![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
168 Cards in this Set
- Front
- Back

What is structure 1? |
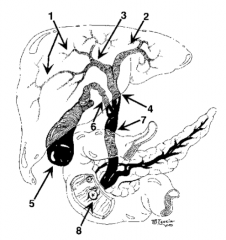
Intrahepatic ducts |
|
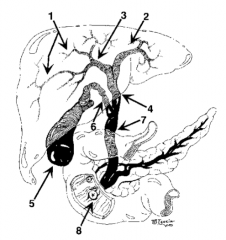
What is structure 2? |
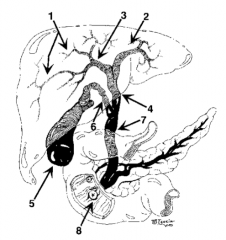
Left hepatic duct |
|
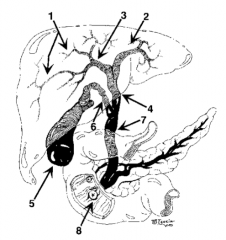
What is structure 3? |
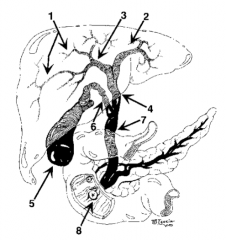
Right hepatic duct |
|
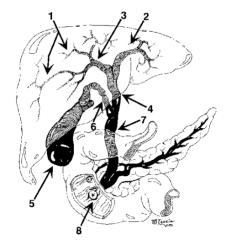
What is structure 4? |

Common hepatic duct |
|
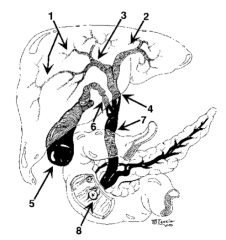
What is structure 5? |
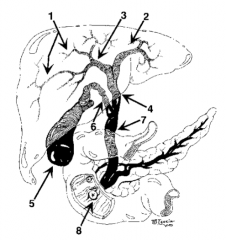
Gallbladder |
|
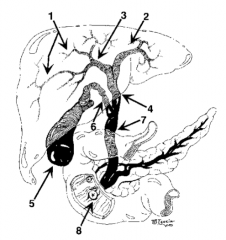
What is structure 6? |

Cystic Duct |
|
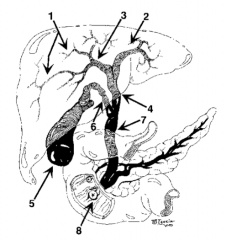
What is structure 7? |
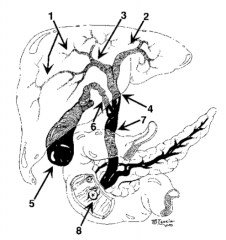
Common bile duct |
|
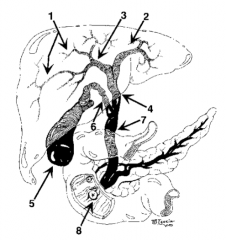
What is structure 8? |
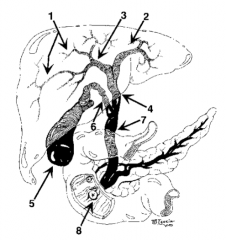
Ampulla of Vater |
|
|
What is the proximal and which is the distal bile duct? |
Proximal is close to the liver (bile and the liver is analogous to blood and the heart; they both flow distally) |
|
|
What is the name of the node in Calot's triangle? |
Calot's node |
|
|
What are the small ducts that drain bile directly into the gallbladder from the liver? |
Ducts of Luschka |
|
|
Which artery is susceptible to injury during cholecystectomy? |
Right hepatic artery, because of its proximity to the cystic artery and Calot's triangle |
|
|
What is the name of the valves of the gallbladder? |
Spiral valves of Heister |
|
|
Where is the infundibulum of the gallbladder? |
Near the cystic duct |
|
|
Where is the fundus of the gallbladder? |
At the end of the gallbladder |
|
|
What is "Hartmann's pouch"? |
Gallbladder infundibulum |
|
|
What are the boundaries of the triangle of Calot? |
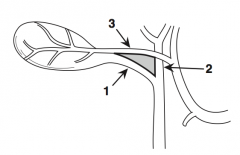
The 3 C's: 1. Cystic duct 2. Common hepatic duct 3. Cystic artery |
|
|
What is the source of alkaline phosphatase? |
Bile duct epithelium; expect alk phos to be elevated in bile duct obstruction |
|
|
What is in bile? |
- Cholesterol - Lecithin (phospholipid) - Bile acids - Bilirubin |
|
|
What does bile do? |
Emulsifies fats |
|
|
What is the enterohepatic circulation? |
Circulation of bile acids from liver to gut and back to the liver |
|
|
Where are most of the bile acids absorbed? |
In the terminal ileum |
|
|
What stimulates gallbladder emptying? |
Cholecystokinin and vagal input |
|
|
What is the source of cholecystokinin? |
Duodenal mucosal cells |
|
|
What stimulates the release of cholecystokinin? |
- Fat - Protein - Amino acids - HCl |
|
|
What inhibits the release of cholecystokinin? |
- Trypsin - Chymotrypsin |
|
|
What are the actions of cholecystokinin? |
- Gallbladder emptying - Opening of ampulla of Vater - Slowing of gastric emptying - Pancreas acinar cell growth and release of exocrine products |
|
|
At what level of serum total bilirubin does one start to get jaundiced? |
>2.5 |
|
|
Classically, what is thought to be the anatomic location where one first finds evidence of jaundice? |
Under the tongue |
|
|
With good renal function, how high can the serum total bilirubin go? |
Very rarely, >20 |
|
|
What are the signs and symptoms of obstructive jaundice? |
- Jaundice - Dark urine - Clay-colored stools (acholic stools) - Pruritus (itching) - Loss of appetite - Nausea |
|
|
What causes the itching in obstructive jaundice? |
Bile salts in the dermis (not bilirubin) |
|
|
What is cholelithiasis? |
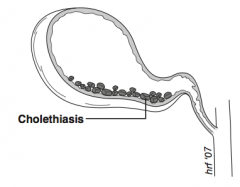
Gallstones in gallbladder |
|
|
What is choledocholithiasis? |
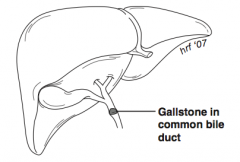
Gallstone in common bile duct |
|
|
What is cholecystitis? |
Inflammation of gallbladder |
|
|
What is cholangitis? |
Infection of biliary tract |
|
|
What is cholangiocarcinoma? |
Adenocarcinoma of bile ducts |
|
|
What is Klatskin's tumor? |
Cholangiocarcinoma of bile duct at the junction of the right and left hepatic ducts |
|
|
What is biliary colic? |
- Pain from gallstones, usually from a stone at cystic duct - The pain is located in RUQ, epigastrium, or right subscapular region of the back - It usually lasts minutes to hours but eventually goes away - It is often post-prandial, especially after fatty foods |
|
|
What is biloma? |
Intraperitoneal bile fluid collection |
|
|
What is choledochojejunostomy? |
Anastomosis between common bile duct and jejunum |
|
|
What is hepaticojejunostomy? |
Anastomosis of hepatic ducts or common hepatic duct to jejunum |
|
|
What is the initial diagnostic study of choice for evaluation of the biliary tract / gallbladder / cholelithiasis? |
Ultrasound |
|
|
What is an ERCP? |
Endoscopic Retrograde Cholangio-Pancreatography |
|
|
What is PTC? |
Percutaenous Transhepatic Cholangiogram |
|
|
What is IOC? |
Intra-Operative Cholangiogram (done laparoscopically or open to rule out choledocholithiasis) |
|
|
What is a HIDA/PRIDA scan? |
Radioisotope study; isotope concentrated in liver and secreted into bile; will demonstrate cholecystitis, bile leak, or CBD obstruction |
|
|
How does the HIDA scan reveal cholecystitis? |
Non-opacification of the gallbladder from obstruction of the cystic duct |
|
|
How often will plain x-ray films see gallstones? |
10-15% |
|
|
What is a cholecystectomy? |
Removal of the gallbladder laparoscopically or through a standard Kocher incision |
|
|
What is a lap chole? |
LAParoscopic CHOLEcystectomy |
|
|
What is the Kocher incision? |
Right subcostal incision |
|
|
What is a sphincterotomy? |
Cut through sphincter of Oddi to allow passage of gallstones from the common bile duct; most often done at ERCP; also known as papillotomy |
|
|
How should post-op biloma be treated after a lap chole? |
1. Percutaneous drain bile collection 2. ERCP with placement of biliary stent past leak (usually cystic duct remnant leak) |
|
|
What is the treatment of major CBD injury after a lap chole? |
Choledochojejunostomy |
|
|
What is obstructive jaundice? |
Jaundice (hyperbilirubinemia >2.5) from obstruction of bile flow to the duodenum |
|
|
What is the differential diagnosis of proximal bile duct obstruction? |
- Cholangiocarcinoma - Lymphadenopathy - Metastatic tumor - Gallbladder carcinoma - Sclerosing cholangitis - Gallstones - Tumor embolus - Parasites - Post-surgical stricture - Hepatoma - Benign bile duct tumor |
|
|
What is the differential diagnosis of distal bile duct obstruction? |
- Choledocholithiasis (gallstones) - Pancreatic carcinoma - Pancreatitis - Ampullary carcinoma - Lymphadenopathy - Pseudocyst - Post-surgical stricture - Ampulla of Vater dysfunction / stricture - Lymphoma - Benign bile duct tumor - Parasites |
|
|
What is the initial study of choice for obstructive jaundice? |
Ultrasound |
|
|
What lab results are associated with obstructive jaundice? |
- Elevated alk phos - Elevated bilirubin with or without elevated LFTs |
|
|
What is cholelithiasis? |
Formation of gallstones |
|
|
What is the incidence of cholelithiasis? |
~10% of US population will develop gallstones |
|
|
What are the big 4 risk factors for cholelithiasis? |
Four F's: - Female - Fat - Forty - Fertile (multiparity) |
|
|
What are other less common risk factors for gallstones? |
- Oral contraceptives - Bile stasis - Chronic hemolysis (pigment stones) - Cirrhosis - Infection - Native American heritage - Rapid weight loss / gastric bypass - Obesity - Inflammatory Bowel Disease (IBD) - Terminal ileal resection - Total parenteral nutrition (TPN) - Vagotomy - Advanced age - Hyperlipidemia - Somatostatin therapy |
|
|
What are the types of stones causing cholelithiasis? |
- Cholesterol stones (75%) - Pigment stones (25%) |
|
|
What are the types of pigmented stones? |
- Black stones (contain calcium bilirubinate) - Brown stones (associated with biliary tract infection) |
|
|
What are the causes of black-pigmented stones? |
Cirrhosis and hemolysis |
|
|
What is the pathogenesis of cholesterol stones? |
Secretion of bile supersaturated with cholesterol (relatively decreased amounts of lecithin and bile salts); then, cholesterol precipitates out and forms solid crystals, then gallstones |
|
|
Is hypercholesterolemia a risk factor for gallstone formation? |
No (but hyperlipidemia is) |
|
|
What are the signs / symptoms of cholelithiasis? |
- Biliary colic - Cholangitis - Choledocholithiasis - Gallstone - Pancreatitis |
|
|
Is biliary colic pain really "colic"? |
No, symptoms usually last for hours, therefore colic is a misnomer! |
|
|
What percentage of patients with gallstones are asymptomatic? |
80% of patients with cholelithiasis are asymptomatic |
|
|
What is thought to cause biliary colic? |
Gallbladder contraction against a stone temporarily at the gallbladder / cystic duct junction; a stone in the cystic duct; or a stone passing through the cystic duct |
|
|
What is Boas' sign? |
Referred right subscapular pain of biliary colic |
|
|
What are the five major complications of gallstones? |
1. Acute cholecystitis 2. Choledocholithaisis 3. Gallstone pancreatitis 4. Gallstone ileus 5. Cholangitis |
|
|
How is cholelithiasis diagnosed? |
- History - Physical exam - Ultrasound |
|
|
How often does ultrasound detect cholelithiasis? |
>98% of the time |
|
|
How often does ultrasound detect choledocholithiasis? |
About 33% of the time.. not a very good study for choledocholithiasis |
|
|
How are symptomatic or complicated cases of cholelithiasis treated? |
By cholecystectomy |
|
|
What are the possible complications of a lap chole? |
- Common bile duct injury - Right hepatic duct / artery injury - Cystic duct leak - Biloma (collection of bile) |
|
|
What are the indications for cholecystectomy in the asymptomatic patient? |
- Sickle cell disease - Calcified gallbladder (porcelain gallbladder) - Patient is a child |
|
|
Define IOC? |
Intra-Operative Cholangiogram (dye in bile duct by way of the cystic duct with fluoro / x-ray) |
|
|
What are the indications for an intraoperative cholangiogram? |
1. Jaundice 2. Hyperbilirubinemia 3. Gallstone pancreatitis (resolved) 4. Elevated alkaline phosphatase 5. Choledocholithiasis on ultrasound 6. To define anatomy |
|
|
What is choledocholithiasis? |
Gallstones in the common bile duct |
|
|
What is the management of choledocholithiasis? |
1. ERCP with papillotomy and basket / balloon retrieval of stones (pre- or post-operatively) 2. Laparoscopic transcystic duct or trans bile duct retrieval 3. Open common bile duct exploration |
|
|
What medication may dissolve a cholesterol gallstone? |
Chenodeoxycholic acid, Ursodeoxycholic acid (Actigall)
But if medication is stopped, gallstones often recur |
|
|
What is the major feared complication of ERCP? |
Pancreatitis |
|
|
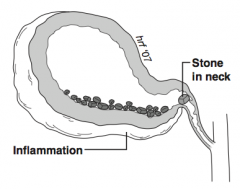
What is the pathogenesis of acute cholecystitis? |
Obstruction of cystic duct leads to inflammation of the gallbladder
95% of cases result from calculi 5% of cases result from acalculous obstruction |
|
|
What are the risk factors for acute cholecystitis? |
Gallstones |
|
|
What are the signs and symptoms of acute cholecystitis? |
- Unrelenting RUQ pain or tenderness - Fever - Nausea / vomiting - Painful palpable gallbladder in 33% - Positive Murphy's sign - Right subscapular pain (referred) - Epigastric discomfort (referred) |
|
|
What is Murphy's sign? |
Acute pain and inspiratory arrest elicited by palpation of the RUQ during inspiration |
|
|
What are the complications of acute cholecystitis? |
- Abscess - Perforation - Choledocholithiasis - Cholecystenteric fistula formation - Gallstone ileus |
|
|
What lab results are associated with acute cholecystitis? |
- Increased WBCs - May have slight elevation in alk phos and LFTs - May have slight elevation in amylase, total bili |
|
|
What is the diagnostic test of choice for acute cholecystitis? |
Ultrasound |
|
|
What are the signs of acute cholecystitis on ultrasound? |
- Thickened gallbladder wall (>3 mm) - Pericholecystic fluid - Distended gallbladder - Gallstones present / cystic duct stone - Sonographic Murphy's sign (pain on inspiration after placement of U/S probe over gallbladder) |
|
|
What ist he difference between acute cholecystitis and biliary colic? |
- Biliary colic has temporary pain - Acute cholecystitis has pain that does not resolve, usually with elevated WBCs, fever, and signs of acute inflammation on U/S |
|
|
What is the treatment of acute cholecystitis? |
- IVF - Antibiotics - Cholecystectomy early |
|
|
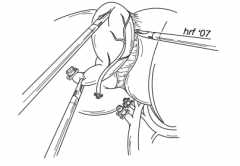
What are the steps in a lap chole? |
1. Dissection of peritoneum overlying the cystic duct and artery 2. Clipping of cystic artery and transect 3. Division of cystic duct between clips 4. Dissection of gallbladder from liver bed 5. Cauterization, irrigation, suction to obtain hemostasis of liver bed 6. Removal of gallbladder through umbilical trocar site |
|
|
How is an IOC performed? |
1. Place a clip on the cystic duct gallbladder junction 2. Cut a small hole in the distal cystic duct to cannulate 3. Inject half-strength contrast and take an x-ray or fluoro |
|
|
What percentage of patients has an accessory cystic artery |
10% |
|
|
Why should the gallbladder specimen be opened in the operating room? |
Looking for gallbladder cancer, anatomy |
|
|
What is acute acalculous cholecystitis? |
Acute cholecystitis without evidence of stones |
|
|
What is the pathogenesis of acute acalculous cholecystitis? |
It is believed to result from sludge and gallbladder disuse and biliary stasis, perhaps 2/2 to absence of cholecystokinin stimulation (decreased contraction of gallbladder) |
|
|
What are the risk factors for acute acalculous cholecystitis? |
- Prolonged fasting - TPN - Trauma - Multiple transfusions - Dehydration - Often occurs in prolonged post-op or ICU setting |
|
|
What are the diagnostic tests of choice for acute acalculous cholecystitis? |
1. U/S: sludge and inflammation usually present with acute acalculous cholecystitis 2. HIDA scan |
|
|
What are the findings in acute acalculous cholecystitis on HIDA scan? |
Non-filling of the gallbladder |
|
|
What is the management of acute acalculous cholecystitis? |
Cholecystectomy or cholecystostomy tube if the patient is unstable (placed percutaneously by radiology or open surgery) |
|
|
What is cholangitis? |
Bacterial infection of the biliary tract from obstruction (either partial or complete); potentially life-threatening |
|
|
What are the common causes of cholangitis? |
- Choledocholithiasis - Stricture (usually post-op) - Neoplasm (usually ampullary carcinoma) - Extrinsic compression (pancreatic pseudocyst / pancreatitis) - Instrumentation of the bile ducts (eg, PTC/ERCP) - Biliary stentW |
|
|
What is the most common cause of cholangitis? |
Gallstones in common bile duct (choledocholithiaisis) |
|
|
What are the signs/symptoms of cholangitis? |
- Charcot's triad: fever/chills, RUQ pain, and jaundice - Reynold's pentad: Charcot's triad + altered mental status + shock |
|
|
What lab results are associated with cholangitis? |
- Increased WBCs - Increased Bilirubin - Increased Alk Phos - Positive blood cultures |
|
|
Which organisms are most commonly isolated with cholangitis? |
- G- organisms (E. coli, Klebsiella, Pseudomonas, Enterobacter, Proteus, Serratia) most common - Enterococci is most common G+ - Anaerobes are less common (B. fragilis most frequent) - Fungi are even less common (Candida) |
|
|
What are the diagnostic tests of choice for cholangitis? |
U/S and contrast study (eg, ERCP or IOC) after patient has "cooled off" with IV antibiotics |
|
|
What is suppurative cholangitis? |
Severe infection with sepsis - "pus under pressure" |
|
|
What is the management of non-suppurative cholangitis? |
- IVF - Antibiotics - Definitive treatment later (eg, lap chole +/- ERCP) |
|
|
What is the management of suppurative cholangitis? |
- IVF - Antibiotics - Decompression: obtained by ERCP with papillotomy, PTC with catheter drainage, or laparotomy with T-tube placement |
|
|
What is sclerosing cholangitis? |
Multiple inflammatory fibrous thickenings of bile duct walls resulting in biliary strictures |
|
|
What is the natural history of sclerosing cholangitis? |
Progressive obstruction possibly leading to cirrhosis and liver failure; 10% of patients will develop cholangiocarcinoma |
|
|
What is the etiology of sclerosing cholangitis? |
Unknown, but probably auto-immune |
|
|
What is the major risk factor for sclerosing cholangitis? |
Inflammatory bowel disease - Ulcerative Colitis (~66%) |
|
|
What are the signs / symptoms of sclerosing cholangitis? |
Same as those for obstructive jaundice: - Jaundice - Itching (pruritus) - Dark urine - Clay-colored stools - Loss of energy - Weight loss - Many are asymptomatic |
|
|
What are the complications of sclerosing cholangitis? |
- Cirrhosis - Cholangiocarcinoma (10%) - Cholangitis - Obstructive jaundice |
|
|
How do you diagnose sclerosing cholangitis? |
Elevated alk phos, and PTC or ERCP revealing "beads on a string" appearance on contrast study |
|
|
What are the management options for sclerosing cholangitis? |
- Hepatoenteric anastomosis (if primarily extra-hepatic ducts are involved) and resection of extra-hepatic bile ducts because of the risk of cholangiocarcinoma - Transplant (if primarily intra-hepatic disease or cirrhosis) - Endoscopic balloon dilations |
|
|
What percentage of patients with IBD develops sclerosing cholangitis? |
<5% |
|
|
What is gallstone ileus? |
Small bowel obstruction from a large gallstone (>2.5 cm) that has eroded through the gallbladder and into the duodenum / small bowel |
|
|
What is the classic site of obstruction with gallstone ileus? |
Ileocecal valve (but may cause obstruction in the duodenum, sigmoid colon) |
|
|
What are the classic findings of gallstone ileus? |
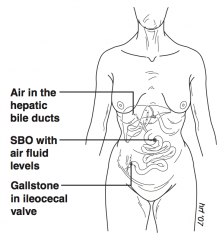
- Air in hepatic bile ducts - SBO with air fluid levels - Gallstone in ileocecal valve |
|
|
What is the population at risk for gallstone ileus? |
Gallstone ileus is most commonly seen in women older than 70 years |
|
|
What are the signs/symptoms of gallstone ileus? |
Symptoms of SBO: - Distention - Vomiting - Hypovolemia - RUQ pain |
|
|
Gallstone ileus causes what percentage of SBO? |
<1% |
|
|
What are the diagnostic tests of choice for gallstone ileus? |
- Abdominal x-ray - UGI - Abdominal CT |
|
|
What are the findings of gallstone ileus on abdominal x-ray? |
Occasionally reveals radiopaque gallstone in the bowel; 40% of patients show air in the biliary tract, small bowel distention, and air fluid levels secondary to ileus |
|
|
What are the findings of gallstone ileus on UGI? |
Used if diagnosis is in question; will show cholecystenteric fistula and the obstruction |
|
|
What are the findings of gallstone ileus on abdominal CT? |
Reveals air in biliary tract, SBO +/- gallstone in intestine |
|
|
What is the management of gallstone ileus? |
Surgery: enterotomy with removal of the stone +/- interval cholecystectomy (interval-delayed) |
|
|
What is carcinoma of the gallbladder? |
Malignant neoplasm arising int he gallbladder, vast majority are adenocarcinoma (90%) |
|
|
What are the risk factors for carcinoma of the gallbladder? |
- Gallstones - Porcelain gallbladder - Cholecystenteric fistula |
|
|
What is the female:male ratio for carcinoma of the gallbladder? |
4:1 |
|
|
What is the most common site of gallbladder cancer in the gallbladder? |
60% in fundus |
|
|
What is a porcelain gallbladder? |
Calcified gallbladder |
|
|
What percentage of patients with a porcelain gallbladder will have gallbladder cancer? |
~50% (20-60%) |
|
|
What is the incidence of carcinoma of the gallbladder? |
~1% of all gallbladder specimens |
|
|
What are the symptoms of carcinoma of the gallbladder? |
- Biliary colic - Weight loss - Anorexia - Many are asymptomatic until late - May present as acute cholecystiits |
|
|
What are the signs of carcinoma of the gallbladder? |
- Jaundice (from invasion of the common duct or compression by involved pericholedochal lymph nodes) - RUQ mass - Palpable gallbladder (advanced disease) |
|
|
What are the diagnostic tests of choice for carcinoma of the gallbladder? |
- U/S - Abdominal CT - ERCP |
|
|
What is the route of spread of carcinoma of the gallbladder? |
Contiguous spread to the liver is most common |
|
|
What is the management of carcinoma of the gallbladder that is confined to the mucosa? |
Cholecystectomy |
|
|
What is the management of carcinoma of the gallbladder that is confined to the muscularis/serosa? |
Radical cholecystectomy: cholecystectomy and wedge resection of overlying liver, and lymph node dissection +/- chemotherapy / XRT |
|
|
What is the main complication of a lap chole for gallbladder cancer? |
Trocar site tumor implants
Note: if known pre-operatively, perform open cholecystectomy |
|
|
What is the prognosis for gallbladder cancer? |
- Dismal overall: <5% 5-year survival as most are unresectable at diagnosis - T1 with cholecystectomy: 95% 5-year survival |
|
|
What is cholangiocarcinoma? |
Malignancy of the extrahepatic or intrahepatic ducts - primary bile duct cancer |
|
|
What is the histology of cholangiocarcinoma? |
Almost all are adenocarcinoma |
|
|
What is the average age at diagnosis for cholangiocarcinoma? Male female ratio? |
~65 years, equally affects male/female |
|
|
What are the signs/symptoms of cholangiocarcinoma? |
Those of biliary obstruction: - Jaundice - Pruritus - Dark urine - Clay colored stools - Cholangitis |
|
|
What is the most common location of cholangiocarcinoma? |
Proximal bile duct |
|
|
What are the risk factors for cholangiocarcinoma? |
- Choledochal cysts - Ulcerative colitis - Thorotrast contrast dye (used in 1950s) - Sclerosing cholangitis - Liver flukes (clonorchiasis) - Toxin exposures (eg, Agent Orange) |
|
|
What is a Klatskin tumor? |
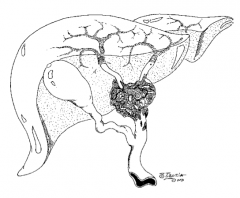
Tumor that involves the junction of the right and left hepatic ducts |
|
|
What are the diagnostic tests of choice for cholangiocarcinoma? |
- U/S - CT scan - ERCP / PTC with biopsy / brushings for cytology - MRCP |
|
|
What is an MRCP? |
MRI with visualization of pancreatic and bile ducts |
|
|
What is the management of proximal bile duct cholangiocarcinoma? |
Resection with Roux-en-Y hepaticojejunostomy (anastomose bile ducts to jejunum) +/- unilateral hepatic lobectomy |
|
|
What is the management of distal common bile duct cholangiocarcinoma? |
Whipple procedure |
|
|
What is a porcelain gallbladder? |
- Calcified gallbladder seen on abdominal x-ray - Results from chronic cholelithiasis / cholecystitis with calcified scar tissue in gallbladder wall - Cholecystectomy required because of the strong associated of gallbladder carcinoma with this condition |
|
|
What is hydrops of the gallbladder? |
Complete obstruction of the cystic duct by gallstone, with filling of the gallbladder with fluid (not bile) from the gallbladder mucosa |
|
|
What is Gilbert's syndrome? |
Inborn error in liver bilirubin uptake and glucuronyl transferase resulting in hyperbilirubinemia |
|
|
What is Courvoisier's gallbladder? |
- Palpable, nontender gallbladder (unlike gallstone disease) associated with cancer of the head of the pancreas - Able to distend because it has not been "scarred down" by gallstones |
|
|
What is Mirizzi's syndrome? |
Common hepatic duct obstruction as a result of extrinsic compression from a gallstone impacted in the cystic duct |

