![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
14 Cards in this Set
- Front
- Back
|
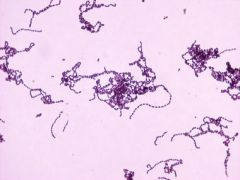
Streptococcus species (gram positive cocci arranged in chains) |
Gram positive cocci, oval or round usually in chains Normal flora of oral cavity, nasopharynx and intestinal tract Facultative anaerobe Catalase negative Nonmotile Non-sporeforming |
|

Hemolysis |
Streptococcus and Enterococcus grouped by the appearance of colonies and hemolytic reaction on sheep blood agar (way they harm red blood cells) |
|
|
Alpha streptococci |
alpha hemolysis
Partial destruction (bruising) of RBC around colony, give green or brown discoloration of medium Streptococcus pneumoniae (primary pathogen) Enterococcus (Lancefield group D) Streptococcus bovis group (Lancefield group D) - members include S. gallolyticus and S. infantarius Viridans Streptococcus group |
|
|
Beta streptococci |
beta hemolysis - clear colorless zone Two common toxins produce beta hemolysis: streptolysin O - oxygen labile (causes subsurface hemolysis if the plate has been stabbed) streptolysin S - oxygen stable (causes surface hemolysis) Streptococcus pyogenes (group A) Streptococcus agalactiae (group B) Enterococcus (group D) very rarely beta-hemolytic S. bovis group (group D) very rarely beta-hemolytic - members include S. gallolyticus and S. infantarius |
|
|
Gamma streptococci |
no hemolysis
Ignores RBC (note: after two days, bacteria being gamma hemolysis can start to look like alpha (yellow) but still categorized as gamma) Non-hemolytic Streptococcus species Enterococcus Streptococcus bovis group (group D) - members include S. gallolyticus and S. infantarius |
|
Streptococcus pyogenes (Group A) |
Infections: Pharyngitis, Tonsillitis, swollen lymph nodes (Strep throat, most common) Otitis Media (middle ear infection) Scarlet Fever (strep throat with a rash, toxin that causes skin rash) Impetigo (also caused by staphylococcus, can have both present) Cellulitis (flesh eating bacteria, bacteria acquire enzyme to degrade tissue) |
|
|
S. pyogenes |
Post-streptococcal sequelae:(a condition that is the consequence of a previous disease or injury) Rheumatic fever (auto-immune reaction and damage to heart muscle following pharyngitis with s. pyogenes, heart muscle damage) Acute glomerulonephritis (auto-immune reaction and damage to renal glomeruli following skin infection or pharyngitis with s. pyogenes) Own antibody overreacting after the organism is gone. Auto antibody destruction of tissue. |
|

Steptococcus agalactiae Group B |
Produce polysaccharide capsules Colonizers of female genital tract (10-30%) Diseases: Neonatal infections - leading cause of Meningitis, Septicemia, Pneumonia in neonates - Mortality rate 10-15% - Recommended to screen all women for group B during 3rd trimester of pregnancy and child birth Urinary Tract Infections and Bacteremia (bacteria in the blood) affects elderly and immunocompromised Post-surgical gynecologic infection |
|
|
Strepococcus pneumoniae (alpha) |
Polysaccharide capsule (invisibility cloak for phagocytosis) Pneumolysin (toxin that is toxic to pulmonary endothelial cells and may allow spread to bloodstream) Diseases: Otitis Media (middle ear infection in children) Bacterial Pneumonia (community acquired) Meningitis (often secondary to pneumonia) Sinusitis Vaccinations: Pneumococcal Conjugate Vaccine - usually given to infants and children (less than 2) in four doses - Kids 24 mo. to 4 years who are unvaccinated or didn't finish doses - Single dose to 6-18 yr children with certain medical conditions 23-valent Polysaccharide Vaccine - Adults 65 yrs or older - Anyone 2 - 64 yrs who is immunocompromised |
|
|
Viridans Streptococcus "means green" |
α-hemolytic (producing a green coloration on blood agar plates)
Normal Flora of Upper Respiratory Tract Subacute bacterial endocarditis - most common cause (infection of heart inner lining, can cause damage) |
|
|
Enterococcus (lancefield group D) |
Over 30 species Two responsible for most human infections - E. faecalis - E. faecium Normal Flora of Intestinal Tract Low virulence (problem only when produces antibiotic resistance) Diseases: Urinary Tract Infections Endocarditis (rarely) Wound Infections |
|
|
Group D Stretpococcus |
interpreted as possible S. bovis group, but subject to clinical interpretation before further identification is deemed necessary GI diseases (S. bovis group has strong association with) GI carcinomas |
|
|
Antibiotic Treatment - Streptococcus |
Penicillin is drug of choice S. pneumoniae - penicillin resistant, treated with vacomycin or 3rd generation cephalosporin S. pyogenes - not reported as penicillin resistant but penicillin treatment of pharyngitis may fail due to diffusible beta-lactamases produced in normal throat flora |
|
|
Antibiotic Treatment - Enterococcus |
Resistant to penicillins or cephalosporins (beta-lactams) when given alone Combination of penicillin and aminoglyside overcomes intrinsic resistance via drug synergism (one drug to work on wall and other to work on the inside) Uncomplicated drugs can usually be treated with beta-lactams If resistant to combined drugs, serious infections can be treated with vancomycin If vancomycin resistant, Synercid or Linezolid may be used VRE - vancomycin-resistant enterococcus |

