8 5. Hct decrease >10% 6. PO2 (ABG) <60 mmHg (amylase value is NOT one of Ranson's criteria) |
|
|
What is the mortality rate if a patient has 0-2 positive Ranson's criteria? |
<5% |
|
|
What is the mortality rate if a patient has 3-4 positive Ranson's criteria? |
~15% |
|
|
What is the mortality rate if a patient has 5-6 positive Ranson's criteria? |
~40% |
|
|
What is the mortality rate if a patient has 7-8 positive Ranson's criteria? |
~100% |
|
|
How can the admission Ranson criteria be remembered? |
GA LAW (Georgia Law): - Glucose >200 - Age >55
- LDH >350 - AST >250 - WBC >16,000
"Don't mess with the pancreas and don't mess with the Georgia law!" |
|
|
How can the Ranson criteria at <48 hours be remembered? |
C HOBBS (Calvin and Hobbes): - Calcium <8 mg/dL
- Hct drop >10% - O2 <60 (PaO2) - Base deficit >4 - BUN >5 increase - Sequestration >6L |
|
|
How can the AST vs LDH values in Ranson's criteria be remembered? |
Alphabetically and numerically: A before L and 250 before 350
Therefore, AST >250 and LDH >350 |
|
|
What is the etiology of hypocalcemia with pancreatitis? |
Fat saponification: fat necrosis binds to calcium |
|
|
What complication is associated with splenic vein thormbosis? |
Gastric varices (treatment with splenectomy) |
|
|
Can TPN with liquids be given to a patient with pancreatitis? |
Yes, if the patient does not suffer from hyperlipidemia (TG <300) |
|
|
What is the least common cause of acute pancreatitis (and possibly the most commonly asked about cause on rounds)? |
Scorpion bite (found on the island of Trinidad) |
|
|
What is chronic pancreatitis? |
Chronic inflammation of the pancreas region causing destruction of the parenchyma, fibrosis, and calcification, resulting in loss of endocrine and exocrine tissue |
|
|
What are the subtypes of chronic pancreatitis? |
1. Chronic calcific pancreatitis 2. Chronic obstructive pancreatitis (5%) |
|
|
What are the causes of chronic pancreatitis? |
- Alcohol abuse (most common, 70% of cases) - Idiopathic (15%) - Hypercalcemia (hyperparathyroidism) - Hyperlipidemia - Familial (found in families without any other risk factors) - Trauma - Iatrogenic - Gallstones |
|
|
What are the symptoms of chronic pancreatitis? |
Epigastric and/or back pain, weight loss, steatorrhea |
|
|
What are the associated signs of chronic pancreatitis? |
- Type I diabetes mellitus (up to 1/3) - Steatorrhea (up to 1/4) - Weight loss |
|
|
What are the signs of pancreatic exocrine insufficiency? |
- Steatorrhea (fat malabsorption from lipase insufficiency - stools float in water) - Malnutrition |
|
|
What are the signs of pancreatic endocrine insufficiency? |
Diabetes (glucose intolerance) |
|
|
What are the common pain patterns of chronic pancreatitis? |
- Unrelenting pain - Recurrent pain |
|
|
What is the differential diagnosis of chronic pancreatitis? |
- PUD - Biliary tract disease - AAA - Pancreatic cancer - Angina |
|
|
What percentages of patients with chronic pancreatitis have or will develop pancreatic cancer? |
~2% |
|
|
What are the appropriate lab tests to diagnose chronic pancreatitis? |
- Amylase / lipase - 72-hour fecal fat analysis - Glucose tolerance test (IDDM) |
|
|
Why may amylase / lipase be normal in a patient with chronic pancreatitis? |
Because of extensive pancreatic tissue loss ("burned-out pancreas") |
|
|
What radiographic tests should be performed in patients with chronic pancreatitis? |
- CT - KUB - ERCP |
|
|
What is the utility of CT for diagnosing chronic pancreatitis? |
Has greatest sensitivity for gland enlargement / atrophy, calcifications, masses, pseudocysts |
|
|
What is the utility of KUB for diagnosing chronic pancreatitis? |
Recognizes calcification in the pancreas |
|
|
What is the utility of ERCP for diagnosing chronic pancreatitis? |
Recognizes ductal irregularities with dilation and stenosis (Chain of Lakes), pseudocysts |
|
|
What is the medical treatment of chronic pancreatitis? |
- Discontinuation of alcohol use - can reduce attacks, though parenchymal damage continues secondary to ductal obstruction and fibrosis - Insulin for T1DM - Pancreatic enzyme replacement - Narcotics for pain |
|
|
What is the surgical treatment of chronic pancreatitis? |
- Puestow: longitudinal pancreaticojejunostomy (pancreatic duct must be dilated) - Duval: distal pancreaticojejunostomy - Near-total pancreatectomy |
|
|
What is the Frey procedure? |
Longitudinal pancreaticojejunostomy with core resection of the pancreatic head |
|
|
What is the indication for surgical treatment of chronic pancreatitis? |
Severe, prolonged / refractory pain |
|
|
What are the possible complications of chronic pancreatitis? |
- Insulin dependent diabetes mellitus - Steatorrhea - Malnutrition - Biliary obstruction - Splenic vein thrombosis - Gastric varices - Pancreatic pseudocyst / abscess - Narcotic addiction - Pancreatic ascites / pleural effusion - Splenic artery aneurysm |
|
|
What is gallstone pancreatitis? |
Acute pancreatitis from a gallstone in or passing through the ampulla of Vater (the exact mechanism is unknown) |
|
|
How is the diagnosis of gallstone pancreatitis made? |
Acute pancreatitis and cholelithiasis and/or choledocholithiasis and no other cause of pancreatitis (eg, no history of alcohol abuse) |
|
|
What radiologic tests should be performed to diagnose gallstone pancreatitis? |
- U/S to look for gallstones - CT to look at the pancreas, if symptoms are severe |
|
|
What is the treatment of gallstone pancreatitis? |
Conservative measurements and early interval cholecystectomy (laparoscopic cholecystectomy or open cholecystectomy) and intraoperative cholangiogram (IOC) 3 to 5 days (after pancreatic inflammation resolves) |
|
|
Why should early interval cholecystectomy be performed on patients with gallstone pancreatitis? |
Pancreatitis will recur in ~33% of patients within 8 weeks (so always perform early interval cholecystectomy and IOC in 3-5 days when pancreatitis resolves) |
|
|
What is the role of ERCP for gallstone pancreatitis? |
1. Cholangitis 2. Refractory choledocholithiasis |
|
|
What is hemorrhagic pancreatitis? |
Bleeding into the parenchyma and retroperitoneal structures with extensive pancreatic necrosis |
|
|
What are the signs of hemorrhagic pancreatitis? |
- Abdominal pain - Shock / ARDS - Cullen's sign - Grey Turner's sign - Fox's sign |
|
|
What is Cullen's sign? |
Bluish discoloration of the periumbilical area from retroperitoneal hemorrhage tracking around to the anterior abdominal wall through fascial planes
Sign of hemorrhagic pancreatitis |
|
|
What is Grey Turner's sign? |
Ecchymosis or discoloration of the flank in patients with retroperitoneal hemorrhage from dissecting blood from the retroperitoneum
Think: Grey TURNer = TURN side to side = flank hematoma
Sign of hemorrhagic pancreatitis |
|
|
What is Fox's sign? |
Ecchymosis of the inguinal ligament from blood tracking from the retroperitoneum and collecting at the inguinal ligament
Sign of hemorrhagic pancreatitis |
|
|
What are the significant lab values associated with hemorrhagic pancreatitis? |
- Increased amylase / lipase - Decreased Hct - Decreased calcium levels |
|
|
What radiologic test should be performed in patients to diagnose hemorrhagic pancreatitis? |
CT scan with IV contrast |
|
|
What is a pancreatic abscess? |
Infected peri-pancreatic purulent fluid collection |
|
|
What are the signs / symptoms of pancreatic abscess? |
- Fever - Unresolving pancreatitis - Epigastric mass |
|
|
What radiographic tests should be performed to diagnose pancreatic abscess? |
Abdominal CT with needle aspiration --> send for Gram stain / culture |
|
|
What are the associated lab findings for pancreatic abscess? |
Positive Gram stain and culture of bacteria |
|
|
Which organisms are found in pancreatic abscesses? |
- Gram negative (most common): E. coli, Pseudomonas, Klebsiella - Gram positive: S. aureus, Candida |
|
|
What is the treatment of a pancreatic abscess? |
Antibiotics and percutaneous drain placement or operative débridement and placement of drains |
|
|
What is pancreatic necrosis? |
Dead pancreatic tissue, usually following acute pancreatitis |
|
|
How do you diagnose pancreatic necrosis? |
Abdominal CT with IV contrast; dead pancreatic tissue does not take up IV contrast and is not enhanced on CT scan (ie, it does not "light up") |
|
|
What is the treatment of sterile pancreatic necrosis? |
Medical management |
|
|
What is the treatment of pancreatic necrosis suspicious for infection? |
CT guided fine needle aspiration |
|
|
What is the treatment of pancreatic necrosis in patient who is toxic / hypotensive? |
Operative débridement |
|
|
What is a pancreatic pseudocyst? |
Encapsulated collection of pancreatic fluid |
|
|
What makes a pancreatic pseudocyst a "pseudo" cyst? |
Wall is formed by inflammatory fibrosis, NOT epithelial cell lining |
|
|
What is the incidence of pancreatic pseudocyst? |
~1 in 10 after alcoholic pancreatitis |
|
|
What are the associated risk factors for pancreatic pseudocyst? |
Acute pancreatitis < chronic pancreatitis from alcohol |
|
|
What is the most common cause of pancreatic pseudocyst in the US? |
Chronic alcoholic pancreatitis |
|
|
What are the symptoms of pancreatic pseudocyst? |
- Epigastric pain / mass - Emesis - Mild fever - Weight loss
Note: should be suspected when a patient with acute pancreatitis fails to resolve pain |
|
|
What are the signs of pancreatic pseudocyst? |
- Palpable epigastric mass - Tender epigastrium - Ileus |
|
|
What lab tests should be performed in a patient you suspect of having pancreatic pseudocyst? |
- Amylase / lipase - Bilirubin - CBC |
|
|
What are the lab findings for pancreatic pseudocyst? |
- High amylase - Leukocytosis - High bilirubin (if there is obstruction) |
|
|
What are the U/S findings for pancreatic pseudocyst? |
Fluid-filled mass |
|
|
What are the CT findings for pancreatic pseudocyst? |
Fluid-filled mass, good for showing multiple cysts |
|
|
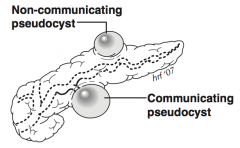
What are the ERCP findings for pancreatic pseudocyst? |
Radiopaque contrast material fills cyst if there is a communicating pseudocyst (ie, pancreatic duct communicates with pseudocyst) |
|
|
What is the differential diagnosis of a pancreatic pseudocyst? |
- Cystadenocarcinoma - Cystadenoma |
|
|
What are the possible complications of a pancreatic pseudocyst? |
- Infection - Bleeding into cyst - Fistula - Pancreatic ascites - Gastric outlet obstruction - SBO - Biliary obstruction |
|
|
What is the treatment for pancreatic pseudocyst? |
Drainage of the cyst or observation |
|
|
What is the waiting period before a pseudocyst should be drained? |
It takes 6 weeks for pseudocyst walls to "mature" or become firm enough to hold sutures and most will resolve in this time period of time if they are going to |
|
|
What percentage of pancreatic pseudocysts resolve spontaneously? |
~50% |
|
|
What is the treatment for pancreatic pseudocyst with bleeding into cyst? |
Angiogram and embolization |
|
|
What is the treatment for pancreatic pseudocyst with infection? |
Percutaneous external drainage / IV antibiotics |
|
|
What size pseudocyst should be drained? |
Most experts say: - Pseudocysts >5 cm have a small chance of resolving and have a higher chance of complications - Calcified cyst wall - Thick cyst wall |
|
|
What are three treatment options for pancreatic pseudocyst? |
1. Percutaneous aspiration / drain 2. Operative drainage 3. Transpapillary stent via ERCP (pseudocyst must communicate with pancreatic duct) |
|
|
What are the surgical options for pancreatic pseudocyst adherent to the stomach? |
Cystogastrostomy (drain into the stomach) |
|
|
What are the surgical options for pancreatic pseudocyst adherent to the duodenum? |
Cystoduodenostomy (drain into the duodenum) |
|
|
What are the surgical options for pancreatic pseudocyst not adherent to the stomach or duodenum? |
Roux-en-Y cystojejunostomy (drain into the Roux limb of jejunum) |
|
|
What are the surgical options for pancreatic pseudocyst in the tail of the pancreas? |
Resection of the pancreatic tail with the pseudocyst |
|
|
What is an endoscopic option for drainage of a pancreatic pseudocyst? |
Endoscopic cystogastrostomy |
|
|
What must be done during a surgical procedure for a pancreatic pseudocyst? |
Biopsy of the cyst wall to rule out a cystic carcinoma (eg, cystadenocarcinoma) |
|
|
What is the most common cause of death due to pancreatic pseudocyst? |
Massive hemorrhage into the pseudocyst |
|
|
What is pancreatic carcinoma? |
Adenocarcinoma of the pancreas arising from duct cells |
|
|
What are the associated risk factors for pancreatic carcinoma? |
- Smoking 3x risk - Diabetes mellitus - Heavy alcohol use - Chronic pancreatitis - Diet high in fried meats - Previous gastrectomy |
|
|
What is the male to female ratio for incidence of pancreatic carcinoma? |
3:2 |
|
|
What is the African American to white ratio for incidence of pancreatic carcinoma? |
2:1 |
|
|
What is the average for onset of pancreatic carcinoma? |
>60 years |
|
|
What are the different types of pancreatic carcinoma? |
>80% are duct cell adenocarcinomas; other types include cystadenocarcinoma and acinar cell carcinoma |
|
|
Where are pancreatic carcinomas commonly found? |
- 66% arise in the pancreatic head - 33% arise in the body and tail |
|
|
Why are most pancreatic carcinomas in the tail non-resectable? |
These tumors grow without symptoms until it is too late and they have already spread - head of the pancreas tumors draw attention earlier because of biliary obstruction |
|
|
What are the signs/symptoms of pancreatic tumors in the head of the pancreas? |
- Painless jaundice from obstruction of common bile duct - Weight loss - Abdominal pain - Back pain - Weakness - Pruritus from bile salts in skin - Anorexia - Courvoisier's sign - Acholic stools - Dark urine - Diabetes |
|
|
What are the signs/symptoms of pancreatic tumors in the body or tail of the pancreas? |
- Weight loss and pain (90%) - Migratory thrombophlebitis (10%) - Jaundice (<10%) - Nausea and vomiting - Fatigue |
|
|
What are the most common symptoms of cancer of the pancreatic HEAD? |
1. Weight loss (90%) 2. Pain (75%) 3. Jaundice (70%) |
|
|
What is "Courvoisier's sign"? |
Palpable, nontender, distended gallbladder |
|
|
What percentage of patients with cancers of the pancreatic head have Courvoisier's sign? |
33% |
|
|
What is the classic presentation of pancreatic cancer in the head of the pancreas? |
Painless jaundice |
|
|
What metastatic lymph nodes described classically for gastric cancer can be found with metastatic pancreatic cancer? |
- Virchow's node - Sister Mary Joseph's nodule |
|
|
What are the associated lab findings of pancreatic carcinoma? |
- Increased direct bilirubin and alkaline phosphatase (as a result of biliary obstruction) - Increased LFTs - Elevated pancreatic tumor markers |
|
|
Which tumor markers are associated with pancreatic carcinoma? |
CA 19-9 |
|
|
What does CA 19-9 stand for? |
Carbohydrate Antigen 19-9 |
|
|
What diagnostic studies are performed for patients suspected of having pancreatic carcinoma? |
- Abdominal CT - Ultrasound - Cholangiography (ERCP to rule out choledocholithiasis and cell brushings) - Endoscopic U/S with biopsy |
|
|
What are the characteristics of pancreatic cancer stage I? |
Tumor is limited to pancreas, with no nodes or metastases |
|
|
What are the characteristics of pancreatic cancer stage II? |
Tumor extends into bile duct, peripancreatic tissues, or duodenum; there are no nodes or metastases |
|
|
What are the characteristics of pancreatic cancer stage III? |
Same findings as stage II plus positive nodes or celiac or SMA involvement |
|
|
What are the characteristics of pancreatic cancer stage IVA? |
Tumor extends to stomach, colon, spleen, or major vessels, with any nodal status and no distant metastases |
|
|
What are the characteristics of pancreatic cancer stage IVB? |
Distant metastases (any nodal status, any tumor size) are found |
|
|
What is the treatment of pancreatic cancer found in the head? |
Whipple procedure (pancreaticoduodenectomy) |
|
|
What is the treatment of pancreatic cancer found in the body or tail? |
Distal resection |
|
|
What factors of pancreatic carcinoma signify inoperability? |
- Vascular encasement (SMA, hepatic artery) - Liver metastasis - Peritoneal implants - Distant lymph node metastasis (periaortic / celiac nodes) - Distant metastasis - Malignant ascites |
|
|
Is portal vein or SMV involvement an absolute contraindication for resection? |
No - can be resected and reconstructed with vein interposition graft at soem centers |
|
|
Should patients undergo pre-op biliary drainage (eg, ERCP) for pancreatic carcinoma? |
No (exceptions for symptoms / preoperative XRT, trials, etc) |
|
|
What occurs in a Whipple procedure? |
- Cholecystectomy - Truncal vagotomy - Antrectomy - Pancreaticoduodenectomy (removal of head of pancreas and duodenum) - Choledochojejunostomy (anastomosis of common bile duct to jejunum) - Pancreaticojejunostomy (anastomosis of distal pancreas remnant to jejunum) - Gastrojejunostomy (anastomosis of stomach to jejunum) |
|
|
What is the complication rate after a Whipple procedure? |
25% |
|
|
What mortality rate is associated with a Whipple procedure? |
<5% at busy centers |
|
|
What is the pylorus-preserving Whipple? |
No antrectomy; anastomose duodenum to jejunum |
|
|
What are the possible post-Whipple complications? |
- Delayed gastric emptying (if antrectomy is performed) - Anastomotic leak (from bile duct or pancreatic anastomosis), causing pancreatic / biliary fistula - Wound infection - Post-gastrectomy syndromes - Sepsis - Pancreatitis |
|
|
Why must the duodenum be removed if the head of the pancreas is resected? |
They share the same blood supply |
|
|
What ist he post-op adjuvant therapy for pancreatic carcinoma? |
Chemotherapy +/- XRT |
|
|
What is the palliative treatment if the tumor is inoperable and biliary obstruction is present? |
PTC or ERCP and placement of stent across obstruction |
|
|
What is the prognosis for pancreatic carcinoma at 1 year after diagnosis? |
Dismal; 90% of patients die within 1 year of diagnosis |
|
|
What is the survival rate for pancreatic carcinoma at 5 year after resection? |
20% |
|
|
What is an annular pancreas? |
Pancreas encircling the duodenum; if obstruction is present, bypass, do not resect |
|
|
What is pancreatic divisum? |
Failure of the two pancreatic ducts to fuse; the normally small duct (Santorini) acts as the main duct
Think: Divisum = Divided |
|
|
What is heterotopic pancreatic tissue? |
Heterotopic pancreatic tissue usually is found in the stomach, intestine, or duodenum |
|
|
What is a Puestow procedure? |
Longitudinal filleting of the pancreas / pancreatic duct with a side-to-side anastomosis with the small bowel |
|
|
What medication decreases output from a pancreatic fistula? |
Somatostatin (GI-inhibitory hormone) |
|
|
Which has a longer half-life: amylase or lipase? |
Lipase; therefore amylase may be normal and lipase will remain elevated longer |
|
|
What is WDHA syndrome? |
Pancreatic VIPoma (Vasoactive Intestinal Polypeptide tumor)
Also known as Verner-Morrison syndrome
Tumor secretes VIP, which causes: - Watery - Diarrhea - Hypokalemia - Achlorhydria (inhibits gastric acid secretion) |
|
|
What is the Whipple triad of pancreatic insulinoma? |
1. Hypoglycemia (glucose <50) 2. Symptoms of hypoglycemia: mental status changes / vasomotor instability 3. Relief of symptoms with administration of glucose |
|
|
What is the most common islet cell tumor? |
Insulinoma |
|
|
|
Somatostatinoma (inhibits gallbladder contraction) |
|
|
What is the triad found with pancreatic somatostatinoma tumor? |
1. Gallstones 2. Diabetes 3. Steatorrhea |
|
|
What are the two classic findings with pancreatic glucagonoma tumors? |
1. Diabetes 2. Dermatitis / rash (necrotizing migratory erythema) |

