![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
70 Cards in this Set
- Front
- Back
|
What is "TBSA"? |
Total Body Surface Area |
|
|
What is STSG? |
Split Thickness Skin Graft |
|
|
Are acid or alkali chemical burns more serious? |
In general, ALKALI burns are more serious because the body cannot buffer the alkali, thus allowing them to burn for much longer |
|
|
Why are electrical burns so dangerous? |
Most of the destruction from electrical burns is internal because the route of least electrical resistance follows nerves, blood vessels, and fascia; injury is usually worse than external burns at entrance and exit sites would indicate; cardiac dysrhythmias, myoglobinuria, acidosis, and renal failure and common |
|
|
How is myoglobinuria treated? |
To avoid renal injury, think "HAM": - Hydration with IV fluids - Alkalization of urine with IV bicarb - Mannitol diuresis |
|
|
Define "first-degree" burn? |
Epidermis only |
|
|
Define "second-degree" burn? |
Epidermis and varying levels of dermis |
|
|
Define "third-degree" burn? |
Full-thickness; all layers of the skin including the entire dermis |
|
|
Define "fourth-degree" burn? |
Burn injury into bone or muscle |
|
|
How do first-degree burns present? |
Painful, dry, red areas that do not form blisters (think of a sunburn) |
|
|
How do second-degree burns present? |
Painful, hypersensitive, swollen, mottled areas with blisters and open weeping surfaces |
|
|
How do third-degree burns present? |
Painless, insensate, swollen, dry, mottled white, and charred areas; often described as dried leather |
|
|
What is the major clinical difference between second and third-dgree burns? |
Third-degree burns are painless, whereas second-degree burns are painful |
|
|
By which measure is burn severity determined |
- Depth of burn and TBSA affected by second- and third-degree burns - TBSA is calculated by the "rule of nines" in adults and by a modified rule in children to account for the disproportionate size of the head and trunk |
|
|
What is the rule of nines? |
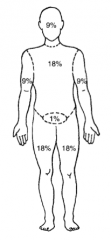
In an adult, the total body surface area that is burned can be estimated by the following: - Each upper limb = 9% - Each lower limb = 18% - Anterior and posterior trunk = 18% - Head and neck = 9% - Perineum and genitalia = 1% |
|
|
What is the "rule of the palm"? |
Surface area of the patient's palm is ~1% of the TBSA used for estimating size of small burns |
|
|
What is the burn center referral criteria for second-dgree burns? |
>20% total body surface area
Or >10% TBSA in children or elderly
- Any burns involving the face, hands, feet, or perineum - Any burns with inhalation injury - Any burns with associated trauma - Any electrical burns |
|
|
What is the burn center referral criteria for third-degree burns? |
>5% total body surface area
- Any burns involving the face, hands, feet, or perineum - Any burns with inhalation injury - Any burns with associated trauma - Any electrical burns |
|
|
What is the treatment of first-degree burns? |
- Keep clean - ± Neosporin - Pain meds |
|
|
What is the treatment of second-degree burns? |
- Remove blisters - Apply antibiotic ointment (usually Silvadene) and dressing - Pain meds - Most second-degree burns do not require skin-grafting (epidermis grows from hair follicles and from margins) |
|
|
What are some newer options for treating a second-degree burn? |
1. Biobrane (silicone artificial epidermis - temporary) 2. Silverlon (silver ion dressing) |
|
|
What is the treatment of third-degree burns? |
Early excision of eschar (within first week post-burn) and split thickness skin graft (STSG) |
|
|
How can you decrease bleeding during excision? |
Tourniquets as possible, topical epinephrine, topical thrombin |
|
|
What is an autograft STSG? |
Split Thickness Skin Graft from the patient's own skin |
|
|
What is an allograft STSG? |
Split Thickness Skin Graft from a cadaver (temporary coverage) |
|
|
What thickness is the STSG? |
10/1000 to 15/1000 of an inch (down to the dermal layer) |
|
|
What prophylaxis should the burn patient get in the ER? |
Tetanus |
|
|
What is used to evaluate the eyes after a third-degree burn? |
Fluorescein |
|
|
What principles guide the initial assessment and resuscitation of the burn patient? |
ABCDEs, then urine output; check for eschar and compartment syndromes |
|
|
What are the signs of smoke inhalation? |
- Smoke and soot in sputum / mouth / nose - Nasal / facial hair burns - Carboxyhemoglobin - Throat / mouth erythema - History of loss of consciousness / explosion / fire in small enclosed area - Dyspnea - Low O2 saturation - Confusion - Headache - Coma |
|
|
What diagnostic imaging is used for smoke inhalation? |
Bronchoscopy |
|
|
What lab value assesses smoke inhalation? |
Carboxyhemoglobin level (a level >60% is associated with 50% mortality)
Treat with 100% O2 and time |
|
|
How should the airway be managed in the burn patient with an inhalational injury? |
With a low threshold for intubation; oropharyngeal swelling may occlude the airway so that intubation is impossible; 100% oxygen should be administered immediately and continued until significant carboxyhemoglobin is ruled out |
|
|
What is "burn shock"? |
Burn shock describes the loss of fluid from the intravascular space as a result of burn injury, which causes "leaking capillaries" that require crystalloid infusion |
|
|
What is the "Parkland Formula"? |
V = TBSA Burn (%) * Weight (kg) * 4
Formula widely used to estimate the volume (V) of crystalloid necessary for the initial resuscitation of the burn patient
Half of the calculated volume is given in the first 8 hours, the rest in the next 16 hours |
|
|
What burns qualify for the Parkland formula? |
≥ 20% TBSA second- and third-degree burns only |
|
|
What is the Brooke formula for burn resuscitation? |
Replace 2 cc for the 4 cc in the Parkland formula |
|
|
How is crystalloid given to burn patients? |
Through two large-bore peripheral venous catheters |
|
|
Can you place an IV or central line through burned skin? |
YES |
|
|
What is the adult urine output goal? |
30-50 cc (titrate IVF) |
|
|
Why is glucose-containing IVF contraindicated in burn patients in the first 24 hours post-burn? |
Patient's serum glucose will be elevated on its own because of the stress response |
|
|
What fluid is used after the first 24 hours post-burn? |
Colloid; use D5W and 5% albumin at 0.5 cc / kg / % burn surface area |
|
|
Why should D5W IV be administered after 24 hours post-burn? |
Because of the massive sodium load in the first 24 hours of LR infusion and because of the massive evaporation of H2O from the burn injury, the patient will need free water
After 24 hours, the capillaries begin to work and then the patient can usually benefit from albumin and D5W |
|
|
What is the minimal urine output for burn patients? |
Adults 30 cc; children 1-2 cc/kg/hr |
|
|
How is volume status monitored in the burn patient? |
- Urine output - BP and HR - Peripheral perfusion - Mental status - Foley catheter is mandatory and may be supplemental by central venous pressure and pulmonary capillary wedge pressure monitoring |
|
|
Why do most severely burned patients require nasogastric decompression? |
Pts with greater than 20% TBSA burns usually develop a paralytic ileus --> vomiting --> aspiration risk --> pneumonia |
|
|
What stress prophylaxis must be given to the burn patient? |
H2 blocker to prevent burn stress ulcer (Curling's ulcer) |
|
|
What are the signs of burn wound infection? |
- Increased WBC with left shift - Discoloration of burn eschar (most common sign) - Green pigment - Necrotic skin lesion in unburned skin - Edema - Ecchmyosis tissue below eschar - Second degree burns that turn into third-egree burns - Hypotension |
|
|
Is fever a good sign of infection in burn patients? |
No |
|
|
What are the common organisms found in burn wound infections? |
- S. aureus - Pseudomonas - Stretococcus - Candida albicans |
|
|
How is a burn wound infection diagnosed? |
Send burned tissue in question to the laboratory for quantitative burn wound bacterial count; if the count is >10^5/gram, infection is present and IV antibiotics should be administered |
|
|
How are minor burns dressed? |
Gentle cleaning with non-ionic detergent and débridement of loose skin and broken blisters
The burn is dressed with a topical antibacterial (eg, neomycin) and covered with a sterile dressing |
|
|
How are major burns dressed? |
Cleansing and application of topical antibacterial agent |
|
|
Why are systemic IV antibiotics contraindicated in fresh burns? |
Bacteria live in eschar, which is avascular (the systemic antibiotic will not be delivered to the eschar); thus apply topical antimicrobial agents |
|
|
What are the advantages / disadvantages of Silver Sulfadiazine (Silvadene)? |
- Painless, but little eschar penetration - Misses pseudomonas - Idiosyncratic neutropenia - Sulfa allergy is contraindication |
|
|
What are the advantages / disadvantages of Mafenide Acetate (Sulfamylon)? |
- Penetrates eschars - Broad spectrum (but misses Staphylococcus) - Causes pain on application - Triggers allergic reaction in 7% of patients - May cause acid-base imbalances (think: Mafenide ACetate = Metabolic ACidosis
** Agent of choice in already-contaminated burn wounds |
|
|
What are the advantages / disadvantages of Polysporin? |
- Polymyxin B sulfate - Painless, clear, used for facial burns - Does not have a wide antimicrobial spectrum |
|
|
Are prophylactic systemic antibiotics administered to burn patients? |
No - prophylactic antibiotics have not been shown to reduce the incidence of sepsis, but rather have been shown to select for resistant organisms
IV antibiotics are reserved for established wound infections, pneumonia, urinary tract infections, etc |
|
|
Are prophylactic antibiotics administered for inhalational injury? |
No |
|
|
Circumferential, full-thickness burns to the extremities are at risk for what complication? |
Distal neurovascular impairment |
|
|
How is distal neurovascular impairment treated? |
Escharotomy: full-thickness longitudinal incision through the eschar with scalpel or electrocautery |
|
|
What is the major infection complication (other than wound infection) in burn patients? |
- Pneumonia - Central line infection (change central lines prophylactically every 3-4 days) |
|
|
Is tetanus prophylaxis required in the burn patient? |
Yes, it is mandatory in all patients except those actively immunized within the past 12 months (with incomplete immunization: toxoid x3) |
|
|
From which burn wound is water evaporation the highest? |
Third degree |
|
|
Can infection convert a partial-thickness injury into a full-thickness injury? |
Yes! |
|
|
How is carbon monoxide inhalation overdose treated? |
100% O2 (+/- hyperbaric O2) |
|
|
Which electrolyte must be closely followed acutely after a burn? |
Na+ (sodium) |
|
|
When should central lines be changed in the burn patient? |
Most burn centers change them every 3-4 days |
|
|
What is the name of the gastric / duodenal ulcer associated with burn injury? |
Curling's ulcer |
|
|
How are STSGs nourished in the first 24 hours? |
IMBIBITION (fed from wound bed exudate) |

