![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
|
Medical tx of choice for acromegaly |
1. Octreotide (TOC) 2. Dopamine agonist (can be used for both prolactinoma and acromegaly)
3. Surgery is the last resort. However, common because if the tumor is a macroadenoma (>1cm)
|
|
|
How do you diagnose acromegaly |
1. IGF/Somatomedins 2. Glucose load - pts with acromegaly fail to suppress GH in response to oral glucose load 3. MRI |
|
|
MCC of hypopituitarism in children |
Craniopharyngiomas |
|
|
In hypopituitarism, which hormones are usually lost first
Which hormone is lost last |
1. GH and Gonadotropins(FSH, LH) These are also the hormones we need the least.
2. ACTH (the most important hormone) |
|
|
How do we diagnose hypopituitarism? |
Check for hormones that are lost early.
measure GH after inducing hypoglycemia (with insulin ~ 5U of insulin) Normal person has increased GH after induced hypoglycemia. |
|
|
What are the two conditions associated with hypopituitarism: |
1. Pituitary apoplexy - Acute onset. - Hx of pituitary adenoma in past - Pt presents with: headache, Altered mental status,, nucchal rigidity, vomitting (meningeal signs) - Sudden bleeding in the center of the pituitary - Endocrine emergency
2. Sheehan syndrome - weeks to months, sometimes even years after pregnancy - inability to lactate |
|
|
T or F: Empty Sella Syndrome causes hypopituitarism |
False. It causes no hormonal issues. Usually an incidental finding.
Pituitary is just pushed to the sides. |
|
|
1. Which class of drugs may cause hyperprolactinemia?
2. Which hypothalamic hormone can cause hyperprolactinemia?
3. What tests should be carried out to rule out non-primary causes of hyperprolactinemia (3)? |
1. Haloperidol, H-2 blockers (Have anti-dopamine effect)
2. TRH at very high levels enhances prolactin
3. a) TSH to rule out hypothyroidism b) Pregnancy c) Drug history to check for anti-dopamine rx d) Check for high prolactin after verifying a-c e) MRI only after a-d |
|
|
Tx of choice for hyperprolactinemia? |
1. Dopamine agonist: Bromocriptine, cabergoline
Start off with both of these drugs. Bromocriptine may cause n/v cabergoline: not enough data for pregnancy
Both of these reverse effects of prolactin and ALSO reduce the size of the prolactinoma. |
|
|
1. Test of choice to dx Diabetes insipidus? |
1. Water depravation test: a) Normal Subject: Plasma osmolarity increases --> ADH increases --> Urine osmolarity increases (water is being retained) and plasma osm. stabilizes,
b) Pt with diabetes insipidus: Plasma osm increase --> ADH not release or no response to ADH --> Urine osm remains low and serum osm. continues to increase |
|
|
1. How to distinguish central from nephrogenic DI? |
1. Give ADH at the end of water deprivation test once its determined that the patient has DI a) Central - Urine osm. increase in response to ADH and serum osm decreases
b) Nephrogenic - No change in Urine osm. ADH levels are usually elevated |
|
|
1. What causes central DI
2. What causes nephrogenic DI |
1. Any space occupying lesion in the brain.
2.a) Lithium - MCC b) democlocycline - MCC after Li c) Extreme hypercalcemia d) Some pts with sickle cell ds. |
|
|
1. What is the tx of choice for Central DI? |
1. Desmopressin - intranasally Note: ADH is not given as tx because it has both anti-diuretic and vasopressor effect (htn). ADH is only used for water deprivation test.
2. Mild diuretic (HCTZ, Chlorthalidone, Amiloride) - quite a paradox!!! NSAIDs, stop the med causing the Nephrogenic DI |
|
|
1. T or F: SIADH presents with clinical edema 2. SIADH presents with ______ hyponatremia 3. What hormones should be checked before making the dx of SIADH? |
1. F 2. Euvolemic hyponatremia Clinical pearl: Consider SIADH in all cases of euvolemic hyponatremia 3. Check TSH and cortisol levels |
|
|
What conditions can cause SIADH? |
1. Any chronic lung condition. Ideal scenario is of Small cell carcinoma of the lung. 2. Any CNS disorder: esp. any space occupying lesion 3. Drugs: - Chlorpropamide - Vincristine, vinblastine, cyclophosphamide - SSRI (esp. sertraline) ! |
|
|
Tx of SIADH? |
1. Fluid restriction (800-1000 ml/day)
2. Meds: If fluid restriction does not work, basically give the same drugs that cause DI: a) Demeclocycline - Tx of choice b/c benign b) Lithium - if severe confusion/convulsions/sz: - Hypertonic saline (5%) 200-300 ml IV in 3-4 hrs |
|
|
1. Increased TBG levels are seen in (2):? 2. Decreased TBG levels are seen in (2):? |
1. Pregnancy and Oral contraceptives 2. Nephrotic syndrome and liver disease |
|
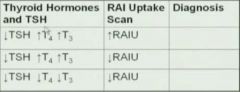
Dx=? 1. 2. 3.
Note: T3 and T4 are free |
1. Primary hyperthyroidism -Graves's if diffuse RAIU uptake-MCC. Proptosis is only seen in graves - Toxic nodular goiter if not diffuse uptake - 2nd MCC 2. Subacute thyroiditis or DeQuervains: Tender, over a few weeks becomes euthyroid. Due to vital infection --> breakdown of thyroid and spilling of thyroid hormones Also, Exogenous thyroid use. 3. Secondary hypothyroidism - sheehan's or pituitary apoplexy |
|
|
What is the tx of Graves ds? |
1. Treatment involves - Propranalol - to tx the adrenergic sx - PTU or Methimazole - agranulocytosis is a side reaction, if SE then stop the med. Methimazole also stops peripheral conversion of T4 to T3. Long term: - RAI ablation - definitive tx in the U.S. Only done once euthyroid - Thyroidectomy - rarely done. Reserved only for the pregnant patient. |
|
|
Tx of Graves in pregnant pt? |
1. Cannot use methimazole 2. Can only use to propranolol or PTU used in small doses only. (both cross the placenta) 3. Thyroidectomy - if uncontrolled Graves during 2nd trimester. |
|
|
1. How do patients with Toxic Multinodular Goiter present:?
2. What is the tx? |
1. Toxic multinodular goiter - pts are elderly with cardiac manifestations - Arrythmia - esp. a-fib - CHF - high output HF - nodular goiter on exam - NO ophthalmopathy
2. Radioactive iodine (just like Graves) |
|
|
What is the treatment of thyroid strom? |
1. Tx - Antithyroid agents esp. methimazole - Iodine - BB - Dexamethasone - given in all severe forms of thyroid ds. - IVF and cooling blankets |
|
|
1. Which drugs may cause hypothyroidism (2) ? 2. After starting a pt on levothyroxine, how long does it take for the TSH levels to equilibrate? 3. For secondary hypothyroidism, what treatment modification is made? |
1. Lithium and Amiodorone 2. 6 weeks 3. Give hydrocortisone before giving levothyroxine because if the pt has cortisol insufficiency and by giving synthroid you are revving up their metabolism, you can give them adrenal crisis
|
|
|
What is the extreme form of hypothyroidism? |
1. Myxedema Coma - Untreated long standing disease - Stupor - hypothermia Precipitated by: infection, cold exposure
2. Very high doses of T4 and the only instance when T3 is given - Corticosteroids - warming blankets, IVF |
|
|
1. What is the treatment of subacute thyroiditis?
2. For every 1 mg/dl drop in albumin below 4 mg/dL, the amount of calcium drops by ______ |
1. If symptomatic: ASA/NSAIDs, (maybe) prednisone
2. 0.8 |
|
|
1. MCC of severe hypercalcemia is: ____ 2. MCC of hypercalcemia is ____ 3. PTH-like peptide are secreted by _____
4. Other causes of hypercalcemia (5) ?
|
1. malignancy 2. hyperparathyroidism 3. Squamous cell carcinomas 4. Sarcoidosis - tx with prednisone Prolonged immobilization - just watch the hypercalcemia Hyperthyroidism - esp. Graves Familial hypocalciuric hypercalcemia - only cause of low urine calcium Drugs: HCTZ
|
|
|
What are the clinical scenarios of hypercalcemia?
a) Neurological? b) GI? c) Renal ? d) Cardiovascular |
a) Neuro - Lethargy, confusion b) GI - constipation, abdominal pain c) Renal - Polyuria, polydipsia (b/c a form of nephrogenic DI) Stones d) Cardiovascular - short QT interval |
|
|
What is the management of significant hypercalcemia (4)? |
1. IVF - normal saline - cornerstone of tx because they are mostly suffering from nephrogenic DI. Furosemide - Also helps prevent fluid overload from the IVF. Only given after the patient is hydrated and pt shows sx of fluid overload Bisphosphonates - Pamidronate (long acting bisphosphonate) - given to pt if they have malignancy esp. multiple myeloma. Takes 2 days to work. Calcitonin - lowers Ca within a few hours. Used if Ca is not getting lowered. Given in conjunction with bisphosphonates. Calcitonin stop working after two days
|
|
|
1. Hypercalcemia and elevated PTH. Dx?
2. What are the causes of hypocalcemia |
1. Primary hyperparathyroidism 2. Acquired hypoparathyroidism (due to surgery) Hypomagnesemia - Mg is required for normal secretion of PTH. - Mg is also required for activation of osteoclasts Vitamin D deficiency - Renal failure - Intestinal malabsorption - |
|
|
What are the indications for surgery for tx of primary hyperthyroidism (2)? |
1. Indications: Symptomatic pt and young pts. |
|
|
What are the signs of hypocalcemia? |
1. Neuromuscular irritability: tetany, laryngospasm, Cramping, sz 2. Chvostek's sign: tetany on facial nerve 3. Trousseau's sign: inflate BP cuff for 1 min -> tetany 4. Cardiovascular : QT prolongation |
|
|
1. Low PTH, Low Ca, high PO4: ? 2. high PTH, Low Ca, Low PO4? |
1. hypoparathyroidism 2. Vit D Deficiency
First look at calcium and then the PO4, if PTH is not given. |
|
|
1. What is the tx of Hypocalcemia: a) Acute b) Maintenance
2. What treatment modification is made for patients with end stage renal disease |
1. a) IV Calcium gluconate b) Oral calcium 2-4 g/day, Vit D
2. Pts with end stage renal disease: |
|
|
1. All Sulfonylureas are metabolized by the _____ except _________ which is metabolized by the ___.
2. The main mech of action of metformin is:
3. The main SE of metformin is: |
1. All Sulfonylureas are metabolized by the kidneys except tolbutamide which is metabolized by the liver. Requires 2-3 doses/day. Other sulfonylureas require 1-2/ daily.
2. Prevents gluconeogenesis in the liver. Has no no effect on beta cells. Therefore, no wt gain and no hypoglycemia.
3. GI side effects (most common), lactic acidosis (rare but high morbidity and mortality). Most of lactic acidosis patients were ones with renal insufficiency. MUST NOT BE GIVEN TO PTS WITH RENAL DS. |
|
|
What are the 1st line agents for DM Type II? |
1. Metformin, Sulfonylureas, Glitazones(some consider it as 1st line as well) |
|
|
DIABETIC KETOACIDOSIS 1. What is a normal anion gap 2. What is the cause of high BUN: Cr ratio in DKA 3. What is the cause of hyperkalemia in DKA (2)? 4. Pt has normal K+ with DKA 5. When do you stop IV insulin in pts with DKA 6. What do you do if glucose gets low while being treated for DKA |
1. 12 2. Prerenal azotemia - tx with fluids 3. Lack of insulin, acidemia. Tx by just tx the DKA 4. Have to supplement the K+ in the fluids while giving IVF. Give KCl 5. Pt is out DKA = anion gap has normalized and HCO3 is back to normal 6. Keep giving insulin. But also give D5 |
|
|
1.Most common cause of blindness in the U.S? Tx? 2. What is Somogyi phenomenon 3. Dawn effect. 4. How do you distinguish between Dawn and Somogyi |
1. Diabetic retinopathy - proliferative retinopathy. Tx = photocoagulation. 2. Somogyi: Morning hyperglycemia due to too much insulin at night. 3. Dawn: Morning hyperglycemia due to insulin being given too little and too early 4. Tx: Check out the glucose levels at 3AM. |
|
|
1. What is the most definitive test to dx Cushing syndrome? 2. Which disease can be suppressed by high dose overnight dexamethasone suppression test? 3. Which cause of cushing syndrome cause hyperpigmentation? |
1. 24 hour free urine cortisol - if normal, no cushings. If elevated - Cushing syndrome.
2. Pituitary adenoma 3. Lung cancer |
|
|
1. What is the main cause of secondary hyperaldosteronism? 2. (T or F) Pts with primary aldosteronism have pedal edema? |
1. Intravascular volume depletion. 2. Pedal edema only may exist with secondary hyperaldosteronism. |
|
|
1a) MCC of Congenital Adrenal Hyperplasia?
1 b) How does it present in males and females How is it dx? How is it tx? |
21-hydroxylase deficiency - 95% of cases Female: ambiguous genitalia Males: normal, hypotension later
Dx: Elevated progestrone Tx: Hydrocortisone + Fludrocortisone given simaltaneously |
|
|
1. MCC of Primary adrenal insufficiency =? 2. What are the sx of primary adrenal insufficiency?
3. What are the lab findings of adrenal insufficiency? 4. How is adrenal insufficiency dx? |
1. Autoimmune 2. Sx = Hypotension, hyperpigmentation(only in primary) 3. Hyperkalemia Hypoglycemia Eosinophilia - 25-30% of cases. Don't know why. 4. ACTH stimulation test. Will diagnose both primary and secondary (chronic only) adrenal insuff. 5. Tx= Hydrocortisone +/- Fludrocortisone (if mineral corticoid effected) |
|
|
1. Pt with HTN develops orthostatic hypotension? Dx? 2. Best test to dx this condition:? 3. Tx=? 4. What is the triad of clinical findings for pheochromocytoma? |
1. Pheochromocytoma 2. Urine free catecholamines. Once dx then localize with MRI 3. alpha blockade (w/ phentalamine or phenoxybenzamine) then surgery. Also, fluids since most of these pts are volume depleted. 4. Episodic headaches, palpitations, diaphoresis |
|
|
1. MCC of hypogonadism? b) male pts are at an increased risk for which kind cancer? c) What are the lab findings (2)? d) How do you treat it? |
1. Klinefelter syndrome 47XXY (80% of cases). Primary hypogonadism b. Breast cancer c) Elevated FSH and LH d) Tx = testosterone |
|
|
1. MCC of secondary hypogonadism? 2. What is the main cause of this disease? 3. What is the unusual clinical finding for these patients? |
1. Kallmann syndrome. X-linked single gene defect. 2. Due to low GnRH --> low FSH, LH 3. Anosmia (permanent) |
|
|
1. Pts with DM Type I should always be screened for ? 2. How is it diagnosed ? |
1. Celiac ds.--> prevalence btw 3-6%. Other risk factors for celiac ds are Down syndrome, chronic lymphocytic (Hashimoto) thyroiditis, selective IgA deficiency 2. Serum tissue transglutaminase IgA (TTG) antibody. Anyone who has a positive TTG antibody test needs to be confirmed with a biopsy |
|
|
1. Diarrhea, facial flushing, bronchospasms 2. Hypercalcemia, hyperphosphotemia, high PTH 3, Urine osmolality < 200mOsm/Kg and specific gravity < 1.005 g/ml.
4. Hyponatremia, hyperkalemia, hyperchloremic acidosis. Likely diagnosis? |
1. Carcinoid syndrome 2. Pseudohypoparathyroidism - due to end organ resistance to PTH --> lack of response by kidneys and bones to PTH 3. DI 4. Adrenal insufficiency |
|
|
Diagnosis: 1. Glucose intolerance (DM), Wt loss, necrolytic migratory erythema, anemia, diarrhea, thromboembolism 2. _______ cause multiple gastic ulcers 3. ____ is characterized by excessive watery diarrhea (>3 L/D), hypokalemia, achlorhydia |
1. Glucagonoma. Typically in older pts. 2. Gastrinoma - a/w MEN I 3. VIPoma |
|
|
1. Pt with thyroid nodule and low TSH, whats the next step in management? 2. Hypothyroidism, unconsciousness, edema and skin changes. |
1. Radioiodine scan 2. Myxedema coma |
|
|
1. ACTH (cosyntropin) stimulation causes increase in serum cortisol to >= ___ ug/dL after 30 or 60 mins.
2. Low free T4 --> __?__ TRH --> __?___ dopamine-----> ___?___ prolactin |
1. 18 2. Low free T4 --> increases TRH --> inhibits dopamine -----> increases prolactin |
|
|
1. Management of subsequent pregnancy in a female who has already given birth to a child with 21-hydroxylase deficiency |
1. Administration of dexamethasone no later than 6 weeks of gestation. Dex crosses placenta and suppresses fetal adrenal steroid secretion and prevents masculinization. Thus preventing ambiguous genitalia in females. |
|
|
1. For pts with high Alk Phos, _____ lab should be taken to determine the source of Alk Phos
2. Tx of choice for cardiac patients with amiodorone induced hypothyroidism is ____ |
1. GGT or 5'nucleotidase - if high then Alk Phos is from the liver otherwise bone
2. Supplementation with levothyroxine
|
|
|
Bones, stones, groans, and psychiatric overtones. Dx=? |
Primary hyperparathyroidism
- can also cause pancreatitis, because of hypercalcemia - Have PUD, because excess Ca stimulates Gastrin --> acid production - Depression and other psych problems
|
|
|
MCC of Primary hyperparathyroidism (2) |
1. Parathyroid adenoma 2. Parathyroid hyperplasia |
|
|
Tissue nonresponsiveness to PTH. Short 4th and 5th digit. Elevated PTH. Dx?
Tx? |
1. Pseudohypoparathyroidism
2. Ca and Vit D supplementation |
|
|
1. Drugs that block DA synthesis ---> __________. 2. Name the drugs |
1. Hyperprolactinemia
2. Phenothiazines Risperidone Haloperidol Methyldopa Verapamil |
|
|
High dose dexamethasone suppression test will not suppress ACTH levels due ______
Whats the dx if High dose Dex suppresses ACTH? |
1. Adrenal tumor (low ACTH level) Non-Adrenal ACTH secreting tumor (High ACTH)
2. Pituitary adenoma |
|
|
When do you test for High Dose Dex suppresion test? |
1. No change in cortisol following morning after low dose dex supression test
2. 24 hr free urinary cortisol is High (Cushing Syndrome)
|
|
|
What Endocrine are involved with MEN I |
3P's -Pituitary -Parathyroid -Pancreas
Features: hypercalcemia, hyperparathyroidism, possible ZES, various pituitary disorders
|
|
|
What endocrines are involved with MEN II |
2 P's - Parathyroid - Pheochromocytoma (Adrenals) - Medullary carcinoma of the thyroid
Features: increased calcitonin, hypercalcemia, hyperparathyroidism, increased urine catecholamines |
|
|
What endocrines are involved with MEN III (IIb) |
1 P: - Pheochromocytoma (adrenals) - Medullary carcinoma of the thyroid - Mucosal Neuroma
Features: increased calcitonin, hypercalcemia, hyperparathyroidism, Marfanoid body habitus |
|
|
Indications for Surgical Parathyroidectomy |
1. If symptomatic |

