![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
537 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is the typical complaint of a pt with retinal detachment? |
Sudden painless onset of flashing lights
Floaters “shade comes down” over the vision of one eye |
|
|
|
What is the treatment for benign paroxysmal positional vertigo (BPPV)?
|
Epley maneuver (reposition otolith) |
|
|
|
What is Todd’s paralysis?
|
Post-ictal hemiparesis lasting 15-24hrs
|
|
|
|
List examples of SSRIs
|
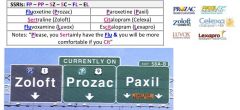
Fluoxetine (Prozac)
Sertraline (Zoloft) Paroxetine (Paxil) Fluvoxamine (Luvox, Lescol) Citalopram (Celexa) Escitalopram (Lexapro) |
|
|
|
List examples of Tricyclic Antidepressants (TCAs)
|

Imipramine (Tofranil)
Amitriptyline (Elavil) Desipramine (Norpramin) Nortriptyline (Aventyl) Clomipramine (Anafranil) Doxepin (Silenor, Sinequan) |
|
|
|
List examples of MAOIs
|
Phenelzine (Nardil)
Tranylcypromine (Parnate) Selegiline (Eldepryl, Emsam, Zelapar) |
|
|
|
List example of NDRI
|

Buproprion (wellbutrin)
|
|
|
|
List examples of SNRI
|

Venlafaxine (Effexor, Pristiq)
Duloxetine (Cymbalta) Milnacipran (Savella) Nefazodone (Serzone) |
|
|
|
list examples of tetracyclic antidepressants
|
Mirtazapine (Remeron)
Trazodone (Desyrel, Oleptro |
|
|
|
What drugs, when combined with SSRIs are known for causing Serotonin syndrome?
|
SSRIs, SNRIs, MAOIs
LSD, St. John’s wort, Levodopa, Meperidine, Lithium Amphetamines, cocaine, ectasy |
|
|
|
What is the most common cause of sensorineural hearing loss? What is the most common cause of conductive hearing loss?
|
Sensorineural → presbycusis
Conductive → otosclerosis |
|
|
|
What is the most common complication of recurrent otitis media?
|
hearing loss
|
|
|
|
An elderly pt presents to the ED with a HA & dilated right pupil. During the history, she reports that she fell at home 5 days ago. What is the most likely diagnosis?
|
R-sided subdural hematoma
|
|
|
|
What medications other than stimulants are used in the treatment of ADHD?
|
TCAs, Bupropion, α-2 agonists (clonidine)
|
|
|
|
What medications are used in the treatment of Tourette’s syndrome?
|
Fluphenazine (Permitil, Prolixin)
Pimozide (Orap) Tetrabenazine (Xenazine) |
|
|
|
What are the most worrisome side effects of the ADHD drug atomoxetine?
|
↑ suicidal ideation
liver injury |
|
|
|
What is the definitive tx for an epidural or subdural hematoma?
|
Evacuation of the hematoma with a burr hole
|
|
|
|
What serum lab abnormalities might you see in a pt with bacterial meningitis? (SU pg 169)
|
↑ WBC ct, left shift or bandemia, leucopenia, hypOnatremia
|
|
|
|
A pt comes to the clinic with the c/o hearing loss and vertigo. On exam of the tympanic membrane you note a grayish-white “pearly” lesion involving the TM. What is the dx?
|
cholesteatoma
|
|
|
|
What anti-islet antibodies can be seen in pts with Type 1 DM?
|
Anti-insulin (IAA)
Anti-islet cell cytoplasm (ICA) Anti-glutamic acid decarboxylase (GAD) Anti-tyrosine phosphatase (IA-2) |
|
|
|
How do you distinguish the somogyi effect from the Dawn phenomenon?
|
Somogyi: at 2-3 am, will have low blood glucose
Tx: ↓ evening insulin Dawn: at 2-3 am will have high blood glucose Tx: ↑ evening insulin |
|
|
|
A concerned mother brings her 6yo son to see you. He c/o nausea and has been vomiting. The mother says that she thinks he caught a stomach bug. What might the child have instead?
|
Diabetic ketoacidosis (DKA)
|
|
|
|
What must be kept in mind for a type I diabetic pt that plans to begin a strenuous exercise program?
|
↑ exercise causes muscle to uptake more glucose
pt is at risk of hypoglycemia |
|
|
|
Whch type of insulin is used in continuous infusion insulin pumps & in treatment of DKA?
|
Regular or fast acting insulin
|
|
|
|
Describe the basic mechanism behind the Somogyi effect
|
Evening insulin dose is too high, blood sugar bottoms out an hour or two past midnight
Stress hormones are released in response to the very low blood sugar → morning glucose is elevated Somogyi: at 2-3 am, will have low blood glucose Tx: ↓ evening insulin Dawn: at 2-3 am will have high blood glucose Tx: ↑ evening insulin |
|
|
|
Describe the mechanism behind the Dawn phenomenon
|
Very elevated morning blood sugar, evening insulin dose is too low
Blood sugar is inadequately treated so it continues to ↑ throughout the night Somogyi: at 2-3 am, will have low blood glucose Tx: ↓ evening insulin Dawn: at 2-3 am will have high blood glucose Tx: ↑ evening insulin |
|
|
|
How can you differentiate between the Somogyi effect & Dawn phenomenon?
|
Check blood sugar in middle of night (2-4am)
|
|
|
|
What Diabetic drug:
Lactic acidosis is a rare but worrisome side effect |
Metformin
|
|
|
|
What Diabetic drug:
Most common side effect is hypoglycemia |
Sulfonylureas (Glipizide, Gliburide, tolbutamide)
|
|
|
|
What Diabetic drug:
Oldest & cheapest of the oral agents |
Sulfonylureas (Glipizide, Gliburide, tolbutamide)
|
|
|
|
What Diabetic drug:
Often used in combination with any of the other oral agents |
Metformin
|
|
|
|
What Diabetic drug:
Also help lower TGs and LDL cholesterol levels |
Metformin
|
|
|
|
What Diabetic drug:
Not safe in settings of CHF |
Thiazolidinediones (TZDs, “glitazones”)
|
|
|
|
What Diabetic drug:
Should not be used in pts with ↑ serum Cr |
Metformin & Sulfonylureas (Glipizide, Gliburide, tolbutamide)
|
|
|
|
What Diabetic drug:
Should not be used in pts with inflammatory bowel disease |
α-glucosidase inhibitors (acarbose)
|
|
|
|
What Diabetic drug:
Hepatic serum transaminase (LFTs) levels should be carefully monitored |
Thiazolidinediones (TZDs, “glitazones”) and Sulfonylureas (Glipizide, Gliburide, tolbutamide)
|
|
|
|
What Diabetic drug:
Not associated with weight gain, often used in overweight diabetics |
Metformin
|
|
|
|
What diabetic drug:
Metabolized by liver, excellent choice in pts with renal dz |
Thiazolidinediones (TZDs, “glitazones” – rosi & pio)
|
|
|
|
What diabetic drug:
Primarily effects postprandial hyperglycemia, taken with meals |
α-glucosidase inhibitors (acarbose)
|
|
|
|
What are the differences between the newer diabetic agents?
|
Sitagliptin (Januvia), Saxagliptin (Onglyza)
Inhibitors of dipeptyl peptidase IV (DPP-4) which affects glucagon-like peptide (GLP-1) aka incretins Prolongs incretin actions, which ↓ glucagon secretion and ↑ insulin secretion, delays gastric emptying Exenatide (byetta), liraglutide (victoza) Exenatide is an analog of exendin, a hormone derived from Glia monster saliva, with actions similar to GLP-1 Lirglutide is a synthetic analog of human GLP-1 Mimic the actions of incretins, which ↓ glucagon secretion and ↑ insulin secretion, delay gastric emptying Not approved for use while on insulin therapy AE: possibly ↑ risk of acute pancreatitis Pramlintide (Symlin) Amylin analog, normally secreted with insulin, ↓ glucagon secretion and gastric emptying Used only in pts taking insulin but in either Type I or II DM |
|
|
|
What are the criteria for the diagnosis of Metabolic Syndrome?
|
Diagnosis based on any 3 of the following:
Abdominal/ truncal obesity: waist circumference >40in (102cm) in men or >35 (88cm) in women TG > 150 HDL <40 in men, < 50 in women BP > 130/ 85 Fasting serum glucose > 100 (or 2hr post oral glucose >140) |
|
|
|
What skin finding can be a sign of insulin resistance?
|
Acanthosis nigricans
|
|
|
|
Hyperosmolar Hyperglycemia Non-ketotic coma (HHNK) is similar in presentation to DKA but differs in what important ways?
|
Occurs only in Type 2 DM
Blood sugar more likely > 800 Lacks ketoacidosis |
|
|
|
You have a well-controlled DM II pt who needs a CT scan with IV contrast. What medication is this pt likely on that must be temporarily held?
|
Metformin
|
|
|
|
Whats the MOA of
α-glucosidase inhibitors (acarbose) |
↓ GI absorption of starch & disaccharides
|
|
|
|
Whats the MOA of Sulfonylureas (Glipizide, Gliburide, tolbutamide)
& Meglitinides |
Stimulates insulin release
|
|
|
|
Whats the MOA of Metformin
|
↓ hepatic gluconeogenesis
|
|
|
|
Whats the MOA of Thiazolidinediones (TZDs, “glitazones” – rosi & pio)
|
↑ tissue glucose uptake and improves insulin sensitivity
|
|
|
|
Whats the MOA of Exenatide & Liraglutide
|
↓ glucagon, ↑ insulin,
|
|
|
|
Whats the MOA of Sitagliptin & Saxagliptin
|
Inhibits DPP-V:
↓ glucagon, ↑ insulin, delays gastric emptying |
|
|
|
Whats the MOA of Pramlintide?
|
An amylin analog which
↓ glucagon & delays gastric empyting |
|
|
|
Which diabetic drugs may cause hypoglycemia?
|
Sulfonylureas (Glipizide, Gliburide, tolbutamide)
Meglitinides |
|
|
|
Which diabetic medications should be avoided in pts with heart failure?
|
Thiazolidinediones (TZDs, “glitazones”)
|
|
|
|
what are the common causes of DKA?
|
Common causes of DKA: usually excess of glucagon, catecholamines, or corticosteroids
Infection (pneumonia, gastroenteritis, UTI) Medication reduction or omission Severe medical illness (MI, CVA, trauma) Undiagnosed DM Dehydration Alcohol or drug abuse Corticosteroids |
|
|
|
What are the steps in the tx of Diabetic ketoacidosis (DKA)?
|
Identify & tx underlying cause
Replace K+ , Ca2+ , Mg2+ & PO43- |
|
|
|
How do we diagnose diabetic gastroparesis?
|
Gastric emptying study
|
|
|
|
What are the treatment options for diabetic gastroparesis?
|
Want to promote GI motility:
Erythromycin Metoclopramide (Reglan) |
|
|
|
General Care of Diabetes Mellitus:
|
Exercise: walking at least 2hr/wk ↓ mortality by 40%
Healthy diet Daily FSBG documented & brought to clinic visit Physical Exam q3-6mo with attention to BP (goal <130/80); weight loss, feet, waist circumference HbA1c q 3mo if > 7.0, q6mo if < 7.0 Amer Diabetic Assoc goal <7.0 Amer Assoc of Clinical Endocrinologists goal <6.5 Urine mircoalbumin q3mo-1yr 24hr urine for protein, Cr, and CrCl is UA protein >100 or high serum Cr Consider annual 24hr urine for protein, Cr, and CrCl Lipid Panel q1 yr: Goal total cholesterol < 150 Goal LDL < 100 (<70 if evidence of vessel disease): use statins or WelChol which has been shown to ↓ HgA1c by 0.47% in users of metformin monotherap Goal HDL > 40 (men) >50 (women) Niacin may worsen insulin resistance Chem. 8 and UA q 1yr Dilated eye exam (r/o retinopathy, glaucoma, cataracts) q1yr Influenza vaccine q1yr Pneumonia vaccine Consider daily ASA 81 mg, ACE-I, statin (Atorvastatin(Lipitor) 10mg) |
|
|
|
In a pt being treated for DKA, what is used to determine when to shut off the insulin infusion?
|
Anion gap – when it is back in the normal range, insulin drip can be stopped
|
|
|
|
Which electrolyte should be given at the beginning of treatment for DKA b/c of its propensity to drop with insulin infusion in these pts?
|
potassium
|
|
|
|
What are Kussmaul respirations, and what is their physiologic purpose?
|
Slow deep breathing (typically, but also can be rapid breathing)
Slower breathing w/ worsening acidosis Purpose is to blow off CO2 & raise pH |
|
|
|
What is the best way to avoid diabetic retinopathy, nephropathy, and neuropathy?
|
Control the diabetes – HbA1c < 7.0
ACE inhibitors or ARBs – to prevent nephropathy Monitor for microalbuminuria Control HTN Annual dilated eye exam – to screen for retinopathy |
|
|
|
How can you track diabetic nephropathy in a diabetic pt?
|
Check microalbumin at least annually
|
|
|
|
What is the pattern & type of sensation lost in diabetic neuropathy?
|
Stocking & glove distribution
|
|
|
|
The surgical intern is called to the bedside of a post-surgical male diabetic pt b/c SOB. The pt denies CP, but cardiac enzymes and an EKG are ordered anyway which reveal an evolving MI. Why doesn’t the diabetic pt have more symptoms indicative of his MI?
|
Sensory loss of diabetic neuropathy effects the nerves involved in angina of chest pain
|
|
|
|
What is the treatment for thyroid storm?
|
ICU admission due to high mortality
R/o infectious cause with blood & urine cx. Empiric antibiotics if infxn is suspected. Hydrate fluid deficit aggressively (unless overt heart failure). Use glucose solutions and replace multivitamins Digoxin if heart failure and/or atrial fibrillation (higher than normal doses may be required) Tylenol for fever. Avoid aspirin which interferes with thyroid protein binding generating more free thyroid β-blockers to control adrenergic stimulation Propanolol IV until adequate tachycardia resolved (must be monitored with continuous EKG and BP monitor) then PO4- q4-6hrs Esmolol IV infusion titrated to resolve tachycardia Thionamide to block new hormone synthesis Propylthiouracil (PTU) – blocks peripheral conversion of T4 to T3, usual DOC Methimazole (Tapazole) – longer acting than PTU, does not block peripheral conversion of T4 to T3 ∴ ideally administered with iopanoic acid (not avail in US) which does this conversion Iodine to block the release of T4 to T3 from the gland, dose at least 1 hour after thionamide to prevent the iodine from being used to create more thyroid hormone Iodide (sodium iodide) IV q6hrs Lugol’s solution PO4- (or to IVF) q 8hrs SSKI (saturated solution of potassium iodide) 5 drops PO4- q6-8hrs +/- Glucocorticoids to ↓ conversion of T4 to T3 and treat the autoimmune process in a hyperthyroid pt with Grave’s Disease |
|
|
|
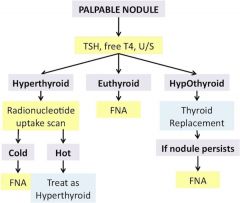
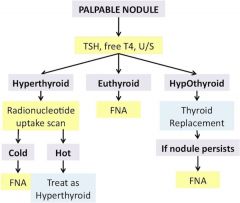
Explain workup of a palpable thyroid nodule
|
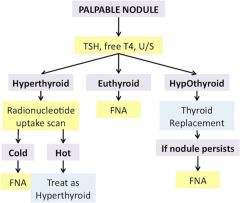
Check TSH, free T4, thyroid sono to measure size and assess for other nodules
If hyperthyroid → radionucleotide uptake scan (no role for radionucleotide scan if euthyroid or hypothyroid) hot nodule → treat as hyperthyroid cold nodule → FNA If hypOthyroid → replace thyroid hormone and monitor for ↓ in nodule size If nodule persists after thyroid replacement → FNA If euthyroid → FNA |
|
|
|
Why must β-blockers be used with caution in diabetic pts?
|
β-blockers mask symptoms of hypoglycemia
|
|
|
|
A pt came into the ER with AMS & you had to administer a glucose infusion empirically b/c there was not a way to determine the blood glucose in a timely fashion. Later it was discovered that the pt was in DKA and subsequently treated inappropriately. In this case was you action careless & harmful?
|
no
|
|
|
|
What is used to determine whether a pt’s hypoglycemia is due to too much insulin production by the body or from too much exogenous insulin administration?
|
Measure C-peptide level
|
|
|
|
What can cause total T4 levels to increase despite free T4 remaining normal?
|
↑ TBG (as seen in pregnancy, OCP use)
|
|
|
|
What is the pathophysiology of Grave’s disease?
|
Autoimmune Abs stimulate TSH receptor of the thyroid, causing excess production & release of thyroid hormone
|
|
|
|
A woman comes to your office c/o neck pain. On exam she is tender and mildly swollen in the thyroid region of the neck. She also reports having some mild anxiety, and at times her heart seems to race. How do you treat this pt’s disease?
|
Dx: subacute thyroiditis
Tx: self-limiting, NSAIDs & β-blockers for symptom control |
|
|
|
How can Grave’s disease be cured?
|
Tx: subtotal thyroidectomy or radioablation using radioactive iodine
PTU or methimazole are used until one of these is performed |
|
|
|
Toxic multinodular goiter & Plummer’s disease are similar in presentation and treatment for Grave’s disease. How are they different?
|
Toxic multinodular goiter: thyroid scan will show the isolated sites (nodules) of excess TH production
Grave’s disease: entire thyroid will show ↑ uptake |
|
|
|
Hypothyroidism can present as what common symptom in a pt?
|
Depression (check TSH)
|
|
|
|
Which antibodies are used to help in the diagnosis of Hashimoto’s thyroiditis?
|
Antimicrosomal & antithyroglobulin Abs
|
|
|
|
A woman comes to your office c/o neck mass. On exam she is not tender but mildly swollen in the thyroid region of the neck. She also reports having some mild anxiety and at times her heart seems to race. How do you treat this pt’s disease?
|
Dx: Hashimoto’s thyroiditis
Tx: Levothyroxine treatment (Synthroid) |
|
|
|
What is the most common form of thyroid carcinoma?
|
Papillary thyroid carcinoma
|
|
|
|
What are the 2 most common complications of a thyroidectomy?
|
Damage to the recurrent laryngeal nerve
Accidental removal of the parathyroid glands which can cause hypocalcemia |
|
|
|
What is the workup for a thyroid nodule?
|
see above
|
|
|
|
Explain next steps following a FNA of a thyroid nodule
|
- FNA follow-up:
- Malignant → needs surgery - Benign → repeat thyroid sono q6mos- 1 yr to make sure no increase in size - If ↑ size → repeat FNA - Nondiagnostic → repeat FNA - Intermediate → repeat thyroid sono in 6 mos - Even if FNA if negative you cannot 100% r/o thyroid cancer. Explain to pt that there is still ~1% chance that this could be cancer and offer to let them choose btw q6mo US surveillance or removal of the nodule (partial vs total thyroidectomy) |
|
|
|
HYQ: Pt has exophthalmos → what is the most likely cause?
|
Dx: Grave’s Disese – antibodies build up & cause inflammation
|
|
|
|
HYQ: How is diabetic gastroparesis diagnosed & treated?
|
Diagnosis made by gastric emptying study
Tx: Metoclopramide (Reglan) |
|
|
|
HYQ: In which of the following hyperthyroid diseases is radioactive iodine most likely to result in hypothyroidism: Graves Disease, toxic multinodular goiter, toxic adenoma?
|
Treatment for Grave’s disease is almost always going to result in hypOthyroidism
|
|
|
|
HYQ: What is the treatment of the most common cause of hyperthyroidism?
|
Mcc of hyperthyroidism = Grave’s Disease
Tx: radionucleotide iodine (preferred), or surgery |
|
|
|
HYQ: What can cause hypoglycemia in a non-diabetic pt?
|
** Diabetes does NOT cause hypoglycemia
Insulinoma Insulin or sulfonylurea use (Factitious disorder, Munchausen’s disorder, Malingering) Check C-peptide levels Alcohol use (fasting) Adrenal insufficiency |
|
|
|
HYQ: What are the S/S of diabetic ketoacidosis (DKA)?
|
Kussmaul respirations
Weight loss Polyuria Polydipsia Nausea & vomiting |
|
|
|
HYQ: What lab abnormalities necessitate obtaining thyroid function testing to r/o thyroid disease?
|
Hyperlipidemia
Unexplained hyponatremia ↑ CPK |
|
|
|
HYQ: A pt with hypothyroidism and ↑ anti-TPO antibodies is at ↑ risk of which type of cancer?
|
Thyroid lymphoma
|
|
|
|
What's the likely cause of hyperthyroidism?
Extremely tender thyroid gland |
Subacute thyroiditis
|
|
|
|
What's the likely cause of hyperthyroidism?
Pretibial myxedema |
Graves Disease
|
|
|
|
What's the likely cause of hyperthyroidism?
Pride in recent weight loss, medical professional |
Abusing levothyroxine
|
|
|
|
What's the likely cause of hyperthyroidism?
Palpation of single thyroid nodule |
Toxic adenoma
|
|
|
|
What's the likely cause of hyperthyroidism?
Palpation of multiple thyroid nodules |
Multinodular goiter
|
|
|
|
What's the likely cause of hyperthyroidism?
Recent study using IV contrast dye (iodine) |
Hyperthyroidism
|
|
|
|
What's the likely cause of hyperthyroidism?
Eye changes: proptosis, edema, injection |
Grave’s Disease
|
|
|
|
What's the likely cause of hyperthyroidism?
H/o thyroidectomy or radioablation of thyroid |
Too much medication
|
|
|
|
What is the next step in the management of a newly-found thyroid nodule in a pt with hyperthyroidism?
|
Check TSH & free T4
|
|
|
|
What is the workup for the underlying cause of DKA?
|
r/o infection (blood cx, urine cx, UA, CXR)
toxicology screen amylase & lipase EKG & cardiac enzymes |
|
|
|
What thyroid abnormalities would you expect to find during pregnancy?
|
↑ TBG & ↑ total T4
normal free T4 |
|
|
|
What is the treatment for proliferative diabetic retinopathy?
|
laser surgery or photocoagulation
|
|
|
|
What is the treatment for peripheral neuropathy?
|
Gabapentin (Neurontin) - analog of the neurotransmitter GABA (doesn’t bind GABA-A or GABA-B receptors, exact MOA unknown)
Pregabalin (Lyrica) – analog of GABA, binds subunit that ↑ Ca2+-dependent release of several NTs Duloxetine (Cymbalta) – selective serotonin & NE reuptake inhibitor (SNRI), potentiating serotonergic & noradrenergic activity in then CNS |
|
|
|
What are the 2 most common causes of primary hyperparathyroidism?
|
Parathyroid adenoma
Parathyroid hyperplasia |
|
|
|
What is the treatment for primary hyperparathyroidism?
|
Surgical parathryoidectomy if one of the following:
Symptomatic (“stones, bones, groans, psychiatric overtone”) Serum Ca2+ > 1.0 above the upper limit of normal Creatine clearance reduced by 30% Bone mineral density scan T-score < -2.5 at any site Age < 50 yrs If adenoma & surgery indicated → removal of only the gland contraining the adenoma & biopsy of 1-3 other glands If hyperplasia & surgery indicated → removal of 3.5 glands and marking the remaining half gland with surgical clip ( or forearm autotransplantation of the gland to remain in cases where recurrence is likely such as MEN type 1) If surery is not recommended or is refused: Prevent worsening by hypercalcemia by avoiding thiazides, lithium, volume depletion, prolonged bed rest, or calcium ingestion > 1000mg/day Adequate hydration (6-8 glasses of water daily) to avoid renal stones Minimize bone resorption via bisphosphonates, exercise, 1000mg Ca2+ daily (except if calcitriol is elevated) and adequate Vit D intake (400-600 IU/day) Routine monitoring of serum Ca2+ (q6mo) serum Cr (q12mo) bone density at the hip, lumbar spine and forearm (q12mo) |
|
|
|
What is the treatment for hyperparathyroidism due to chronic renal disease?
|
Hyperphosphatemia:
Dietary restriction of phosphate (protein) Oral phosphate binders taken with meals Calcium carbonate (tums) & acetate (PhosLo) – most commonly used (NOT calcium citrate (Citracal) which ↑ aluminum absorption) Sevelamer (renagel) nonabsorbable (does not cause hypercalcemia) can be taken with calcium Lanthanum (fosrenol) long term side effects currently unknown Aluminum hydroxide (found in Rulox, antacids) – now avoided b/c of gradual induction of aluminum toxicity Renal osteodystrophy Lessen hyperphosphatemia via the above measures in order to lessen bone resorption Calcitriol, other Vit D analog, or cinacalcet (a calcimimetic) to suppress PTH secretion |
|
|
|
What is a nickname for PTH that aids in remembering its effect on serum phosphate?
|
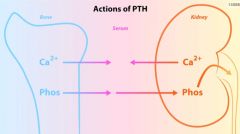
“Phosphate Trashing Hormone”: it pulls phosphate from the bone and trashes it in the urine - ↑ Ca2+ ↓ phophate ↑ Vit D
|
|
|
|
What are the common causes of primary hyperparathyroidism?
|
Single parathyroid adenoma (85%)
Hyperplasia of the glands (15%) |
|
|
|
Why might PTH be elevated in renal disease?
|
Can’t activate Vit D to active form in the kidneys
|
|
|
|
What happens to phosphate in pts with hyperparathyroidism caused by renal disease?
|
↑ phosphate
|
|
|
|
What is the disease a/w shortened 4th and 5th digits on the hand “knuckle, knuckle, dimple, dimple”, and what is the derangement?
|
Albright’s hereditary osteodystrophy
Renal unresponsiveness to PTH |
|
|
|
hypercalcemia + ↑ PTH + ↓ Phosphate
|
Hyperparathyroidism (1° and 3°) – ↑ PTH from adenoma, hyperplasia, MEN1/MEN2A
Familial hypocalciuric hypercalcemia (FHH) inact. mut in Ca sensing receptor in parathyroid & kidney; ↑ Ca2 setpt ±↑ PTH |
|
|
|
hypercalcemia + ↓ PTH + ↑ Phosphate
|
Vit D excess: intoxication or granulomas (Sarcoid/TB/histo/Wegen) which synthesize 1α-hydroxylase, ↑ 1,25Vit D
|
|
|
|
hypercalcemia + ↓ PTH + ↓ Phosphate
|
Malignancy: ↑ PTHrP [lung SqCC, RCC]
Bone mets – activate osteoclasts ↑ lysis Multiple myeloma – ↑ IL-1, ↑ bone lysis *↓PTH = no 1α-hydroxylase= ↓1,25Vit D Note: ↓ PO4 if PTHrP; nml PO4 if lytic, ↓ 1,25VitD Milk-alkali syndrome [too much dairy or OD ca-based antacids) Thiazides [vol depletion ↑ renal reabsorp Ca2+] |
|
|
|
low calcium, ↑ PTH + ↓ Phosphate
|
Vit D def – can be due to lack of sunlight, malabsorption (celiac dz), Cirrhosis, Drugs (anticonvulsants - phenytoin, rifampin, ketoconazole, F-FU/Leucovorin)
Rickets: Type I absent 1α-hydroxylase (↓ 1,25VitD, tx with Calcitriol) Type 2 absent receptors for Calcitriol, ↑ 1,25Vit D |
|
|
|
low calcium, ↑ PTH + ↑ Phosphate
|
Pseudohypoparathyroidism: Aut Dom, end-organ resistance to PTH
(including ↓ 1α-hydroxylase) Chronic Renal failure (2° hyperpara) – ↓ 1,25VitD, ↑ PO4 from ↓ clearance |
|
|
|
low calcium, low PTH, high phosphate
|
HypOparathyroidism: sporadic, or iatrogenic (s/p thyroid surgery, neck radiation) Wilson’s, hemochromatosis,
hypoMg (Mg cofactor for adenylate cyclase, cAMP required for PTH activat) |
|
|
|
what are the pitfalls in measuring calcium?
|
Physiologically active Ca2+ is free (ionized)
Serum Ca2+ reflects total Ca2+ (bound + unbound) and ∴ influenced by albumin (main Ca2+ binding protein) Corrected Ca2+ = measured Ca2+ + [0.8 x (4 – albumin)] Alkalosis will cause more Ca2+ to be bound to albumin → therefore total Ca2+ may be normal, but ↓ ionized Ca2+ Best to measure ionized Ca2+ directly |
|
|
|
Signs/ Symptoms of hypercalcemia in hyperparathyroidism?
|
“STONES”:
renal stones nephrocalcinosis: polyuria, polydipsia, uremia “BONES”: ↑ osteoclastic activity osteitis fibrosa cystica: rare today b/c of early detection commonly involves the jaw/ fingers, histologically the pathognomonic features are ↑ osteoclasts on surface of the bone & replacement of normal cellular & marrow elements with fibrous tissue – xrays show periosteal resorption osteoporosis osteomalacia osteoarthritis “GROANS”: GI manifestations: constipation, nausea, vomiting peptic ulcers pancreatitis “PSYCHIATRIC OVERTONES”: Lethargy, fatigue, depression Memory loss Psychosis Personality changes Confusion, stupor, coma Other: Proximal muscle weakness, keratitis, conjunctivitis, HTN, itching |
|
|
|
What are the symptoms of hyperprolactinemia? (high yield!)
|
Premenopausal female → Hypogonadism
Infertility, Oligo- or amenorrhea Rarely galactorrhea Post-menopausal → Already hypogonadal, less symptoms, +/- galatorrhea Male: ↓ testosterone: ↓ libido, impotence, ↓ sperm ct (infertility), gynecomastia +/- galactorrhea |
|
|
|
Whats the workup if you suspect a prolactinoma?
|
Prolactin levels
TSH MRI of brain |
|
|
|
What is the treatment for a prolactinoma?
|
First step: Dopamine agonist – Cabergoline (Dostinex) > bromocroptine or pergolide
If Dopamine agonist ineffective → switch to a 2nd agonist If 2 dopamine agents are ineffective → Transphenoidal surgery If female with adenoma >3cm and desire to become pregnant (during which time the dopamine agonist is withheld) → transphenoidal surgery even if the dopamine agonist is effective If large adenoma is surgically removed → radiation therapy after surgical debulking |
|
|
|
What are the S/S of acromegaly? What tests can be used to confirm the diagnosis?
|
Note: the average time from onset to diagnosis is 12yrs and it presents with the following symptoms:
Enlarged jaw (teeth spread apart), nose & frontal bones (coarse facial features), hand & feets (increase in ring, glove, shoe size) Soft tissue growth: voice deepens, macroglossia (teeth indentations in tongue), carpal tunnel syndrome and other entrapment syndromes, hypertrophy of synovial tissue and cartilage → arthropathy cardiovascular disease: HTN, LVH, diastolic dysfxn Glucose intolerance in 50%, DM in 10% Diagnostic testing: Screening: measure serum levels of insulin-like growth factor 1 (IGF-1) Confirm diagnosis: with oral glucose suppression test (75g glucose → measure GH at 1 hr and 2hr → if GH conc is > 1ng/mL = acromegaly) If testing positive for acromegaly → pituitary MRI to eval for mass or empty sella |
|
|
|
What is the treatment for acromegaly?
|
Transphenoidal resection of pituitary adenoma or external beam radiation
If unable to resect adenoma → somatostatin analog – Octreotide (Sandostatin) or lanreotide (Somatuline) – inhibits GH secretion If somatostatin analog ineffective → cabergoline (dopamine agonist that inhibits GH secretion) Bromocriptine is less effective than is cabergoline if cabergoline ineffective → pegvisomant (GH receptor antagonist) |
|
|
|
What is the usual presentation of Sheehan syndrome? (HYQ!)
|
Postpartum hemorrhage → hypotension → infarction of the pituitary gland → hypopituitarism
Severe Sheehan → first few days-weeks after delivery → lethargy, anorexia, weight loss, and inability to lactate mid Sheehan → wks, months, or yrs after delivery → mild fatigue, anorexia, weight loss; failure of postpartum lactation, failure to resume menses, and loss of sexual hair possible ACTH deficiency → hypocortisolism Possible TSH deficiency → hypothyroidism |
|
|
|
Which 2 hormone levels are decreased in response to excess prolactin?
|
↓ LH & ↓ FSH (leads to hypogonadal symptoms of infertility, gynecomastia, galatorrhea)
|
|
|
|
What common medications can cause hyperprolactinemia?
|
Medications that antagonize dopamine
Neuroleptics (Risperidone) Domperidone Metoclopramide Methyldopa |
|
|
|
What is the visual field defect classically assoc with prolactinoma?
|
Bilateral hemianopsia (mass effect of tumor in sella turcica)
|
|
|
|
What are the first-line drugs used to treat prolactinomas?
|
Dopamine agonists (Cabergoline > bromocriptine, pergolide)
|
|
|
|
What substance is used in screening for acromegaly? What study is used to confirm the diagnosis?
|
Screening: measure serum IGF-1 (can’t measure GH b/c it varies during the day)
Confirmatory: oral glucose suppression test Give 75g glucose → measure GH at 1 hr and 2hr → if GH conc is > 1ng/mL = acromegaly |
|
|
|
What complications can result from acromegaly?
|
Cardiac failure
Diabetes Spinal cord compression Compression of optic nerve → vision loss |
|
|
|
What is Sheehan syndrome?
|
Postpartum hemorrhage → pituitary infarction → pituitary dysfunction
|
|
|
|
What changes in serum potassium (K+) & serum sodium (Na+) would be seen in patients with excessive aldosterone [Conn’s Syndrome] or adrenal insufficiency [Addison’s Disease]?
|
Addison’s is due to Adrenal Atrophy and Absence of hormone production
Conn’s is HYPERaldosteronism due to an aldosterone-secreting tumor → muscular weakness, hypertension, hypokalemia, alkalosis- Conn’s are “HYPER”-aldosterone, but muscles are really weak Conn’s Syndrome: HypOkalemia, HYPERnatremia Addison’s Disease: HYPERkalemia, HypOnatremia |
|
|
|
What mineralcorticoid medication is used to tx pts with hypoaldosteronemia [Addison’s Disease] ?
|
Fludrocortisone (Florinef)
|
|
|
|
What aldosterone antagonist can be given to treat HYPERaldosteronemia? What effect would this drug have on serum K+ levels?
|
Spironolactone (Aldactone): would ↑ serum K+
|
|
|
|
What condition(s) do you see ↑ aldosterone : ↓ renin?
|
Primary Hyperaldosteronism:
Conn’s syndrome (adrenal adenoma secreting aldosterone) |
|
|
|
What condition(s) do you see ↑ aldosterone : ↑ renin?
|
Secondary Hyperaldosteronism:
Renovascular disease, Renin-secreting tumor CHF, cirrhosis, nephrotic syndrome Hypovolemia, diuretic use |
|
|
|
What condition(s) do you see ↓ aldosterone : ↓ renin?
|
Non-aldosterone mineralcorticoid excess:
Cushing’s syndrome (see below) Chronic licorice ingestion |
|
|
|
What are some causes of Cushing’s syndrome?
|
Excess corticosteroid administration (most common)
Pituitary adenoma (Cushing’s disease) – producing ACTH Paraneoplastic ACTH production – small cell lung cancer Adrenal tumor – producing cortisol |
|
|
|
What can a high dose of dexamethasone suppress? What can it not suppress?
|
If am cortisol suppressed → pituitary adenoma producing ACTH (Cushing’s disease)
If am cortisol not suppressed → adrenal tumor producing cortisol, or ectopic ACTH secreting tumor (small cell lung ca) |
|
|
|
What are the electrolyte abnormalities found in hyperaldosteronism?
|
hypOkalemia, HTN, metabolic alkalosis (↓ K+, mildy ↑ Na+)
|
|
|
|
A pt with a high plasma aldosterone concentration and low plasma renin activity ratio has what condition? Which medication could be used to treat this condition until definitive therapy can be undertaken?
|
Dx: Conn’s Syndrome
Tx: Spironolactone (Aldactone) |
|
|
|
Increased skin pigmentation is seen in pts with which kind of adrenal insufficiency?
|
Dx: Addison’s disease = Primary adrenal insufficiency
Pathophys: autoimmune destruction of adrenal cortex |
|
|
|
Which steroid is used to replace mineralcorticoid deficiency?
|
Fludrocortisone (Florinef)
|
|
|
|
A pt on chronic steroid therapy contracts pneumonia that requires admission into the ICU. What should the admitting physician make sure to do with the pt’s medications and why?
|
Increase the dose of steroids
(during times of stress, adrenals tend to ↓ activity) |
|
|
|
What is the likely condition of a female infant with virilization of the genitalia and hypotension?
|
Congenital adrenal hyperplasia → 21-α hydroxylase def
|
|
|
|
What serum lab abnormality would you see in a 17-α hydroxylase def and in 21-α hydroxylase deficiency?
|
17-α: hypOkalemia, mildly ↑ Na+, HTN
21-α: hypOnatremia, hyperkalemia, hypotension |
|
|
|
A 23 yo F presents with c/o episodic anxiety, palpitations, and sweating. She managed to measure her BP during one of the episodes which revealed 165/103, a large increase over her normal 118/77. What tests should be ordered to aid in diagnosis of her condition?
|
Dx: Pheochromocytoma
Labs: urinary catecholamines, metanephrines & vanillylmadelic acid (VMA), plasma free metanephrines |
|
|
|
What is the medical management of the above pt’s condition prior to her having the necessary surgery for a definitive cure?
|
Tx: α-blockade before β-blockers
|
|
|
|
A pt with acromegaly is found to have elevated Ca2+ on a blood draw during a work up of his peptic ulcer disease. What is the diagnosis of this pt?
|
Dx: MEN 1 syndrome
Acromegaly, ↑ Ca2+ from hyperparathyroidism, peptic ulcer disease (Zollinger-Ellison syndrome) |
|
|
|
What tumors are associated with MEN 2a?
|
Medullary thyroid cancer
Hyperparathyroidism Pheochromocytoma |
|
|
|
HYQ: A pt with ↑BP, palpitations, HA, excessive perspiration is found to have elevated urine vanillymandelic acid levels. What effect would giving a β-blocker have on this pt?
|
Dx: Pheochromocytoma
Giving β-blockers will rapidly raise the blood pressure more |
|
|
|
HYQ: What is lactotroph adenoma? What is a somatotroph adenoma?
|
Lactotroph adenoma: Prolactin secreting
Somatotroph adenoma: GH secreting |
|
|
|
HYQ: Most likely cause of ↑ PTH + ↓ serum Ca2+ + ↑ serum phosphate?
|
Renal failure with Vit D Deficiency
|
|
|
|
HYQ: Of DHEA, DHEA-S, and testosterone, which is made only by the adrenal and is more specific marker for an androgen-producing adrenal tumor in a woman?
|
DHEA-sulfate
|
|
|
|
HYQ: What is the most specific lab finding in making the diagnosis of primary hyperaldosteronism?
|
High PAC: PRC ratio
|
|
|
|
What is the next step in the management of a pt with hyperprolactinemia not due to an obvious drug cause?
|
MRI of the brain (sella turcica)
Check TSH |
|
|
|
What is the next step in the management of a pt found to have an absent pituitary on MRI (empty sella)? |
Reassurance if not symptomatic
|
|
|
|
What drugs are known for causing ↑prolactin levels?
|
Phenothiazine, thioridazine, prochlorperazine, promethazine |
|
|
|
What are the indications for surgical parathyroidectomy?
|
Symptomatic |
|
|
|
(H/P) = rhinorrhea (i.e., nasal congestion & increased secretions), nonproductive cough; nasal and throat irritation, sneezing, possible fever, no exudates or productive coughLabs = negative throat culture
|
Upper respiratory infections (URI)Inflammation of the upper airways most commonly caused by rhinovirus, coronavirus, or adenovirus
|
Treatment = rest, analgesia, treat symptoms; antibiotics are NOT helpful
|
|
|
H/P = sore throat, tonsillar exudates (more common w/ bacterial infection), lymphadenopathy, possible nasal congestion; fever, red and swollen pharynx,
|
PharyngitisPharyngeal infection caused by group A β-hemolytic streptococci (“strep throat”) or common cold virusComplications = untreated infection can cause rheumatic heart disease or glomerulonephritis (characterized by a high antistreptolysin O titer)
|
Labs = throat culture grows streptococcal species, and rapid streptococcal Ag test is + for strep throat; - culture suggests viral etiologyTreatment = self-limited; β-lactam antibiotics (e.g., penicillin, amoxicillin, etc.) reduce infection time
|
|
|
H/P = similar to streptococcal pharyngitis, tonsillar exudates; ear pain, difficulty swallowing; possible high fever.
|
Tonsillar infectionsSpread of streptococcal pharyngitis to palatine tonsils leading to tonsillar inflammation (i.e., tonsillitis)Complications = airway compromise; abscess (requires intravenous [IV] antibiotics and surgical incision and drainage followed by tonsillectomy after resolution to prevent recurrence)
|
Treatment = self-limited; β-lactam antibiotics (e.g., penicillin, amoxicillin, etc.) reduce infection time
|
|
|
H/P = myalgias, vomiting, diarrhea; high fevers (typically >100°F/37.8°C and can reach up to 106°F/41°C), arthralgias, sore throat, nasal congestion, nonproductive cough, nausea, lymphadenopathy
|
Viral influenzaGeneralized infection with URI symptoms caused by one of several influenza viruses
|
Labs = serologic tests are definitive, but rarely required for diagnosisTreatment = treat symptoms; fluid intake important to replace losses from vomiting and diarrhea; self-limited (several days) but amantadine may shorten course of disease; elderly patients, health care workers, immunocompromised patients, and patients with lung disease should receive annual vaccine to reduce risk of infection
|
|
|
pain over infected sinuses, purulent nasal discharge, maxillary toothache pain; pain on palpation of affected sinuses, illumination test (i.e., light held close to sinuses) may detect congestion in frontal of maxillary sinuses, but is unreliable
|
SinusitisSinus (most maxillary)infection associated w/ allergic rhinitis, barotrauma, viral infection, prolonged nasogastric tube placement, or asthmaAcute sinusitis is usually caused by Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, viral infectionAcute sinusitis can spread to CNS & cause meningitis if untreated.Chronic sinusitis (lasting >3 months) is usually caused by sinus obstruction, anaerobic infection; patients with diabetes mellitus (DM) predisposed to mucormycosis
|
Radiology = radiograph shows opacification and fluid levels in affected sinuses; computed tomography (CT) is diagnostic; frequently radiologic tests are not needed because of clinical diagnosisTreatment = treat symptoms; amoxicillin × 2 weeks in acute cases and for 6–12 weeks in chronic cases; surgical drainage or correction of anatomic obstruction may be required for full cure
|
|
|
H/P = productive cough, sore throat; fever, wheezing, tight breath sounds
|
Acute bronchitis Inflammation of trachea and bronchi caused by spread of URI or exposure to inhaled irritants |
Labs = sputum culture only performed in persistent cases and is most commonly -;Radiology = chest x-ray (CXR) may show only mild congestionTreatment = self-limited if viral (most cases); patient groups with an increased risk of bacterial infection (e.g., smokers, elderly, patients with other lung disease) may be given antibiotics (e.g., fluoroquinolones, tetracycline, or erythromycin)
|
|
|
H/P = pleuritic chest pain; decreased breath sounds, dullness to percussion, tachypnea, productive or nonproductive cough, dyspnea, chills, night sweats, rales, wheezing, egophony (i.e., change in voice quality heard during auscultation over a consolidated region of lung), tactile fremitusLabs = increased white blood cell count (WBC) (slight increase with viral cause, significant increase with bacterial or fungal cause) with left shift (more immature forms); + sputum culture
|
PneumoniaInfection of the bronchoalveolar tree can be caused by common nasopharyngeal bacteria (i.e., typical pneumonia) or bacteria, viruses, or fungi from the surrounding environment (i.e., atypical pneumonia); common causes vary by age group
|
Treatment = viral pneumonia is self-limited and only requires supportive care; bacterial and fungal pneumonias require antibiotics (started as broad coverage and changed to pathogen-specific therapy as culture results become availableAdmission=elderly, multiple medical comorbidity, significant laboratory abnormalities, multilobar involvement, signs of sepsis
|
|
|
H/P=a non-productive cough be used for influenza A virus
|
Viral Pneumonia Viral (influenza, parainfluenza, adenovirus, cytomegalovirus, respiratory syncytial virus) Most common pneumonia in children; common in adults
|
Treatment=Self-limited; amantidine may
|
|
|
H/P=pneumonia, high fevers, pleuritic pain, productive cough
|
Streptococcus pneumoniae Most common pneumonia in adults; higher risk of infection in sickle cell patients
|
Treatment=β-lactams, macrolides(azithromycin, clarithromycin, erythromycin)
|
|
|
H/P=pneumonia, slower onsetPatients with COPD; higher risk of infection in patients with sickle cell disease
|
Haemophilus influenzae
|
Treatment=β-lactams, TMP-SMX
|
|
|
H/P=pneumonia, abscess formationNosocomial pneumonia, immunocompromised patients
|
Staphylococcus aureus
|
Treatment=β-lactams
|
|
|
H/P=pneumonia, “Currant-jelly” sputum; Alcoholics, patients with high risk of aspiration, patients staying in the hospital for extended amounts of time, sickle cell patients
|
Klebsiella pneumoniae
|
Treatment=Both cephalosporins and aminoglycosides (gentamicin, tobramycin)
|
|
|
H/P=pneumonia, Young adults, possible rash; + cold-agglutinin test
|
Mycoplasma pneumoniae
|
Treatment=Macrolides (azithromycin, clarithromycin, erythromycin)
|
|
|
H/P=pneumonia, rapid onsetChronically ill and immunocompromised patients, patients with cystic fibrosis, nosocomial pneumonia
|
Pseudomonas aeruginosa
|
Treatment=Fluoroquinolones (ciprofloxacin), aminoglycosides, generation 3rd-cephalosporins
|
|
|
H/P=pneumonia Slow onset, nausea, diarrhea, confusion, or ataxia
|
Legionella pneumophilaAssociated with aerosolized water (air-conditioners)
|
Treatment=Macrolides, fluoroquinolones
|
|
|
H/P=pneumonia, Slow onset, frequent sinusitisMore common in very young and elderly
|
Chlamydia pneumoniae
|
Treatment=Doxycycline, macrolides
|
|
|
H/P=pneumonia, Respiratory distress, lethargyNeonates and infants
|
Group B Streptococcus
|
Treatment=β-lactams
|
|
|
H/P=pneumoniaNosocomial pneumonia, elderly patients
|
Enterobacter sp.
|
Treatment=TMP-SMX
|
|
|
H/P=pneumonia, Less severe symptoms; subacute disease for initial history
|
FungiTravelers to southwest U.S. (coccidioidomycosis), caves (histoplasmosis), or Central America (blastomycosis)
|
Treatment=Antifungal agents (amphotericin B, ketoconazole)
|
|
|
H/P=pneumonia, Slow onset, GI symptomsImmunocompromised patients (HIV) (CD4 count <200)
|
Pneumocystis carinii (fungi-like)
|
Treatment=TMP-SMX
|
|
|
H/P = cough, hemoptysis, dyspnea, weight loss, night sweats; fever, ralesRisk factors = immunosuppression, alcoholism, lung disease, DM, advanced age, homelessness, malnourishment, crowded living conditions, and close proximity to infected patientsRadiology = CXR may show apical fibronodular infiltrates (reactivated disease), lower-lobe infiltrates (primary lesion), and calcified granulomas/lymph nodes (Ghon complexes)
|
Tuberculosis (TB)Pulmonary infection caused by Mycobacterium tuberculosisFollowing primary infection, disease enters inactive state; untreated infections can become reactivated (most active cases) and extend to extrapulmonary sites (i.e., miliary TB)
|
Labs = + purified protein derivative (PPD) tuberculin skin test is screening test for exposure (followed by a CXR to look for signs of TB), anergy test (subcutaneous Candida preparation) in addition to a PPD to check for an appropriate immune response; + sputum acid-fast stain, + culture (may take weeks, so not useful in planning therapy); 1 bronchoscopy is considered equal to 3 sputum samples for specimen collectionTreatment = respiratory isolation for any inpatient; report all diagnosed cases to local and state health agencies; multidrug treatment initially w/ isoniazid (INH), rifampin, pyrazinamide, & ethambutol followed by INH & rifampin for a total of 6 months; give vitamin B6 w/ INH to prevent peripheral neuritis (INH competes with vitamin B6 as a cofactor in neurotransmitter synthesis, so supplemental vitamin B6 helps offset this competition); give prophylactic INH to patients with an asymptomatic positive PPD who are immunocompromised, have a history of IV drug abuse (IVDA), are <35 years of age, a history of close contact with TB-infected people, or are indigent patients (reporting is unnecessary unless TB is diagnosed); monthly sputum acid-fast tests should be performed during therapy to confirm adequate treatment
|
|
|
H/P = acute dyspnea and pulmonary decompensation in setting of serious underlying condition; cyanosis, tachypnea (begins within 48 hours of initial insult), wheezing, rales, rhonchiLabs = arterial blood gas (ABG) shows respiratory alkalosis, decreased O2 (caused by impairment of O2 transfer to pulmonary capillaries by pulmonary edema), decreased CO2 (caused by hyperventilation); other tests should reflect underlying pathology; Swan-Ganz catheterization shows wedge pressure <18 mm Hg; Pao2:Fio2 ratio will be <200 during mechanical ventilation
|
Acute respiratory distress syndrome (ARDS)Acute respiratory failure caused by sepsis, trauma, aspiration, near drowning, drug overdose, shock, or lung infection that is characterized by refractory hypoxemia, decreased lung compliance, and pulmonary edema, and carries a high mortalityEtiology=ARDS: Aspiration/Acute pancreatitis/Air or Amniotic embolism, Radiation, Drug overdose/Diffuse lung disease/DIC/Drowning, Shock/Sepsis/Smoke inhalation.
|
Radiology = bilateral pulmonary edema and infiltratesTreatment = treatment in intensive care unit with mechanical ventilation frequently required; mechanical ventilation should include positive end-expiratory pressure (PEEP), increased inspiratory times, and Fio2 adjusted to maintain O2 saturation (Sao2) >90%; underlying cause must be treated; keep fluid volumes low to prevent pulmonary edema; use of extracorporeal membrane oxygenation (ECMO) may improve outcome in severe cases
|
|
|
H/P = prolonged expiratory duration, accessory muscle use, cough, dyspnea, wheezing, chest tightness; tachypnea, tachycardia, decreased breath sounds, wheezing, possible pulsus paradoxus; cyanosis, decreased arterial O2 saturation (Sao2) on pulse oximetry, or difficulty talking in severe attacks
|
AsthmaReversible airway obstruction secondary to bronchial hyperactivity, acute airway inflammation, mucous plugging, and smooth muscle hypertrophyExacerbations (i.e., sudden bronchoconstriction and airway inflammation) are triggered by allergens (e.g., dust, smoke, pollen, fumes, pet dander), URI, exercise, stress, β-antagonist drugs, aspirin (rare), and sulfites (rare)Risk factors = family history of asthma, allergies, atopic dermatitis, low socioeconomic statusDisease can be worse in childhood and improve with age
|
Labs = peak expiratory flow rate (PEFR) decreased and used along with clinical symptoms and frequency of medication use to classify disease as mild intermittent, mild persistent, moderate persistent, or severe (see Table 2-8); PFT show decreased FEV1, normal/elevated DLcoRadiology = CXR shows hyperinflationTreatment=Inhaled short-acting β2-agonist IV corticosteroids if persistent during exacerbation. daily corticosteroid inhaler (+long long-acting β2-agonist, considerleukotriene inhibitor or theophylline) from Mild Persisent up
|
|
|
prolonged, nonresponsive asthma attack
|
Status asthmaticus
|
Treatment=aggressive bronchodilator therapy, corticosteroids, O2, and, possibly, intubation
|
|
|
H/P = productive cough, recurrent respiratory infections, dyspnea; wheezing, rhonchihistory of productive cough for 3 months of the year for >2 years
|
Chronic bronchitisChronic bronchial inflammation associated with tobacco use (common) or chronic asthma (uncommon); occurs in continuum with emphysema as chronic obstructive pulmonary disease (COPD)“blue bloaters,” because secondary development of cor pulmonale causes cyanosis and peripheral edema;Complications = emphysema frequently results without smoking cessation
|
Labs = PFTs show gradually worsening signs of obstructive disease as condition progressesTreatment = tobacco cessation, antibiotics given for URI because of the greater incidence of a bacterial etiology; bronchodilators during exacerbations
|
|
|
H/P = dyspnea, possible productive cough, morning headache; barrel-chested, pursed-lip breathing, prolonged expiratory duration, decreased heart sounds, decreased breath sounds, wheezing, rhonchi, accessory muscle use, jugular venous distension (JVD); exacerbations present with worsening symptoms
|
Emphysema (later stage—COPD)Long-term tobacco use leads to chronic bronchoalveolar inflammation associated with release of proteolytic enzymes by neutrophils and macrophages; destruction of alveoli and bronchioles results with panacinar airspace enlargement and a decreased capillary bedLess common form (appears at younger age) caused by α1-antitrypsin deficiencycommon form of emphysema has a centrilobular distribution, whereas the form associated with α1-antitrypsin deficiency has a panlobular distribution.
|
Labs = PFTs show decreased FEV1, decreased FEV1/FVC, increased total lung capacity (TLC), decreased PEFR; ABG during acute exacerbations shows decreased O2, increased CO2 (beyond a baseline increase already seen in these patients)Radiology = CXR shows flat diaphragm, hyperinflated lungs, subpleural blebs and bullae (i.e., small fluid-filled sacs), and decreased vascular markingsTreatment = smoking cessation; supplemental O2; inhaled, short-acting β2-agonists; inhaled anticholinergics; inhaled corticosteroids and long-acting β2-agonists may be useful in severe cases; antibiotics given for respiratory infections; pneumococcal and influenza vaccines important to reduce infection risk; enzyme replacement may have a role in α1-antitrypsin deficiency therapy; lung transplant may be an option in late severe disease
|
|
|
H/P = copious sputum, persistent, productive cough; hemoptysis, frequent respiratory infections, dyspnea; wheezing, rales, and hypoxemia
|
D. BronchiectasisPermanent dilation of small and medium bronchi because of destruction of bronchial elastic componentsOccurs secondary to chronic airway obstruction, chronic tobacco use, TB, fungal infections, severe pneumonia, or cystic fibrosisComplications = cor pulmonale, massive hemoptysis, abscess formation
|
Radiology = multiple cysts and bronchial crowding seen on CXR; CT shows dilation of bronchi, bronchial wall thickening, bronchial wall cystsTreatment = pulmonary hygiene (e.g., hydration, sputum removal), chest physical therapy; antibiotics given when sputum production increases; inhaled β2-agonists and corticosteroids may reduce symptoms; resection of severely diseased regions of lung indicated for hemorrhage, substantial sputum production, or inviability
|
|
|
H/P = possibly asymptomatic; hemoptysis, cough, dyspnea, pleuritic chest pain, fatigue, weight loss, frequent pulmonary infections;
|
Lung cancerMost frequently associated with tobacco use (~90% of cases); also can be caused by occupational exposures (e.g., smoke, asbestos)Complications = poor prognosis (~10% 5-yr survival); recurrence common for primary tumors
|
Radiology = initially seen on CXR or CT as pulmonary nodule; bronchoscopy with biopsy and brushings or fine needle aspiration of lesion are diagnosticTreatment = use of surgical resection, chemotherapy, and/or radiation therapy based on type of lung cancer (large cell, squamous cell, or adenocarcinoma vs. small cell) and staging of disease (based on local extension, lymph node involvement, and presence of metastases) (see Table 2-11)
|
|
|
miosis, ptosis, and anhidrosis
|
Horner's syndrome
|
|
|
|
Horner's syndrome plus brachial plexus involvement
|
Pancoast's syndrome
|
|
|
|
obstruction of venous drainage through superior vena cava and associated head swelling and CNS symptoms
|
Superior vena cava syndrome
|
|
|
|
Lung Cancer, CentralCavitary lesions; direct extension to hilar lymph nodesParaneoplastic Syndromes= Hypercalcemia, Dermatomyositis
|
Squamous cell carcinoma
|
Treatment=Chemotherapy as primary, Radiation Therapy as adjuvant
|
|
|
Lung Cancer,PeripheralWide metastases; can be caused by asbestos; pleural effusions show increased hyaluronidase levels; bronchiolar cancer is subtype that is low grade and occurs in single nodulesParaneoplastic Syndromes= DIC, Thrombophlebitis,, Microangiopathic hemolytic anemiaDermatomyositis
|
Adenocarcinoma
|
Treatment for all non-small:no lymph node involvement beyond ipsilateral hilar nodes, No mediastinal invasion, no metastases->Surgical resection, radiation as primary or postop adjuvant, chemo as adjuvant
|
|
|
Lung Cancer, CentralRapidly growing; early distant metastases; several paraneoplastic syndromesParaneoplastic Syndromes= Cushing's syndrome, Syndrome of inappropriate ADH secretion (SIADH), Ectopic growth hormone and ACTH secretion, Peripheral neuropathy, Subacute cerebellar degeneration, Eaton-Lambert syndrome (similar presentation to myasthenia gravis), Subacute sensory neuropathy, Limbic encephalitis, Dermatomyositis
|
Small cell carcinoma
|
Treatment for all non-small:has extension to ipsilateral mediastinal nodes, No mediastinal invasion or metastases->radiation as primary, surgery if tumor shrinik, chemo as induction for surgery or adjuvant
|
|
|
Lung Cancer, PeripheralLate distant metastases, early cavitationParaneoplastic Syndromes=Gynecomastia, Dermatomyositis
|
Large cell carcinoma
|
Treatment for all non-small:Mediastinal invasion, distant nodes, and/or metastases-> chemo or radiation as palliative
|
|
|
H/P = hoarseness that worsens with time (over several weeks), dysphagia, ear pain, hemoptysis; laryngoscopy may visualize mass and airway obstruction
|
Laryngeal cancerSquamous cell cancer of the larynx associated with tobacco and alcohol use
|
Labs = biopsy is diagnosticRadiology = magnetic resonance imaging (MRI) or CT with contrast detects soft tissue mass; PET may be useful for detecting lesions earlier in disease courseTreatment = partial or total laryngectomy used to remove lesions confined to larynx; radiation therapy can be used in conjunction with surgery or as sole therapy in extensive lesions; advanced cases may require combination of surgery, radiation, and chemotherapy to resect lesion while preserving surrounding structures
|
|
|
H/P = progressive exercise intolerance, dyspnea; dry crackles, JVD, tachypnea, and possible digital clubbingpatients >50 years of ageLabs = PFT will show restrictive lung disease characteristics (e.g., FEV1/FVC normal, decreased FVC, decreased TLC, decreased compliance); bronchioalveolar lavage shows increased polymorphonuclear (PMN) cells; lung biopsy demonstrates extensive fibrosis and loss of parenchymal architectureRadiology = CXR shows reticulonodular pattern and “honeycomb” lung in advanced cases; CT will show lung fields with “ground glass” appearance
|
Idiopathic pulmonary fibrosis (IPF)Inflammatory lung disease causing lung fibrosis;Complications = progressive lung fibrosis with frequent mortality within 5 years; most patients do not survive sufficiently long to receive a lung transplant
|
Treatment = corticosteroids combined with either azathioprine or cyclophosphamide are helpful in some patients (follow PFTs to evaluate effectiveness); worsening PFTs should indicate need to change drug regimen; lung transplant is frequently indicated
|
|
|
H/P = cough, malaise, weight loss, dyspnea, arthritis (knees, ankles), chest pain; fever, erythema nodosum (i.e., tender red nodules on shins and arms), lymphadenopathy, vision loss, cranial nerve palsiesLabs = increased serum angiotensin-converting enzyme (ACE), increased calcium, hypercalciuria, increased alkaline phosphatase, decreased WBC, increased erythrocyte sedimentation rate (ESR); PFT show decreased FVC, decreased DLcoRadiology = CXR shows bilateral hilar lymphadenopathy, pulmonary infiltrates (ground glass appearance)
|
SarcoidosisSystemic disease characterized by noncaseating granulomas, hilar adenopathy, pulmonary infiltrates, and skin lesions; unknown etiologyRisk factors = blacks > whites; females > males; most frequently occurs between 10 and 40 years of agePatients with sarcoidosis frequently show anergy (no reaction) to a skin test or PPD.
|
Treatment = occasionally self-resolving; corticosteroids in chronic cases; cytotoxic drugs can be used with failure of steroid therapy; lung transplantation is rarely required (only in severe cases)
|
|
|
H/P = symptoms begin when significant pulmonary fibrosis has occurred (several years between exposure to onset of symptoms is common); cough, dyspnea on exertion, heavy sputum production; rales and wheezing are heard on auscultation, digital clubbing
|
PneumoconiosesInterstitial lung diseases that result from long-term occupational exposure to substances that cause pulmonary inflammation
|
Labs = PFT show a restrictive patternRadiology = CXR shows multinodular opacities; CT shows signs of pulmonary fibrosisTreatment = usually, no successful treatments are available for these conditions; prevention (e.g., proper air filters, following safe-handling recommendations) is vital to avoiding disease
|
|
|
H/P = hemoptysis, dyspnea, recent respiratory infectionLabs = + anti-GBM Ab; PFT show restrictive pattern, but increased DLco (caused by the presence of Hgb in alveoli); urinalysis shows proteinuria and granular casts; renal biopsy shows crescentic glomerulonephritis and IgG deposition along glomerular capillaries
|
Goodpasture's syndromeProgressive autoimmune disease of lungs and kidneys caused by anti-glomerular basement membrane (anti-GBM) antibodies and characterized by intra-alveolar hemorrhage and glomerulonephritis
|
Radiology = CXR shows bilateral alveolar infiltrationTreatment = plasmapheresis to remove auto-antibodies; corticosteroids and immunosuppressive agents
|
|
|
H/P = ulcerations of nasopharynx, fever; hemoptysis, dyspnea, myalgias, chronic sinusitis; additional symptoms from renal (e.g., mild hematuria), CNS (e.g., hearing loss, sensory neuropathy, cranial nerve dysfunction), ophthalmologic (e.g., conjunctivitis, proptosis, corneal ulceration, diplopia), and cardiac (e.g., arrhythmia) involvementLabs = + cytoplasmic antineutrophil cytoplasmic antibody (c-ANCA); biopsy shows noncaseating granulomas; renal biopsy detects vasculitic process
|
Wegener granulomatosisRare disease with granulomatous inflammation and necrosis of lung and other organ systemsCaused by systemic vasculitis that mainly affects lung and kidney causing formation of noncaseating granulomas and destruction of lung parenchymaComplications = rapidly fatal if untreated
|
Treatment = cytotoxic therapy (e.g., cyclophosphamide), corticosteroids
|
|
|
PneumoconiosesWorking with insulation, construction, demolition, building maintenance, automobiles
|
AsbestosisComplications=Increased risk of malignant mesothelioma and lung cancer; synergistic effect with tobacco
|
Labs=pleural biopsy show asbestos fibersRadiology= Multinodular opacities, pleural effusions, blurring of heart/diaphragm; chest CT shows linear pleural/parenchymal fibrosis
|
|
|
PneumoconiosesMining, pottery making, sandblasting, cutting granite
|
SilicosisComplications=Increase risk of TB infection; progressive fibrosis
|
Radiology=Small apical nodular opacities; hilar adenopathy
|
|
|
Pneumoconioses.Coal mining
|
Coal worker's diseaseComplications=Progressive fibrosis
|
Radiology=Small apical nodular opacities
|
|
|
PneumoconiosesElectronics, ceramics, tool, die manufacturing
|
BerylliosisComplications=Increased risk of lung cancer;
|
Labs=Pulmonary edema, diffuse granuloma formationRadiology=Diffuse infiltrates; hilar adenopathyTreatment=may need chronic corticosteroid treatment to maintain respiratory function
|
|
|
H/P = sudden dyspnea, pleuritic chest pain, cough, syncope, hemoptysis, feeling of impending doom; fever, tachypnea, tachycardia, cyanosis, loud S2, decreased breath sounds over regions of effusionLabs = increased A-a gradient; increased D-dimer; ABG shows increased CO2, decreased O2 (<80 mm Hg), ventilation-perfusion scan (V/Q scan) may show areas of mismatchECG = tachycardia, may show S wave in lead I and T-wave inversion in lead V3
|
Pulmonary embolism (PE)Occlusion of pulmonary vasculature by a dislodged thrombusIncreasing pulmonary artery pressure caused by occlusion leads to right-sided heart failure, hypoxia, and pulmonary infarctionRisk factors = 7 Hs: Heredity (genetic hypocoagulability), History (prior DVT or PE), Hypomobility (fracture, prolonged travel, surgery, obesity), Hypovolemia (dehydration), Hypercoagulability (cancer, smoking), Hormones (pregnancy, oral contraceptive pill [OCP] use), and Hyperhomocysteinemia.
|
Radiology = CXR may be normal or may show pleural effusion or wedge-shaped infarct; pulmonary angiography is diagnostic, but a higher risk study; spiral CT may detect proximal PE; ventilation-perfusion (V/Q) scan can detect areas of ventilation-perfusion mismatchA positive or negative V/Q scan is diagnostic or rules out PE, but an equivocal scan indicates need for angiographyTreatment = supplemental O2 to maximize saturation; IV fluids or cardiac pressors as needed for hypotension; anticoagulate initially with either low molecular weight heparin (LMWH) or unfractionated heparin (titrated for PTT 1.5–2.5 times normal); patients treated with unfractionated heparin need to be converted to either LMWH or warfarin (given to achieve goal international normalized ratio [INR] 2 -3) for 3–6 months; inferior vena cava filter can be placed if anticoagulation is contraindicated; thrombolysis may be considered for patients with massive PE or those with no cardiac contraindications, recent trauma, or surgery
|
|
|
H/P = dyspnea, fatigue, deep chest pain, cough, syncope, cyanosis; digital clubbing, loud S2, JVD, hepatomegalyLabs = increased red blood cell count (RBC) and WBCECG = right ventricular hypertrophyRadiology = CXR shows large pulmonary artery and large right ventricle; echocardiogram useful for measuring pulmonary artery pressure noninvasively and detecting valvular disease; cardiac catheterization is the gold standard test for measuring pressures, but carries greater risks than other studies; PFTs may be useful in diagnosing underlying pulmonary disease
|
Pulmonary hypertensionIncreased pulmonary artery pressure caused by PE, valvular disease, left-to-right shunts, COPD, or idiopathic causesIdiopathic pulmonary hypertension has a high mortality rate within a few years of diagnosis
|
Treatment = treat underlying condition; supplemental O2 helps maintain blood oxygenation; vasodilators indicated for idiopathic and pulmonary causes to decrease pulmonary vascular resistance; anticoagulants indicated in patients with idiopathic, embolic, or cardiac causes to decrease risk of pulmonary thrombus formation
|
|
|
H/P = orthopnea, paroxysmal nocturnal dyspnea, dyspnea; tachycardia, frothy sputum, wheezing, rhonchi, rales, dullness to percussion, peripheral edema, S3 or S4 heart sound, hypertensionLabs = increased brain natriuretic peptide (BNP) or abnormal cardiac enzymes help elucidate a cardiac causeECG = T-wave abnormalities or QT prolongation are common changes and can occur suddenly with acute onset
|
Pulmonary edemaIncreased fluid in lungs caused by increased pulmonary venous pressure and hydrostatic leak of fluid from vesselsCaused by left-sided heart failure, myocardial infarction (MI), valvular disease, arrhythmias, ARDS(pulmonary wedge pressure <18 mm Hg).A pulmonary wedge pressure measured with a Swan-Ganz catheter is suggestive of a cardiac cause for pulmonary edema if >18 mm Hg
|
Radiology = CXR shows fluid throughout lungs, cephalization of vessels (i.e., increased vascular markings in upper lung fields), Kerley B lines (i.e., prominent horizontal interstitial markings in lower lung fields)Treatment = treat underlying condition; diuretics, salt restriction, O2, morphine, vasodilators; nesiritide improves outcomes in cases with a cardiac cause; pressors may be required to improve cardiac output if perfusion is inadequate; Swan-Ganz catheter placement useful for monitoring response to therapy
|
|
|
H/P = possibly asymptomatic; dyspnea, pleuritic chest pain, weakness; decreased breath sounds, dullness to percussion, decreased tactile fremitus, egophonyRadiology = CXR shows blunting of costophrenic angles; decubitus CXR can demonstrate whether fluid is loculated or free flowing; CT is useful for measuring pleural thickness, distinguishing a discrete collection from a diffuse one (e.g., abscess vs. empyema)
|
Pleural effusionSerous or lymphatic fluid collection in pleural space is classified according to protein and lactate dehydrogenase (LDH) content and is caused by changes in hydrostatic and oncotic pressure (transudative), inflammation (exudative), or lymphatic duct rupture (lymphatic)1/4 of pleural effusions are associated with neoplasm
|
Labs = pleural fluid analysis used for protein and LDH levels (i.e., transudate vs. exudates), glucose (low in TB, malignancy, autoimmune diseases), pH (acidic in malignancy, TB, empyema), amylase (high in pancreatitis, esophageal rupture, some malignancies), triglycerides (high in thoracic duct rupture), complete blood cell count (CBC), Gram stain, and cytologyTreatment = treat underlying condition; relieve pressure on lung with thoracocentesis and chest tube placement; for cases with empyema (i.e., effusion of pus due to infection), a chest tube is required; if recurrent malignant effusion occurs, use pleurodesis (talc or other irritant) to scar the pleural layers together
|
|
|
Pleural effusionPleural: Serum Protein Ratio <0.5;Pleural: Serum LDH Ratio <0.6;Total Pleural Protein <3 g/dL
|
Transudateetiology=CHF, cirrhosis, kidney diseases (nephrotic syndrome)
|
|
|
|
Pleural effusionPleural: Serum Protein Ratio >0.5;Pleural: Serum LDH Ratio >0.6;Total Pleural Protein >3 g/dL
|
Exudateetiology=Infection, cancer, vasculitis
|
|
|
|
H/P = unilateral chest pain, dyspnea; decreased chest wall movement, unilateral decreased breath sounds, increased resonance to percussion, decreased tactile fremitus; respiratory distress, decreased Sao2, hypotension, JVD, or tracheal deviation suggest tension pneumothoraxRadiology = CXR shows lung retraction and mediastinal shift away from affected side; tension PTX will demonstrate tracheal deviation
|
Pneumothorax (PTX)Collection of air in pleural space that predisposes patient to pulmonary collapseCan occur spontaneously (less common) or secondary to trauma or a pulmonary medical condition (more common)
|
TreatmentSmall (<15% lung field) PTX may resolve with supplemental O2 onlyLarger (>15%) PTX requires chest tube placementOpen PTX with small wound is treated with chest tube and occlusive dressingOpen PTX with larger wounds should be treated with attempted closure and should carry a low threshold for intubationTension pneumothorax requires immediate needle decompression (4th or 5th intercostal space at the maxillary line) and chest tube placementRecurrent pneumothorax may require pleurodesis
|
|
|
H/P = dyspnea, pleuritic chest pain, weakness; decreased breath sounds, dullness to percussion, decreased tactile fremitus, egophonyLabs = thoracocentesis shows bloody effusion
|
HemothoraxCollection of blood in pleural space caused by trauma, malignancy, TB, or pulmonary infarctionComplications = thrombi formation, fibrosis can occur if blood is not drained from pleural space
|
Radiology = CXR resembles that for pleural effusion (i.e., lung retraction, mediastinal shift from affected side)Treatment = supplemental O2; chest tube placement; treat underlying cause
|
|
|
H/P = nonpleuritic chest pain, dyspnea; dullness to percussion over lung bases, palpable chest wall mass, scoliosis toward lesion
|
Malignant mesotheliomaUncommon tumor occurring on visceral pleura or pericardium with very poor prognosisIncreased incidence with asbestos exposure (occurs 20 years after exposure)
|
Labs = pleural biopsy is usually diagnostic; thoracocentesis of an associated pleural effusion can be used for cytology studiesRadiology = CXR shows pleural thickening, pleural effusion; chest CT can display extent of local disease; PET scan can be used to detect extrathoracic diseaseTreatment = extrapleural pneumonectomy with adjuvant chemotherapy and radiation therapy; chemotherapy alone used for unresectable disease
|
|
|
H/P = fatigue, daytime sleepiness, snoring, gasping or choking during sleep, morning headaches or confusion, impaired daytime function because of sleepiness; obesity common, anatomic abnormalities of palate or pharynx may be visibleLabs = Epworth sleepiness scale is useful for predicting likelihood of sleep apnea as cause for daytime somnolence (score >10 common in sleep apnea); polysomnography is definitive test that measures Apnea Index (AI, average apneic episodes per hour), Sao2, and number of arousals
|
Sleep apneaEpisodic cessation of airflow during sleep leading to desaturations and frequent arousalsTypesObstructive: obstruction of upper airway during sleep with continued respiratory effort; most often associated with obesity or abnormal pharyngeal anatomyCentral: loss of central respiratory drive leads to cessation of airflow and respiratory effortMixed: combines both obstructive and central characteristicsRisk factors = obesity, sedative use; males more than femalesEtiology is unknown, but may be linked to abnormal feedback control during sleep or decreased sensitivity of upper airway muscles to stimulation
|
TreatmentObstructive = consider weight loss (possibly bariatric surgery) and stop sedative use; continuous positive airway pressure (CPAP) is helpful in chronic cases to maintain airway patency; surgical correction of tonsillar hypertrophy, polyp removal, correction of congenital upper airway deformities, or tracheostomy may be necessary in severe or refractory casesCentral = respiratory stimulants; phrenic nerve pacemaking may be needed in severe casesBariatric surgery is associated with resolution of sleep apnea in 86% of cases.
|
|
|
H/P = asymptomatic if mild or slow development; pleuritic chest pain, dyspnea; fever, decreased breath sounds, dullness to percussion over affected areaRadiology = CXR will show fluffy infiltrates in mild cases and lobar collapse in cases of airway obstruction
|
AtelectasisLocalized alveolar collapse; common after surgery (especially abdominal) and anesthesia (generally not clinically serious); can also occur in asthmatics, after foreign body aspiration, or from mass effect (e.g., tumors, pulmonary lesions, or lymphadenopathy)If atelectasis lasts >72 hr, pneumonia is likely to develop.
|
Treatment = inspiratory spirometry, ambulation, and inpatient physical therapy are important for prevention in the hospital and postoperatively; severe cases require upper airway suctioning or bronchoscopy with deeper suctioning
|
|
|
Mechanical VentilationUse=General anesthesia, overdosePatient=No effort
|
Mode=Controlled mechanical ventilation (CMV)
|
Machine Determines and automatically delivers tidal volume (TV) and rate
|
|
|
Mechanical VentilationUse=Weaning patient from ventilatorPatient=Can breathe spontaneously between mechanical breaths
|
Mode=Intermittent mandatory ventilation (IMV)
|
Machine Determines and automatically delivers TV and rate
|
|
|
Mechanical VentilationUse=More comfortable for patient because of attempted synchronization; frequently used in place of IMVPatient=Can breathe spontaneously between mechanical breaths
|
Mode=Synchronized intermittent mandatory ventilation (SIMV)
|
Machine Machine tries to synchronize rate with patient-initiated breaths; automatically delivers TV and rate
|
|
|
Mechanical VentilationUse=Used when patient is more awake and in progressive weaningPatient driven unless no attempts to breathe (backup rate)
|
Mode=Assist-control ventilation (AC)
|
Machine senses patient's attempt to breathe and delivers full preset TV; backup rate if no spontaneous breaths
|
|
|
Mechanical VentilationUse=Used when patient relies less on ventilator; intubation not requiredPatient does all breathing
|
Mode=Continuous positive airway pressure (CPAP)
|
Machine maintains airway patency to decrease work of breathing
|
|
|
H/P = barking cough, inspiratory stridor, dyspnea, nasal congestion; fever, mild pharyngeal erythema, lymphadenopathy; respiratory distress in severe casesRadiology = neck radiographs may show subglottic narrowing of airway (i.e., steeple sign)
|
CroupAcute inflammation of larynx caused by parainfluenzae virus type 1; less commonly, by parainfluenzae virus types 2 and 3, respiratory syncytial virus (RSV) influenza virus, rubeola, adenovirus, or Mycoplasma pneumoniae3 Ss: Seal-bark cough, Subglottic swelling, and Stridor.
|
Treatment = supportive care (e.g., hydration, humidified air, rest, analgesia); aerosolized epinephrine and inhaled corticosteroids can be used in severe cases to decrease pharyngeal inflammation; with concerns for respiratory distress, the child should be admitted for observationIf child develops stridor at rest, hospitalization and respiratory monitoring is needed.
|
|
|
H/P = dysphagia, muffled voice, drooling, soft stridor, anxiety from symptoms; sudden high fever, inspiratory retractions; child may lean forward with hands on knees to aid breathing; erythematous and swollen epiglottisRadiology = neck radiographs show swollen opacified epiglottis that partially obstructs the airway (i.e., thumbprint sign); laryngoscope (only used in controlled situations) can visualize red and swollen epiglottis
|
EpiglottitisRapidly progressive infection of epiglottis and surrounding tissues that can cause airway obstructionMost common in children from 2–7 years of ageCaused by Haemophilus influenzae type B (Hib) infection; can also be caused by streptococcal or other H. influenzae bacteria
|
Labs = culture from swab of epiglottis can determine causative bacteria (should only be performed if patient intubated)Treatment = keep child calm; admit for close observation and respiratory monitoring; unless airway obstruction is mild, intubate (nasotracheal) to maintain airway patency; antibiotics for 7–10 days; airway obstruction preventing intubation requires emergent tracheostomyIn cases of suspected epiglottitis, examine the patient's throat only in a setting in which prompt intubation is possible because examination of the patient's throat can lead to additional throat irritation and resulting occlusion.
|
|
|
H/P = nasal congestion, cough, respiratory distress; wheezing, fever, tachypnea, crackles, prolonged expiration, hyperresonance to percussionRadiology = CXR shows hyperinflation of lungs and patchy infiltrates
|
BronchiolitisViral infection of bronchioles caused by RSV (most cases) or parainfluenzae virus type 3 (less common)Most commonly occurs in winter and spring; usually found in children <2 years of ageComplications = increased risk of developing asthma
|
Treatment = adequate hydration, humidified air, inhaled corticosteroids and β2-agonists; ribavirin can be used in severe cases to shorten disease course; children with respiratory distress or hypoxemia should be admitted for observation and respiratory monitoring
|
|
|
H/P = presentation within 2 days of birth; cyanosis, nasal flaring, expiratory grunting, intercostal retractions, respiratory rate >60 breaths/min, crackles, decreased breath soundsRadiology = CXR shows bilateral atelectasis with ground glass appearance and decreased lung volumes
|
Respiratory distress syndrome of the newbornPreterm infants (e.g., 24–37 wks' gestation and especially before 30 wks' gestation) have surfactant deficiency because of lung immaturity that leads to decreased lung compliance, atelectasis, and respiratory failureComplications = increased risk of developing asthma in childhood compared with other children
|
Labs = ABG shows increased CO2, decreased O2; amniotic fluid analysis (see Figure 2-9) not usually helpful, but may guide treatment between 34 and 37 wks' gestation by determining fetal lung maturity with the amniotic lecithin:sphingomyelin ratio (always treat for <34 weeks, treatment typically unnecessary for >37 weeks)Treatment = maternal administration of corticosteroids before initiation of labor helps to speed fetal lung maturation; neonatal intensive care unit (ICU) admission appropriate for close observation; supplemental O2 and surfactant replacement therapy mainstays of therapy; intubation should be performed for any neonate not responding to treatment or requiring high levels of O2 to maintain adequate Sao2
|
|
|
H/P = meconium stained-amniotic fluid seen during delivery; cyanosis, intercostal retractions; distended chest, tachypnea
|
Meconium aspiration syndromeAspiration of meconium (i.e., fetal stool passed into amniotic sac) predelivery causing obstruction of airways and pneumoniaComplications = pulmonary hypertension can develop if not promptly treated; increased risk of developing asthma during childhood
|
Labs = consider blood culture to rule out sepsisTreatment = suction nose, mouth, and upper airway at birth; supplemental O2; intubate for worsening respiratory distress; surfactant therapy may be useful for improving respiratory function; consider empiric antibiotic therapy if concerned for development of pneumonia
|
|
|
H/P = recurrent pulmonary infections (e.g., Pseudomonas, S. aureus), dyspnea, hemoptysis, chronic sinusitis, cough, meconium ileus at birth, steatorrhea, failure to thrive; cyanosis, digital clubbing, esophageal varices, rectal prolapseLabs = decreased serum Na; sweat test shows increased Na and increased Cl (>60 mEq/L in children, >80 in adults); genetic testing can locate mutation in CF transmembrane conductance regulator (CFTR) gene in suspected cases or in carriers of the gene considering pregnancy
|
Cystic fibrosis (CF)Autosomal recessive disorder caused by defect in chloride-pumping channel in exocrine glands; ducts of exocrine glands (e.g., lungs, pancreas, reproductive glands) become clogged with thick secretionsPresents in childhood and universally fatal, but proper treatment may allow survival into late 20s or early 30sAffects both pulmonary (recurrent infections, chronic sinusitis) and gastrointestinal systems (pancreatic enzyme deficiencies, malabsorption)Risk factors = whites at higher risk than other races
|
Treatment = deoxyribonuclease (DNase) aids in decreasing the viscosity of secretions; chest physical therapy helps to clear secretions; bronchodilators, non-steroidal anti-inflammatory drugs (NSAID), antibiotics for any suspected pulmonary exacerbation or infection; supplemental pancreatic enzymes and vitamins A, D, E, and K given for malabsorption
|
|
|
Tidal volume (TV)
|
Inspiratory volume during Normal respiratioN
|
|
|
|
Inspiratory reserve volume (IRV)
|
Air volume beyond normal tidal volume that is filled during maximal inspiration
|
|
|
|
Inspiratory capacity (IC)
|
Total inspiratory air volumE considering both tidal volume and inspiratory reserve volume (IC = TV + IRV)
|
|
|
|
Expiratory reserve volume (ERV)
|
Air volume beyond tidal volume that can be expired during normal respiration
|
|
|
|
Residual volume (RV)
|
Remaining air volume left in lung ollowing maximal expiration
|
|
|
|
Functional reserve capacity (FRC)
|
Air volume remaining in lungs after expiration of tidal volume (FRC = RV + ERV)
|
|
|
|
Functional vital capacity (FVC)
|
Maximal air volume that can be inspired and expired (FVC = IC + ERV)
|
|
|
|
Total lung capacity (TLC)
|
Total air volume of lungs (TLC = FVC + RV) |
|
|
|
Risk factors for DVT.
|
stasisendothelial injuryhypercoagulability (Virchow's triad)
|
|
|
|
Criteria for exudative effusion.
|
pleural/serum protein > 0.5pleural/serum LDH > 0.6
|
|
|
|
Causes of exudative effusion.
|
Think of leaky capillaries.MalignancyTBbacterial or viral infectionpulmonary embolism w/ infarctpancreatitis
|
|
|
|
Causes of transudative effusion.
|
Think of intact capillarie.CHFliver or kidney diseaseprotein-losing enteropathy
|
|
|
|
Nornalizing PCO2 in a patient having an asthma exacerbation may indicate?
|
Fatigue & impending respiratory failure
|
|
|
|
dypnealateral hilar lymphadenopathy on CXRnoncaseating granulomasincreased ACEhypercalcemia
|
Sarcoidosis
|
|
|
|
PFT showing decreased FEV1/FVC.
|
Obstructive pulmonary disease (e.g. asthma)
|
|
|
|
PFT showing increased FEV1/FVC.
|
Restrictive pulmonary disease
|
|
|
|
Honeycomb patten on CXR. Diagnosis?Treatment?
|
Diffuse interstitial pulmonary fibrosis.Supportive care.Steroids may help.
|
|
|
|
Treatment for SVC syndrome.
|
Radiation
|
|
|
|
Treatment for mild, persistent asthma.
|
Inhaled beta-agonists & inhaled corticosteroids
|
|
|
|
Acid-base disorder in pulmonary embolism.
|
Hypoxia & hypocarbia
|
|
|
|
Non-small cell lung cancer (NSCLC) associated with hypercalcemia.
|
Squamous cell carcinoma
|
|
|
|
Lung cancer associated w/ SIADH.
|
Small cell lung cancer (SCLC)
|
|
|
|
Lung cancer highly related to cigarette
|
Small cell lung cancer (SCLC)
|
|
|
|
A tall white male presents w/ acute shortness of breath. Diagnosis?Treatment?
|
Spontaneous pneumothorax.Spontaneous regression.Supplemental O2 may be helpful.
|
|
|
|
Treatment of tension pneumothorax.
|
Immediate needle thoracostomy
|
|
|
|
Characteristics favoring carcinoma in an isolated pulmonary nodule.
|
Age > 45-50 yrslesions new or larger in comparison to old filmsabsence of calcifcation or irregular calcificationsize > 2 cmirregular margins
|
|
|
|
Hypoxemia & pulmonary edema w/ normal pulmonary capillary wedge pressure.
|
ARDS
|
|
|
|
Increased risk of what infection w/ silicosis?
|
Mycobacterium tuberculosis
|
|
|
|
Causes of hypoxemia.
|
right-to-left shunt hypoventilation low inspired O2 tension diffusion defect V/Q mismatch |
|
|
|
Classic CXR findings for pulmonary edema |
cardiomegaly prominent pulmonary vesselsKerley B lines"bat's wing" appearance of hilar shadowsperivascular & peribronchial cuffing
|
|
|
|
_x0001_ SymptomsUnilateral, throbbing, visual and autonomic disturbances, nausea.Basilar migraine may present with ataxia, vertigo, dysarthria._x0001_ DiagnosisTypical symptoms in young adult, positive family history often, 75%of cases are women. Increased incidence of motion sickness and in-fantile colic.
|
Migraine_x0001_ Description• Classic migraine—unilateral throbbing headache with aura.• Common migraine—subtle onset, no aura, represents 80% of cases_x0001_ PathophysiologySerotonergic neurons in brain stem raphe involved. Vasomotorchanges. Spreading depression of Leao (neuronal depression). Cor-tical oligemia, extracranial vasodilation.
|
_x0001_ Treatment Steps1. Pharmacotherapy—acute headache: ergot alkaloids, serotonin(5-HT) agonists, prochlorperazine, metoclopramide.2. Preventive treatment: β-blockers, sodium valproate, topiramate,gabapentin, lamotrigine, methysergide (potential for retroperi-toneal fibrosis with long-term use), calcium channel blockers, an-tidepressants, nonsteroidal anti-inflammatory drugs (NSAIDs),cyproheptadine.3. Avoid alcohol, tyramine (cheese), chocolate, citrus, onions, andnitrite.
|
|
|
_x0001_ SymptomsSevere pain in short episodes without aura, for weeks to months,then remits, ipsilateral lacrimation, nasal congestion, conjunctivalinjection, nasal congestion, dilated superficial temporal artery._x0001_ DiagnosisTypical symptoms, men more often (95%), worse with alcohol andsleep.
|
Cluster Headache_x0001_ DescriptionVascular headache, also known as histamine cephalalgia, Horton’sheadache, migrainous neuralgia.
|
_x0001_ Treatment Steps1. Pharmacotherapy—acute headache: ergot alkaloids, serotonin(5-HT) agonists, prochlorperazine, metoclopramide.2. Preventive treatment: β-blockers, sodium valproate, topiramate,gabapentin, lamotrigine, methysergide (potential for retroperi-toneal fibrosis with long-term use), calcium channel blockers, an-tidepressants, nonsteroidal anti-inflammatory drugs (NSAIDs),cyproheptadine.3. Avoid alcohol, tyramine (cheese), chocolate, citrus, onions, andnitrite.2. Also prednisone, oxygen, lithium.
|
|
|
_x0001_ SymptomsTemporal headache, focal tenderness superficial temporal/occipitalarteries, vision loss, malaise. Can be associated with polymyalgiarheumatica._x0001_ DiagnosisClinical suspicion, elevated erythrocyte sedimentation rate (ESR),biopsy of temporal artery.patientover age 50 (but oftenmuch older) whopresents with unilateralheadache in temporalregion, or eye pain
|
Temporal Arteritis (Giant Cell)_x0001_ DescriptionInflammatory systemic illness in elderly. Medical emergency._x0001_ PathologyMononuclear cell and giant-cell infiltrates in cranial arteries. Skip le-sions.
|
_x0001_ Treatment StepsCorticosteroids Treatment with steroidsmust be startedimmediately to preventloss of vision.• Surgical biopsy isdefinitive for diagnosis,and although startingsteroids empirically mayalter biopsy results, it isoften done to preventblindness.
|
|
|
_x0001_ SymptomsThose of increased intracranial pressure without tumor, headache,visual disturbances, nausea, vomiting, dizziness._x0001_ DiagnosisClinical seting (headache, papilledema, no focal neurologic find-ings, obese female). Magnetic resonance imaging (MRI) more sensi-tive to look for hydrocephalus, rule out tumor or dural sinus veinthrombosis. Lumbar puncture shows elevated opening pressure.
|
Benign Intracranial Hypertension(Pseudotumor Cerebri)_x0001_ PathologyDecreased cerebrospinal fluid outflow conductance.
|
_x0001_ Treatment Steps1. Acetazolamide, diuretics.2. Prednisone.3. Serial lumbar punctures.4. Optic nerve sheath incision, lumboperitoneal shunts.
|
|
|
_x0001_ SymptomsBrief episodes of pain in fifth cranial nerve distribution, third andsecond divisions_x0001_ DiagnosisOnset after 40, more often in women, may coexist with multiple scle-rosis (MS); history is diagnostic, may have facial trigger points butno sensory impairment.
|
Trigeminal Neuralgia (Tic Douloureux)_x0001_ PathologyDegenerative changes gasserian ganglion. Compression of trigemi-nal nerve by vascular loops causing demyelination. MS; demyelina-tion of root entry zone.
|
_x0001_ Treatment Steps1. Phenytoin, carbamazepine, baclofen, gabapentin, amitriptyline,lamotrigine.2. Alcohol nerve block.3. Microvascular decompression.4. Percutaneous radiofrequency nerve thermocoagulation.
|
|
|
Impending loss of consciousness secondary to inadequate cerebralperfusion.
|
Syncope and PresyncopeEtiology vascular or cardiac, not neurologic. May be due to hyperventilation, orthostatic hypotension, vasovagal, micturition
|
|
|
|
Disorder of balance system, dizziness when standing and walking,
|
Dysequilibriummultiple possible central nervous system (CNS) causes. Chronic andcommon in elderly.
|
|
|
|
Sensation of movement, due to abnormality of the peripheral orcentral vestibular system pathways. Nystagmus may be present. Pe-ripheral nystagmus is unidirectional and suppressed by fixation.Central nystagmus may be multidirectional and is never suppressedby fixation.
|
Vertigodisorders resulting in vertigoinclude vestibular neuronitis, labyrinthitis, posttraumatic brain stemtransient ischemic attack (TIA), MS, posterior fossa tumor, and basi-lar artery migraine
|
|
|
|
hearing loss, tinnitus, and vertigo.
|
Ménière’s disease
|
|
|
|
vertigo aggravated by change in head position, sneezing, noises
|
Perilymph fistulaoval window tear resulting
|
|
|
|
premonitory phase followed by immediate lossof consciousness, tonic, clonic, and postictal (confusion) phases.Electroencephalogram (EEG) hallmark is immediate bihemisphericdischarges
|
Tonic and/or clonicGeneralized Epileptic Seizures
|
|
|
|
brief loss of consciousness (5–10 seconds), sud-den blank stare, abrupt cessation of activity; clonic movements, au-tomatisms such as lip smacking. EEG three per second spike-and-wave pattern.
|
Absence seizuresGeneralized Epileptic Seizures
|
Drug of choice: ethosuximide.
|
|
|
sudden generalized or focal muscle jerk, EEG dischargeconcurrent with jerk
|
MyoclonicGeneralized Epileptic Seizures
|
|
|
|
1 to 2 sec. Drop attacks limited or generalized, .
|
Atonic seizuresGeneralized Epileptic Seizuressecondary to diffuse brain disease
|
|
|
|
infantile spasms (sudden extensor/flexor trunk movements) psychomotor retardation and EEG hyparrhythmia (disorganized high-voltage slow waves, spikes, and sharp waves)
|
West syndromeGeneralized Epileptic Seizurespre- & postnatal causes including genetic disorders, injuries, infections,metabolic disorders.
|
Adrenocorticotropic hormone (ACTH), valproic acid or clonazepam
|
|
|
less abrupt onset, longer, loss of postural tone, as-sociated with other seizure types; EEG background abnormal, ictal0.5- to 2.5-Hz spike-and-wave discharges.
|
Atypical absenceGeneralized Epileptic Seizures
|
|
|
|
no impairment of consciousness.start in one motor cortical area—may spread with progressive jerking (jacksonian seizures)
|
Simple partial sezures, Motor
|
|
|
|
no impairment of consciousness.tingling, numbness, sensation of movement or absenceof body part.
|
Simple partial sezures, Sensory, Parietal
|
|
|
|
no impairment of consciousness.flashes of light, hemianopsia, scotomata. Visual associa-tion cortex, complex images—micropsia, macropsia, distortions.
|
Simple partial sezures, Sensory, Occipital
|
|
|
|
no impairment of consciousness.auditory, olfactory hallucinations, emotional or psy-chic phenomena, memory or cognitive distortions (déjà vu),time distortions, detachment, affective (fear, depression)
|
Simple partial sezures, Sensory, Temporal
|
|
|
|
impaired level of awareness and con-sciousness, amnesia for event, automatisms may occur.
|
Complex partial seizuresFocal Epilepsy
|
|
|
|
a. Benign childhood epilepsy with centrotemporal spikes; stops inadolescence—somatosensory, tonic/tonic–clonic activity involv-ing face to arm, generalized with nocturnal seizures.b. Childhood epilepsy with occipital paroxysms (spikes)—visualseizures while awake, motor seizures during sleep.
|
Partial epileptic syndromesFocal Epilepsy
|
|
|
|
weakness in a part of the body after a seizure
|
Todd’s postictal paralysisreflects a partial seizurehaving taken place
|
|
|
|
Continued or recurrent seizures of any type with unconsciousnessfor 20 or more minutes
|
Status Epilepticus
|
Treat as medical emergency, intravenous(IV) lorazepam (binds γ-aminobutyric acid [GABA]A receptor) followed by IV phenytoin
|
|
|
quadriplegia and lower cranial nerve paralysis, but conscious with higher mental activity intact.
|
Locked-in syndrome
|
|
|
|
Patient cannot be aroused, total unresponsivenesmay demonstrate response to noxious stimuli
|
COMA_x0001_ PathologyDiffuse cerebral hemisphere dysfunction and/or involvement of thebrain stem ascending reticular activating system.• Trauma. History of injury. Epidural hematoma: lucid interval. Sub-dural: depressed consciousness, then focal findings.• Vascular disease. Sudden onset, nuchal rigidity, bloody cerebrospinal fluid (CSF).• Neoplasm. Focal signs, papilledema.• Infection. Cerebrospinal fluid increased protein normal or low CSFglucose.• Metabolic. Abnormal labs.
|
_x0001_ Treatment Steps1. Establish airway, and IV line.2. Determine cardiovascular status, history, and physical.3. Obtain full lab, skull x-ray, computed tomography (CT), and/orMRI.4. May need lumbar puncture.5. Give thiamine, dextrose, and possibly naloxone.6. If cerebral edema or increased intracranial pressure, restrict fluids,hyperventilate, mannitol, and steroids.
|
|
|
patient in coma, but appears awake
|
Akinetic mutism (coma vigile)
|
|
|
|
coma (lesion localization)hyperpnea alternating with apnea
|
Cheyne–Stokes respirationbilateral cerebral hemisphere damage
|
|
|
|
coma (lesion localization)long inspiration then pauseorataxic (chaotic) breathing
|
Apneustic respiration or ataxic (chaotic) breathinglower pontine lesions
|
|
|
|
coma (lesion localization)extension/adduction of armsand legs
|
Decerebrate posture. Midbrain lesion
|
|
|
|
coma (lesion localization)flexion arms, wrists, and fingers
|
Decorticate posture. Lower diencephalon lesion
|
|
|
|
sudden onset of a focal neurologic deficit due to cerebrovas-cular disease, lasting more than 24 hours.
|
StrokeTo identify cause of stroke, the following tests are usually completed:• Carotid ultrasound.• Echocardiogram (transesophageal echocardiogram done incertain settings).• Fasting lipid panel.• Hypercoagulability workup may be indicated in certaincases, particularly young individuals with no other source of stroke
|
|
|
|
focal, abrupt in onset, usually lasts less than 1 hour; resolvewithin 24 hours
|
TIAGreatest risk for stroke in days to weeks.
|
|
|
|
stroke or TIA (origin)abrupt onset while activePatients rarely lose consciousness
|
Cerebral Embolismmost commonsource of embolism is the heart; less common peripheral arterialembolization.
|
|
|
|
stroke or TIA (origin)abrupt onset while activemay lose consciousness
|
Subarachnoid Hemorrhageaneurysm at circle of Willi
|
|
|
|
stroke or TIA (origin)abrupt onset while activemay lose consciousness; CT positive for hematoma
|
Intraparenchymatous Hemorrhage
|
|
|
|
stroke or TIA (origin)10% preceded by TIA, often during sleep; rarely loseconsciousness.May have normal CT and lumbar puncture early;rarely have headache
|
Thrombotic
|
|
|
|
Ischemic Stroke (artery?)contralateral hemiplegia/paresis. Domi-nant hemisphere—nonfluent or Broca’s aphasia from upper-divisionocclusion.Wernicke’s (fluent) aphasia from lower-division lesions.
|
Middle cerebral artery
|
|
|
|
Ischemic Stroke (artery?)contralateral leg paralysis, abulia, aki-netic mutism, sphincter incontinence
|
Anterior cerebral artery
|
|
|
|
Ischemic Stroke (artery?)contralateral weakness or sensory loss, speechdisturbance, ipsilateral visual loss
|
Carotid artery
|
|
|
|
Ischemic Stroke (artery?)contralateral homonymous hemianopia, cortical blindness, prosopagnosia, alexia without agraphia.
|
Posterior cerebral
|
|
|
|
Ischemic Stroke (artery?)ataxia, hemiplegia, horizontal gaze, palsy, nystagmus vertigo, deafness, dizziness
|
Vertebrobasilar
|
|
|
|
Ischemic Stroke (artery?)ataxia, dizziness, nausea, vomiting
|
Cerebellar
|
|
|
|
Ischemic Stroke (artery?)pure motor or sensory strokes, clumsy hand syndrome may be seen
|
Lacunar infarct—due to lipohyalinosis
|
|
|
|
Ischemic Stroke
|
_x0001_ Risk Factors• Nonmodifiable—race, age, gender, family history prior TIA orcerebrovascular accident (CVA).• Modifiable—hypertension, diabetes mellitus, smoking, alcoholabuse, oral contraceptives, cardiac disease, prior stroke, lipoproteinabnormalities, elevated homocysteine and C-reactive protein, coag-ulopathies.
|
_x0001_ Treatment Steps1. Prevention—treat modifiable risk factors (above).2. TIA—antiplatelet aggregating drugs (aspirin, ticlopidine, clopi-dogrel).3. Acute ischemic infarction—protect airway, prevent aspiration,avoid aggressive blood pressure (BP) control. Treat BP slowly ifover 170/100 mm Hg. Treat hyperglycemia, reduce fever. Throm-bolysis in infarcts less than 3 hours old with tissue plasminogenactivator. Cerebral edema peaks in 2 to 7 days; treat with modestfluid restriction, intubation and hyperventilation, mannitol.4. Elective carotid endarterectomy if carotid stenosis present.
|
|
|
headache, vomiting, decreasedlevel of consciousnessStroke (cause)
|
Hypertensive intracerebral hemorrhage
|
|
|
|
Hypertensive intracerebral hemorrhage (location?)Unusual eye signs
|
thalamic hemorrhage
|
|
|
|
Hypertensive intracerebral hemorrhage (location?) pin-point reactive pupils, coma, quadriplegia, ophthalmoplegia, decerebrate posturing
|
Pontine hemorrhage
|
|
|
|
Hypertensive intracerebral hemorrhage (location?)vertigo,headache, vomiting, and ataxia.
|
Cerebellar bleed
|
|
|
|
Hypertensive intracerebral hemorrhage (location?)hydrocephalus
|
Ventricular extension associated with poor prognosis.
|
|
|
|
Sudden severe headache, meningeal irrita-tion; exam may be normal
|
Subarachnoid hemorrhage—caused by saccular aneurysm or vascular malformation
|
|
|
|
Hemorrhagic Stroke (work up/treatment?)Other causes of bleeding include arteriovenous malformation, tu-mor, anticoagulant therapy, cocaine abuse, cerebral amyloid an-giopathy, angiitis
|
Initial test of choice—CT scan. Do lumbar puncture only if CT not available, and check for papilledema before doing lumbar puncture.
|
_x0001_ Treatment Steps1. Control BP.2. Treat seizures.3. Control raised intracranial pressure (ICP).4. Surgery in selected cases—ventriculostomy to decrease ICP andremove blood, hemorrhage removal in some instances (cerebellum, putamen, lobar).
|
|
|
_x0001_ SymptomsOptic neuritis, vertigo, paresthesias, sensory loss, pain, incoordination,bladder dysfunction, nystagmus, weakness in 50%, trigeminal neural-gia, diplopia, internuclear ophthalmoplegia, characteristically bilateral.
|
Multiple Sclerosis_x0001_ DescriptionMultiple areas of neurologic deficits, peak age 20 to 24. Increased in-cidence in women and north temperate latitudes, etiology unknown,possibly autoimmune. Fewer exacerbations during pregnancyDIAGNOSIS OF MS• Signs and symptomstypical of the disease areneeded and must bepresent at two differentpoints in time.• Testing will help confirmthe diagnosis.• Demyelinating plaquesseen on MRI ofbrain/spinal cord.• CSF often revealsoligoclonal bands.• Increased latency invisual evoked response(VER), brain stemauditory evokedresponse (BAER), orsomatosensory evokedpotential (SSEP)
|
_x0001_ Treatment Steps1. Acute exacerbations: Intravenous or oral steroids.2. Prophylaxis: Interferon-β (Avonex, Betaseron, Rebif), interferon-α (Intron A), or glatiramer acetate (Copaxone).3. Symptomatic treatment: Spasticity—Lioresal, Tizanidine, Dantrium;bladder—oxybutinin, hyoscyamine, antiseptics (vitamin C, meth-enamine); pain—carbamazepine, gabapentin, amitriptyline, lam-otrigine.
|
|
|
Papillitis, swelling of the optic nerve head may occur. May cause acute visual lossDecreased visual acuity and color vision, scotomata, ocular pain. Ab-normal VER, visual fields, and contrast sensitivity.
|
Optic Neuritis_x0001_ DescriptionInflammation of the optic nerve, often from optic nerve demyelination. Episode of optic neuritis may precede MS. _x0001_ DiagnosisMRI may demonstrate T2-weighted and gadolinium-enhancing lesions of optic nerve.Brain or spinal cord MRI abnormalities—greater risk of MS with twoor more
|
_x0001_ Treatment StepsIntravenous methylprednisolone (Solu-Medrol). Interferon-β prohylaxis with 2 or more MRI lesions.
|
|
|
_x0001_ SymptomsHeadache, stiff neck, confusion, seizures, fever, coma. Focal andmultifocal signs. Mortality 10–30%.postinfectious and postvaccinal
|
Acute Disseminated Encephalomyelitis_x0001_ DescriptionMonophasic, mostly postinfectious and postvaccinal
|
_x0001_ Treatment StepsCorticosteroids.
|
|
|
_x0001_ SymptomsProgressive ascending weakness, areflexiaFrequently preceded by upper respiratory or gastroin-testinal (GI) infection (Campylobacter jejuni), surgery, immunization.Linked to Epstein–Barr virus (EBV), cytomegalovirus (CMV), human immunodeficiency virus (HIV)._x0001_ DiagnosisHigh CSF protein, with few cells, short duration of progression;nerve conduction studies. With HIV infection, CSF pleocytosis isfound.
|
Guillain–Barré Syndrome—A PeripheralNeuropathy_x0001_ DescriptionAcute inflammatory polyradiculoneuropathy in young to middle-aged adults. _x0001_ PathologyEndoneurial perivascular mononuclear cell infiltration; multifocal root and nerve demyelination
|
_x0001_ Treatment StepsSpontaneous recovery may occur, plasmapheresis, or intravenous im-munoglobulin.
|
|
|
_x0001_ SymptomsHeadache, fever, stiff neck. Minimal neurologic signs in viral menin-gitis, which is a benign self-limited disorder and also termed asepticmeningitis. Positive Kernig’s and Brudzinski’s signs.
|
Acute Meningitis_x0001_ DiagnosisGram stain and culture of CSF. CSF protein over 50, viral; in bacte-rial or fungal up to 400. Hypoglycorrhachia (CSF glucose less than40% of serum level) suggests bacterial cause. Tuberculous (charac-teristically lymphocytic meningitis) active pulmonary disease in onethird, positive purified protein derivative (PPD) in 50%_x0001_ Pathology1. Neonatal—group B streptococcus, Escherichia coli.2. Early childhood—Haemophilus influenzae, Streptococcus pneumoniae,and Neisseria meningitidis.3. Young adults—Neisseria meningitidis (petechial or ecchymotic rashoften), S. pneumoniae, H. influenzae.4. Nosocomial—Gram-negative bacteria and Staphylococcus aureus.5. Immunosuppressed—Listeria monocytogenes, S. pneumoniae, H. in-fluenzae, Nocardia, Mycobacterium tuberculosis, Cryptococcus neofor-mans.6. HIV patients—acute aseptic meningitis.7. Viral meningitis—most common agent is mumps; enterovirus ismost common viral group.
|
_x0001_ Treatment Steps1. Toxoplasma—pyrimethamine plus sulfadiazine.2. Brucella—tetracycline and aminoglycoside. Chronic neurobrucel-losis––rifampin, trimethoprim–sulfamethoxazole, doxycycline.3. Neonatal—ampicillin and gentamicin.4. Adults—ceftriaxone or ampicillin.5. Tuberculous—isoniazid, ethambutol, rifampin, pyrazinamide.6. Fungal—amphotericin B.• Newer studies havesuggesteddexamethasone may beuseful in acute bacterialmeningitis if given beforeor with first dose ofantibiotics.• Prophylaxis (rifampin orciprofloxacin) is given toclose contacts ofpatients with meningitisdue to N. meningitidis,rifampin, or ciprofloxacin
|
|
|
_x0001_ SymptomsTabes dorsalis, general paresis, gumma, optic atrophy, cerebrovascu-lar disease from invasion of leptomeninges with Treponema pallidum.Neurosyphilis most often is asymptomatic.
|
Neurosyphilis
|
_x0001_ Treatment StepsHigh-dose parenteral penicillin
|
|
|
hypotension, fever, headache, chills, and tachycardia in first 24 hours of treatment of neurosyphilis
|
Jarisch–Herxheimer reactionrelease of treponemal products; not a penicillinreaction
|
|
|
|
Infection spread from paranasal sinuses and middle earmarked peripheral leukocytosis.
|
Empyema (Subdural)treptococcusmost often
|
|
|
|
_x0001_ SymptomsFocal signs and acute febrile illness, seizures and coma, or depressed state of consciousness. Headache, fever, and nuchal rigidity._x0001_ DiagnosisAseptic CSF, lymphocytic CSF with normal glucose
|
Viral Encephalitis_x0001_ DescriptionMortality of 10%_x0001_ PathologyCaused by mumps, herpes simplex type 1, lymphocytic choriomenin-gitis, arboviruses, EBV. Mouse and hamster exposure linked to lymphocytic choriomeningitis
|
_x0001_ Treatment StepsTreat edema and seizures
|
|
|
respiratory spasms, dysphagia–hydrophobia
|
Rabies—brain stem encephalitis, incubation 30 to 60 days or more fatal in acute stage in95%
|
|
|
|
an acute febrile illness w/ evidence of lower motorneuron paralysis
|
Polio—etiology: enteroviruses that damage anterior horn cells of spinal cord
|
|
|
|
most common opportunisticCNS pathogen in acquired immune deficiency syndrome (AIDS)
|
Toxoplasmosis—intracellular parasite
|
|
|
|
Ataxia and myoclonus, dementia
|
Creutzfeldt–Jakob, kuru
|
|
|
|
Elevated gamma globulin and measles antibodies in CSF
|
Subacute sclerosing panencephalitis
|
|
|
|
Due to SV40-PML
|
Progressive multifocal leukoencephalopathy (PML)
|
|
|
|
temporal lobe localizationCNS infection
|
Herpes simplex encephalitis
|
treat with acyclovir
|
|
|
progressive muscle weaknessand atrophydiagnosis by family history, weakness, muscle biopsy,probable death by age 20. Elevated creatine kinase (CK).
|
Duchennedue to mutation on X chromosome (dystrophin gene;Xp21 locus)
|
|
|
|
NEUROMUSCULAR DISEASEautosomal recessive and dominant forms
|
Limb–girdle
|
|
|
|
thinning face muscles, electromyogram (EMG) shows adecremental pattern, and irregular after potentials. Autosomal domi-nant (chromosome 19q. Expanded CTG repeats in myotonin pro-tein kinase
|
Myotonic
|
Treat with phenytoin sodium (Dilantin).
|
|
|
NEUROMUSCULAR DISEASEFascioscapulohumeral
|
autosomal dominant. No carriers
|
|
|
|
_x0001_ SymptomsWeak with activity, fatigue, ocular symptoms; facial muscles, voice,limb muscles, and respiration can be affected._x0001_ DiagnosisTensilon test, electromyogram—repetitive nerve stimulation, posi-tive antibodies to acetylcholine receptor.
|
Myasthenia Gravis_x0001_ DescriptionAutoantibodies against acetylcholine receptor. Associated withthymic hyperplasia and thymoma. Women more than men
|
_x0001_ Treatment Steps1. Cholinesterase inhibitors.2. Steroids.3. Plasmapheresis.4. Thymectomy.Thymectomy may offer acure to patients withmyasthenia gravis (MG).Thymectomy is offered toall patients with a thymomaand patients aged 10–55without a thymoma butwith generalized MG5. Immunosuppressants, IV immunoglobulin
|
|
|
_x0001_ SymptomsLimb weakness without cranial muscle weakness and absence ofdeep tendon reflexes. Found with small cell lung cancer or as autoimmune disease._x0001_ DiagnosisResponse to repetitive stimulation (increasing action potential)
|
Eaton–Lambert Syndrome_x0001_ DescriptionFacilitating neuromuscular transmission disorder due to autoanti-bodies against presynaptic neuromuscular voltage-gated calciumchannels
|
_x0001_ Treatment Steps Guanidine. Calcium channel antagonists are contraindicated.
|
|
|
_x0001_ SymptomsBegin 12–36 hours after ingestion of exotoxin in contaminatedfood. Blurred vision, dilated fixed pupil, flaccid quadriplegia, dysphagia, dysarthria, respiratory paralysis, dry mouth.
|
Botulism_x0001_ DescriptionToxin of Clostridium botulinum blocks acetylcholine release._x0001_ DiagnosisIsolate toxin from stool, stomach, or food. Spores also found inhoney. EMG—decreased compound muscle action potentials; post-tetanic facilitation
|
_x0001_ Treatment Steps1. Cathartics.2. Trivalent antitoxin (A, B, E).3. Quinidine.4. Supportive therapy.
|
|
|
predominantly distal weakness, cardiacconduction problems, cataracts, testicular atrophy, endocrine dys-function, increased sensitivity to medications which depress respiratory drive, ptosis, temporalis and masseter muscle wasting.
|
Myotonic dystrophy
|
|
|
|
Impaired muscle relaxation
|
Myotonia congenita
|
treat with phenytoin
|
|
|
eosinophilia, weakness, myalgiaundercooked pork mostcommon source
|
Trichinosis_x0001_ DescriptionNematode Trichinella spiralis infection,
|
_x0001_ Treatment StepsThiabendazole, mebendazole.
|
|
|
_x0001_ Symptoms/DiagnosiMuscle spasms, trismus (lockjaw), facial muscle spasm (risus sardon-icus), opisthotonos, autonomic dysfunction. Clinical diagnosis
|
etanus_x0001_ DescriptionLockjaw, intense motor neuron activity._x0001_ PathologyCaused by neurotoxin (tetanospasmin) from Clostridium tetani, agram-positive coccus, which inhibits spinal inhibitory interneurons.
|
_x0001_ Treatment Steps1. Cleaning and debridement of infected site.2. Antibiotics.3. Antitoxin (human hyperimmune globulin).4. Skeletal muscle relaxants (diazepam).
|
|
|
_x0001_ SymptomsIdiopathic, acute, peripheral facial weakness; may have ipsilateralhyperacusis and decreased taste._x0001_ DiagnosisInexcitable facial nerve, denervation of facial muscles after 2–3weeks.
|
Bell’s Palsy
|
_x0001_ Treatment StepsSupportive treatment Artificial tears to prevent corneal drying. Of-ten self-limited. If patients present early, steroids and/or antiviral medications may be helpful.
|
|
|
middle-age rapid progressionof weakness. Combination of upper (spasticity, hyperreflexia, emo-tional lability) and lower (atrophy, weakness, cramps, fasciculations)neuron involvement. Bulbar and respiratory weakness in 50%
|
Amyotrophic lateral sclerosis (ALS)Familial ALS has mutation forsuperoxide dysmutase gene
|
Treated with riluzole
|
|
|
floppy infant, delayed milestones, progressive atrophy, respiratoryand swallowing problems
|
Type 1 proximal spinal muscular atrophy (Werdnig–Hoffmann)Autosomal recessive, deletions in neu-ronal apoptosis inhibitory gene in two-thirds.
|
|
|
|
Weakness,onset age 20–40, muscle cramps, gynecomastia, dysphagia, dysarthria
|
Bulbospinal muscular atrophy (Kennedy’s disease)X-linked recessive, increased CAG repeats in androgen receptor gene
|
|
|
|
_x0001_ SymptomsProgressive emotional or intellectual decline associated with chorea,abnormalities in gait, ocular motor function, and dexterity. Onset in fourth or fifth decades in most. Patients live an average of 15 years after diagnosis.
|
Huntington’s Disease_x0001_ DescriptionChorea, personality change, psychiatric syndromes, progressive de-mentia. Autosomal dominant with expanded CAG repeat sequence in huntingtin gene._x0001_ DiagnosisExam, family history._x0001_ PathologyCaudate nucleus and cerebral cortex atrophy, neuronal loss andgliosis, and decreased GABA and acetylcholine have been noted along with spared somatostatin–neuropeptide Y neurons.
|
_x0001_ Treatment StepsNo cure but dopaminergic antagonists: presynaptic—tetrabenazine,reserpine; postsynaptic—haloperidol (Haldol).
|
|
|
_x0001_ SymptomsNeurologic—tremor, incoordination, ataxia, akinesia, dysarthria,dysphagia, dystonia.Hepatic—hepatitis, which may be acute or chronic; cirrhosis.Ocular—Kayser–Fleischer ring in Descemet’s membrane of corneanoted (rusty brown ring at limbus).Psychiatric—variable presentation._x0001_ DiagnosisHigh serum copper and high urine copper. Slit lamp exam, lowserum ceruloplasmin, and elevated 24-hour urine copper; liverbiopsy and copper quantitation are also helpful. Abnormal liverfunction tests. Aminoaciduria. MRI—cerebral atrophy, putaminal,thalamic, and brain stem hypodensities. Pathology––excess copperdeposits in liver and brain.
|
Wilson’s Disease (Hepatolenticular Degeneration)_x0001_ DescriptionChromosome 13 autosomal recessive disorder of copper metabolism(mutations in copper-transporting P-type ATPase), characterized bydeficient ceruloplasmin, elevated urinary copper excretion. Presentsin adolescence or early adulthood
|
_x0001_ Treatment StepsD-penicillamine. Adverse effects of therapy include hypersensitivity,fever, nephrotic syndrome, myasthenia gravis, Goodpasture syn-drome, bone marrow suppression (agranulocytosis and thrombocy-topenia), and collagen vascular disorders.
|
|
|
_x0001_ SymptomsCharacterized by resting tremor (pill-rolling—5–7 Hz), cogwheelrigidity, bradykinesia, impaired postural reflexes, masked facies, flexed posture, hypophonia._x0001_ DiagnosisClinical exam. Reduced 6-[18F]-fluorolevodopa in striata withpositron-emission tomography (PET)
|
Parkinson’s Disease_x0001_ DescriptionAn idiopathic extrapyramidal movement disorder affecting the el-derly. Reduced activity complex I mitochondrial electron transportchain. Mutation in α-synuclein gene in familial Parkinson’s disease_x0001_ PathologyDepigmentation, neuronal loss and gliosis in substantia nigra andpigmented nuclei. Cytoplasmic inclusion (Lewy) bodies. Results inreduced striatal dopamine. Associated decreased activity complex I mitochondrial electron transport chain.
|
_x0001_ Treatment Steps1. Levodopa/carbidopa (Sinemet), toxicity with levodopa: dyskine-sias, hallucinations, confusion.2. Anticholinergics, amantadine.3. Dopamine agonists (bromocriptine, pergolide, pramipexole,ropinirole) particularly late.4. Catechol-O-methyltransferase (COMT) inhibitors prolong L-dopa availability.5. Pallidotomy and deep brain stimulation for end-stage disease
|
|
|
methylphenyltetrahydropyridine (MPTP); neuroleptics block striatal dopamine receptor sitesIatrogenic Dyskinesias
|
Drug-induced parkinsonism
|
|
|
|
linguofasciobuccal, choreiformIatrogenic Dyskinesias
|
Tardive dyskinesia
|
|
|
|
levodopaIatrogenic Dyskinesias
|
Dopamine agonist-induced chorea
|
|
|
|
inappropriate cocontraction of antagonistic muscles, re-sulting in repetitive twisting movements.
|
Dystonia
|
Focal dystonias treated withbotulinum toxin injection: generalized with trihexiphenidyl (Ar-tane)
|
|
|
random twitching or jerking, excessive, involuntary, pur-poseless movements
|
Chorea
|
|
|
|
oromandibular dystonia
|
Blepharospasm(Meige syndrome)
|
|
|
|
most frequent focal dystonia, involving neckmuscles. Intermittent or sustained head deviation
|
Spasmodic torticollis
|
|
|
|
distal upper extremity, postural or action tremor; is of-ten progressive. May be familial (autosomal dominant with variablepenetrance)
|
Tremor (Essential)
|
Treatment includes propranolol, primidone, topira-mate. Alcohol responsive
|
|
|
Rapid jerking movement
|
Myoclonus
|
treat primary cause when known. Clonazepam, 5-hydroxytryptophan (5-HTP) and valproic acid often used
|
|
|
Sudden loss of postural toneClassically described as a “flap.” Patient has arms outstretched, palms out, but cannot keep hands still.
|
AsterixisOccurs in metabolic encephalopathies(uremic, hepatic), drug intoxications, and structural brain lesions.
|
|
|
|
_x0001_ SymptomsMemory loss, language and visuospatial impairments, mood distur-bance, delusions, hallucinations, changes in personality and behav-ior. Generalized seizures (10–20%).
|
Alzheimer’s Disease_x0001_ DescriptionA progressive dementia (global cognitive decline) of middle and late life._x0001_ DiagnosisNo one test is diagnostic. It is a clinical diagnosis/diagnosis of exclu-sion. Clinical, abnormal mental status exam and exclusion of otherillnesses (e.g., normal pressure, hydrocephalus, metabolic disease,multi-infarct dementia, tumor, and infections). Etiology is unknown,but frequency increases with age. Familial associations with amyloidprecursor protein and presenilin protein mutations; inheritance ofE4 allele apolipoprotein E. MRI demonstrates cortical atrophy. Sin-gle photon-emission computed tomography (SPECT), PET scanshave bilateral temporoparietal hypometabolism._x0001_ PathologySenile plaques (dystrophic neurites surrounding an amyloid core)and neurofibrillary tangles are prominent, associated with cerebral atrophy and ventricular dilatation.
|
_x0001_ Treatment StepsSymptoms such as agitation and depression are treatable. Acetyl-cholinesterase inhibitors (tacrine, donepezil, rivastigmine, galantamine). Newer medications include memantine (Namenda).
|
|
|
_x0001_ SymptomsProminent, early personality change, apathy, abulia, disordered speech, aphasia.
|
Pick’s Disease_x0001_ DescriptionDementia with lobar atrophy._x0001_ DiagnosisOccasionally familial. CT/MRI—prominent symmetric/asymmetricfrontotemporal atrophy_x0001_ PathologyFrontotemporal lobar atrophy. Argyrophilic neuronal (Pick) inclu-sion bodies in frontal and temporal lobes. Frontal and temporal at-rophy sparing superior temporal gyrus.
|
_x0001_ Treatment StepsSupportive treatment for dementia.
|
|
|
_x0001_ SymptomsDementia. Clinical features determined by location1)(location?)psychomotor slowing, decreased atten-tion, concentration and memory deficits, gait disorder (lower half parkinsonism)2)(location?) aphasia, apraxia, visuospatial defects, amnesia_x0001_ DiagnosisProgressive intellectual decline. Associated stroke risk factors andmultiple infarctions, ventricular dilatation. Multifocal decreases incerebral blood flow on PET/SPECT.
|
Multi-infarct Dementia_x0001_ DescriptionEpisodic neurologic dysfunction secondary to infarcts of the cere-bral hemispheres leading to dementia.1)=subcortical 2)=cortical
|
_x0001_ Treatment Steps1. Aspirin, ticlopidine, clopidogrel.2. Treat hypertension.
|
|
|
_x0001_ SymptomsUrinary incontinence, dementia, gait disturbance (slow, short steps;unstable)._x0001_ DiagnosisNormal CSF pressure. Enlarged cerebral ventricles, relatively normalcortical gyri on CT/MRI. Subependymal CSF resorption on MRI.
|
Hydrocephalus (Normal Pressure)_x0001_ DescriptionProgressive dementia usually occurring in the elderly_x0001_ PathologyIncreased resistance to arachnoid villus absorption of CSF. Associ-ated with subarachnoid hemorrhage, trauma, tumor, infection.
|
_x0001_ Treatment StepsVentriculoperitoneal shunt. Significant improvement w/ CSF removal.
|
|
|
_x0001_ SymptomsSubacute progressive dementia, myoclonus._x0001_ DiagnosisClinical, EEG high-voltage, triphasic periodic complexes on depressed background.
|
Creutzfeldt–Jakob Disease_x0001_ DescriptionProgressive dementia, due to abnormal isoform of prion protein(PrPSc). Disease may be infectious, inherited, or sporadic._x0001_ PathologySpongiform change (vacuolar dilatation of neurons), amyloidplaques, loss of neurons, and gliosis.
|
_x0001_ Treatment StepsNone.
|
|
|
_x0001_ SymptomsPtosis, miosis, anhidrosis, enophthalmos, narrowing palpebral fis-sure, flushing on affected side of face
|
Horner Syndrome_x0001_ PathologyInterruption of the unilateral sympathetic system due to trauma,lung apex tumor, CNS lesions, vascular headache._x0001_ DiagnosisCocaine and para-OH-amphetamine tests
|
|
|
|
_x0001_ SymptomsUnilaterally dilated pupil with slow response to light and accommo-dation; areflexia may be present.
|
Adie’s Pupil_x0001_ PathologyPostganglionic parasympathetic lesion._x0001_ DiagnosisWeak pilocarpine solution results in Adie’s pupil contraction
|
|
|
|
_x0001_ SymptomsVery small pupils that fail to constrict to light with accommodationpreserved. One or both eyes affected
|
Argyll–Robertson Pupil_x0001_ DiagnosisArgyll–Robertson pupil is a sign of neurosyphilis. Rule out CNS structural lesions
|
|
|
|
_x0001_ SymptomsPupils fixed and dilated, ophthalmoplegia and contralateral hemi-paresis
|
Uncal Herniation Syndrome
|
|
|
|
_x0001_ SymptomsDefective direct light reflex with intact consensual reflex on “swing-ing flashlight test.”
|
Marcus Gunn Pupil
|
|
|
|
_x0001_ SymptomsEye “down and out.”
|
Third Cranial Nerve LesionAffects medial rectus, superior rectus, inferior rectus, inferioroblique, and levator of eyelid.
|
|
|
|
_x0001_ Symptomsvertical diplopia.
|
Fourth Cranial Nerve LesionSuperior oblique muscle affected;
|
|
|
|
_x0001_ SymptomsWeak lateral rectus, poor abduction
|
Sixth Cranial Nerve Lesion
|
|
|
|
Unreactive, Midposition Pupil (lesion localization)
|
Midbrain lesion
|
|
|
|
Pinpoint Pupils
|
Pontine lesion
|
|
|
|
Unilaterally Dilated and Unreactive Pupil
|
Possible third nerve lesion
|
|
|
|
—Daytime sleep attacks accompanied by cataplexy,hypnogogic hallucinations, and sleep paralysis. Rapid onset REMsleep.
|
Narcolepsy
|
Treat with amphetamine, pemoline, methylphenidate,dextroamphetamine. Clomipramine for cataplexy.
|
|
|
—Arousal from NREM sleep
|
Night Terror
|
|
|
|
—Awakening from REM sleep
|
Nightmare
|
|
|
|
Gliomas typemost common of all gliomas, and most commonbrain tumor in childhood
|
Astrocytoma
|
|
|
|
Gliomas typeusually frontal lobe, slow growing, presentswith headache, seizures, and the tumor may bleed.
|
Oligodendroglioma
|
|
|
|
most common posterior fossa tumor in chil-dren. Fast growing, radiosensitive
|
Medulloblastoma
|
|
|
|
Gliomas typeInfratentorial morethan supratentorial and filum terminale
|
Ependymomaependymal surface location
|
|
|
|
CNS neoplasm typeUsually benign, associated with type 2 neurofibromatosis
|
Meningiomas
|
|
|
|
CNS neoplasm typeSuprasellar, visual field defects often (bitemporal hemianopsia), en-docrinopathies, diabetes insipidus.
|
Craniopharyngiomas
|
|
|
|
CNS neoplasm typeEndocrine and visual symp-toms
|
Pituitary TumorsSecretory in 75%, nonsecretory in 25%
|
|
|
|
CNS neoplasm typeUnilateral hearing loss, tinnitus
|
Acoustic SchwannomaMay compress cranial nerves V, VII,and brain stem. Bilateral in neurofibromatosis type 2
|
|
|
|
_x0001_ SymptomsLucid interval after brief unconsciousness followed by increasingobtundation. Sometimes no lucid interval present. Extremeheadache, contralateral hemiparesis
|
Epidural Hematoma_x0001_ DiagnosisHistory and physical, CT scan.
|
_x0001_ Treatment Steps1. Neurosurgical evaluation for possible drainage.2. Empiric anticonvulsants.3. May use mannitol to control intracranial pressure/swelling
|
|
|
Acute, subacute, and chronic from cortical vein tear.Acute—From high speed trauma, coma from impact; CT useful(see Fig. 11–2).Subacute—Several days of lethargy, then deterioration; MRI.Chronic—Minor trauma may cause gradual deterioration; MRI.
|
Subdural Hematoma
|
|
|
|
_x0001_ SymptomsSudden-onset severe headache, may have sentinel bleed with minorsymptoms. May have stiff neck, photophobia, nausea, and focal signs
|
Subarachnoid Hemorrhage
|
_x0001_ Treatment Steps1. Supportive care.2. Bed rest, analgesics.3. Prophylactic anticonvulsants.4. Carefully control blood pressure.
|
|
|
_x0001_ SymptomsHigh fever, muscular rigidity, akinesia, decreased consciousness, au-tonomic dysfunction all as a complication of major tranquilizers, tri-cyclic antidepressants, or withdrawal from dopaminergic agents.
|
Neuroleptic Malignant Syndrome (NMS)
|
_x0001_ Treatment Steps1. Withdraw neuroleptics.2. Bromocriptine or dantrolene.3. Supportive care.
|
|
|
_x0001_ SymptomsAcute respiratory failure in a patient with myasthenia gravis.
|
Myasthenic Crisis
|
_x0001_ Treatment Steps1. Discontinue cholinesterase (ChE) inhibitors.2. Ventilate patient in intensive care unit (ICU).3. Slowly reintroduce ChE inhibitors.
|
|
|
_x0001_ SymptomsDepression of level of consciousness with myoclonus, asterixis,tremor, seizures. EEG abnormal; may have triphasic waves.
|
Uremic Encephalopathy
|
Treat renal disease.
|
|
|
_x0001_ SymptomsConfusion, lethargy, headache, seizures. The more rapid the sodium drop, the more severe the symptoms.
|
Hyponatremia
|
Syndrome of inappropriate an-tidiuretic hormone (SIADH): treat with water restriction; demeclocycline if chronic.
|
|
|
_x0001_ SymptomsAbdominal pain, vomiting, constipation or diarrhea, confusion, seizures, neuropathy._x0001_ DiagnosisWatson–Schwartz test for elevated aminolevulinic acid
|
Acute Intermittent Porphyria_x0001_ PathologyDeficiency of porphobilinogen deaminase
|
_x0001_ Treatment Steps1. Hematin and high-carbohydrate diet.2. Carbamazepine for seizures.
|
|
|
_x0001_ SymptomsAcute exposure—abdominal colic, headache, behavioral change, en-cephalopathy, seizures. Chronic exposure—gastrointestinal distur-bances, anemia, weight loss, behavioral disturbances, cognitive impairment. Peripheral neuropathy (wrist drop) in adults.
|
Lead Toxicity_x0001_ DiagnosisBasophilic stippling, lead line on x-ray. Lead colic is most frequentsign in adults. Screen with lead level, ethylenediaminetetraaceticacid (EDTA) test if lead level not over 80._x0001_ PathologyNeuropathy from segmental demyelination.
|
_x0001_ Treatment StepsChelation with Ca-EDTA or penicillamine.
|
|
|
_x0001_ SymptomsAsterixis, slow EEG, depressed mental status, elevated blood ammo-nia.
|
Liver Disease—Hepatic Encephalopathy
|
Give protein-free diet, neomycin, or lactulose.
|
|
|
_x0001_ SymptomsNausea, vomiting, abdominal pain, renal failure, neuropathy, encephalopathy._x0001_ DiagnosisHistory, exam, Mees’ lines (transverse lines in nails).
|
Arsenic Toxicity
|
_x0001_ Treatment StepsUse dimercaprol (BAL) or penicillamine.
|
|
|
—Wernicke’s encephalopathy, nystagmus,ataxia, confusion, amnesia
|
Thiamine (B1) deficiency
|
|
|
|
—Pernicious anemia, megaloblastic ane-mia, subacute combined spinal cord degeneration
|
Cobalamin (B12) deficiency
|
|
|
|
—Excess can produce sensory neuropathy
|
Pyridoxine (B6)
|
|
|
|
_x0001_ SymptomsTinnitus, hearing loss, delirium, coma, seizures
|
Salicylate Toxicity_x0001_ DiagnosisHistory, respiratory alkalosis, serum salicylate level, rapid screen: ferric chloride test
|
_x0001_ Treatment Steps1. Treat shock.2. Protect airway.3. Routine drug intoxication measures.
|
|
|
_x0001_ SymptomsVomiting, lethargy, and delirium due to brain edema after a viral ill-ness that was treated with aspirin, with abnormal liver functions, hy-poglycemia, and respiratory alkalosisLiver shows microvesicularfatty infiltration
|
Reye’s Syndrome
|
|
|
|
_x0001_ SymptomsType I—visceromegaly. Type II/III—gaze palsies, trismus, spasticity,dementia, seizures, and visceromegaly.
|
Gaucher’s Disease_x0001_ DescriptionGlucocerebroside lipidosis._x0001_ DiagnosisClinical. Bone marrow may contain Gaucher cells (lipid-ladenmacrophages). Enzymatic analysis._x0001_ PathologyDeficiency of lysosomal glucocerebrosidase. Autosomal recessive.
|
|
|
|
_x0001_ SymptomsPolyneuropathy with neuralgia, cerebrovascular disease in middleage, vasculopathy with renal and cardiac disease, cutaneous angio-keratoma and telangectasias.
|
Fabry’s Disease_x0001_ DescriptionSphingolipidosis. Inborn error of metabolism._x0001_ DiagnosisClinical exam. Enzymatic analysis._x0001_ PathologyDeficiency of lysosomal α-galactosidase A. Sex-linked recessive. Gly-cosphingolipid deposition in tissues (eyes, kidney, heart, CNS).
|
Treatment StepsCarbamazepine, phenytoin for pain. Renal transplantation.
|
|
|
_x0001_ SymptomsProgressive dementia and visual impairment, irritability, muscleweakness, spasticity, seizures._x0001_ DiagnosisCherry-red spot in the fovea. Abnormal electroretinogram (ERG) and visual evoked potential (VEP).
|
Tay–Sachs Disease_x0001_ DescriptionInfantile cerebromacular degeneration caused by mutations of α-subunit of the lysosomal β-hexosaminidase A gene._x0001_ PathologyAccumulation of gangliosides in retina and CNS neurons. Autosomal recessive
|
|
|
|
_x0001_ SymptomsPain, fatigue, and stiffness on exertion._x0001_ DiagnosisForearm exercise test—low/absent lactate production. Elevatedmuscle glycogen on biopsy.
|
McArdle’s Disease_x0001_ DescriptionA glycogen-storage disorder due to a mutation in the myophosphorylase gene._x0001_ PathologyDeficient muscle phosphorylase
|
_x0001_ Treatment StepsGlucose and reduce exercise.
|
|
|
Progressive weakness,hypotonia, heart failure
|
Pompe’s DiseaseAcid α-glycosidase (acid maltase) deficiency
|
|
|
|
Episodic Muscle Weakness, low potassium
|
Episodic Muscle WeaknessFamilial hypokalemic periodic paralysis—autosomal dominant,due to mutation of DHP-sensitive calcium channel
|
|
|
|
Episodic Muscle Weakness, elevated potassium.
|
Familial hyperkalemic periodic paralysis—autosomal dominant(mutation of the human muscle sodium channel), shorter weakness attacks
|
|
|
|
Obesity, mental retardation, retinitis pigmentosa, hypogonadism,polydactyly, diabetes insipidus, autosomal recessive
|
Laurence–Moon–Biedl Syndromelooney,moon,blind
|
|
|
|
Multisystem atrophy with orthostatic hypotension and CNS degeneration (parkinsonism; cerebellar, pyramidal features)
|
Shy–Drager SyndromeNeuronal loss intermediolateral cell column
|
|
|
|
Most common spinocerebellar degeneration onset childhood. Mutation in GAA repeat frataxin (X25) gene
|
Friedreich’s Ataxia
|
|
|
|
Demyelinating polyneuropathy, slowly progressive, peroneal muscleatrophyMutation in peripheral myelin protein-22 gene.
|
Charcot–Marie–Tooth Disease
|
|
|
|
Café au lait spots (more than six of 1.5-cm size), neurofibromas, schwannomas, optic nerve gliomas,Lisch nodules iris.
|
Neurofibromatosis 1mutation in NF-1 neurofibromin gene
|
|
|
|
Bilateral vestibular schwannomas, menin-giomas, astrocytomas, posterior lens opacities
|
Neurofibromatosis 2mutation in NF-2(MERLIN protein) gene.
|
|
|
|
mental retardation, epilepsy, cutaneous faciallesions, and organ hamartomasAutosomal dominant
|
Tuberous Sclerosis
|
|
|
|
Autosomal disorder with retinal and cerebral hemangioblastomas;renal, pancreatic, and epididymal cysts; and renal carcinomas
|
von Hippel–Lindau Disease
|
|
|
|
Progressive cerebellar ataxia (Purkinje cell degeneration), oculocu-taneous telangiectasia, radiosensitivity, immunodeficiency and lym-phoid malignancies.
|
Ataxia–TelangiectasiaDue to mutated ATM gene with phosphoinositol-3′kinase activity
|
|
|
|
_x0001_ DescriptionStatic encephalopathy with abnormal motor function from birth.Antepartum events cause 90%; also associated with prematurity andlow birth weight.
|
Cerebral Palsy_x0001_ DiagnosisHistory and physical examination, skull x-ray, CT/MRI of the head,EEG, and psychological testing, evaluation of developmental mile-stones._x0001_ PathologyIncludes periventricular leukomalacia, periventricular/intraventric-ular hemorrhages, infarction
|
_x0001_ Treatment Steps1. Multidisciplinary support.2. Orthopedic intervention.3. Physical/occupational therapy.4. Control seizures.5. Social services.
|
|
|
Cerebral Palsyassociated with prematurity. Either periventricularleukomalacia or periventricular hemorrhage (greater involvement of intellectual function)
|
Spastic diplegia
|
|
|
|
Cerebral Palsyassociated with congenital malformations & intrauterine infections. Severe disability associated with mental retardation and seizures (Lennox–Gastaut syndrome)
|
Spastic quadriplegia
|
|
|
|
Cerebral Palsycaused by developmental malformations, stroke, trauma. Seizures associated
|
Spastic hemiplegia
|
|
|
|
Cerebral Palsybilirubin encephalopathy (rare) and causes of spasticquadriplegia
|
Athetosis
|
|
|
|
_x0001_ Symptomsshort seizure without focal features_x0001_ DescriptionSeizure in child age 3 months to 5 years, associated with fever/infection
|
Febrile Seizures_x0001_ DiagnosisHistory and physical exam; rule out meningitis, septicemia. Hospitaladmission, including routine lab, lumbar tap._x0001_ PathologyUnknown.
|
_x0001_ Treatment Steps1. Temperature reduction (tub bath, acetaminophen [Tylenol]).2. Medication (diazepam [Valium] 0.2 mg/kg rectally or IV).
|
|
|
_x0001_ SymptomsAsymptomatic, or may demonstrate pain, red eye, and vision loss.May note halos around lights.
|
Glaucoma_x0001_ DescriptionOphthalmic disorder of elevated intraocular pressure, which is etiology of 10% of blindness in the United States._x0001_ DiagnosisOn exam, elevated intraocular pressure (over 22 mm Hg by Schiøtz’tonometry)_x0001_ PathologyTypes include primary angle-closure, open-angle, secondary, andcongenital. May be of sudden obstructive (primary angle-closure) etiology, or chronic obstruction (open-angle).
|
|
|
|
eye pain, vomiting, visionloss, sudden onset
|
Primary angle-closure GLAUCOMA
|
_x0001_ Treatment StepsPrimary Angle-Closure—Surgical iridectomy, with acetazo-lamide (Diamox) and β-blockers preop.
|
|
|
vision field defects, disccupping, no pain!
|
Primary open-angle GLAUCOMA
|
_x0001_ Treatment StepsPrimary Open-Angle—Treatment includes topical (eyedrops):• β-Blockers––Timoptic (timolol).• Carbonic anhydrase inhibitors––Trusopt(clorzolamide), Diamox(acetazolamide).
|
|
|
_x0001_ SymptomsNarrowed visual field; larger blind spot, vision may be normal or im-paired._x0001_ DiagnosisFundoscopic exam (disc swollen, associated hemorrhages/exu-dates).
|
Papilledema_x0001_ DescriptionElevation/swelling of optic nerve head.Papilledema may cause optic atrophy._x0001_ PathologySecondary to elevated CSF pressure, and a result of infection, opticneuritis, metabolic disease, CNS lesions.
|
_x0001_ Treatment StepsTreat primary cause.
|
|
|
_x0001_ Symptoms/DiagnosisProgressive painless visual loss, or asymptomatic. Diagnose via oph-thalmoscopic examination._x0001_ DescriptionLens opacity (nuclear, cortical, and subcapsular).
|
Cataract_x0001_ PathologyAge related; ultraviolet light exposure association, and may also relate to trauma, corticosteroids, and diabetes.
|
_x0001_ Treatment StepsCataract removal and intraocular lens implantation.
|
|
|
light flashes in eye
|
Retinal detachmentretinal degeneration ortrauma induced
|
|
|
|
Constricted pupil differential
|
iritis, drugs, Horner’s
|
|
|
|
Dilated pupil differential
|
Adie’s, glaucoma, drugs, third nerve lesion.
|
|
|
|
thickened conjunctiva
|
Pinguecula
|
|
|
|
thickened conjunctiva encroaching on cornea
|
Pterygium
|
|
|
|
small pupil, ciliary injection
|
Iritis
|
treat with cycloplegics andsteroids
|
|
|
large pupil, diffuse injection
|
glaucoma
|
treat with pilocarpine, acetazolamide [Diamox], etc.
|
|
|
eye anterior chamber blood
|
Hyphema—trauma induced
|
|
|
|
blocked meibomian gland duct
|
Chalazion |
|
|
|
Sudden vision loss
|
rule out artery (secondary to emboli, retinawhite) or vein occlusion.
|
|
|
|
xanthomas and hepatomegaly?
|
- primary biliary sclerosis- other sx: pruritis- lab: increased alk phos, cholesterol, IgM- associated with Sjogrens, Raynauds, scleroderma, autoimmune hypoTH, celiac, increased malignancy- tx: ursodeoxycholic acid, only def tx = liver transplant
|
|
|
|
- anti-smooth muscles- anti-smith- pANCA
|
- acute and chronic hepatitis- SLE (sensitive but only 30-50%)- Churg-Strauss, micrscopic polyangitis
|
|
|
|
pt with hep C?
|
- all pts should receive vaccine for hep A, B including during pregnancy
|
|
|
|
pregnant pt with HCV?
|
- OK to breast feed, vaginal delivery, sex without barrier protection if in stable relationship
|
|
|
|
cholecdochal cyst
|
- congenital abnormality of biliary ducts => dilation of intra/extra hepatic biliary ducts- infants: juandice, acholic stools; kids - abd pain, jaundice, recurrent pancreatitis; adults: vague pain, cholangitis- US -> CT -> MRI- can become choriocarcinoma
|
|
|
|
baby with jaundice, acholic stools?
|
- biliary atresia, choledocal cyst
|
|
|
|
carolis syndrome
|
- congenital d/o, intrahepatic dilation of bile ducts
|
|
|
|
pancreatic pseudocyst occurs where?
|
- as retroperitoneal mass
|
|
|
|
ddx peritoneal fluid
|
- portal HTN, trauma, infx, pancreatitis, malignancy- to ddx need to know exudate vs transudate => calculate SSAG = ascites albumin - serum albumin => if >1.1 = transudative = portal HTN
|
|
|
|
signs of decreased liver synthetic fx?
|
- decreased serum albumin, increased INR
|
|
|
|
what PEX is not associated with hyperaldo?
|
- will see decreased Na but should not see EDEMA (b/c then something else)
|
|
|
|
pt with newly dx cirrhosis?
|
- do screening endoscopy to eval esoph varices => if + give beta blocker
|
|
|
|
octreotide
|
- used for tx hepatorenal syndrome
|
|
|
|
unconjugated hyperbili
|
- unconjugated bili > 90% of T bili- estimate Hg and periph smear to check for hemolysis
|
|
|
|
pt with chronic hep C but normal LFTs x 1 yr
|
- no tx needed
|
|
|
|
when to check for hep B and C in pts with hx of blood transfusion?
|
- hep B: prior to 1986- hep C: prior to July 1992
|
|
|
|
when to check HCV?
|
- IV drug, blood transfusion/transplant prior July 1992, HD, chronically elevated ALT, children born to HCV mom
|
|
|
|
when to check HBV?
|
- hyperendemic areas (AFrica, SE asia, ME, Amazon, Haiti, Dominican Republic), male + male, IVDA, dialysis, HIV+, pregnant, contacts of HBV pts
|
|
|
|
liver toxins?
|
- dose dependent direct liver toxins: carbon tetrachloride, acetaminophen, tetracycline, amonita phalloides- idiosyncratic rxn: isoniazide, chlorpromazine, halothane, antiretrovirial
|
|
|
|
drug induced liver dz?
|
- cholestasis: chlorpromazine, nitrofurantoin, erythromycine, anabolic steroids- fatty liver: tetracycline, valproate, anti-retrovirals- hepatitis: halothane, phenytoin, isoniazide, alpha-methyldopa- toxic/fulminant liver dz: carbon tetrachloride, acetaminophen- granulomatous: allopurinol, phenylbutazone
|
|
|
|
labs on alcoholic hep?
|
- AST:ALT >2
|
|
|
|
biopsy of hepatitis?
|
- panlobular mononuclear infiltratio nwith hepatic cell necrosis- if negative serology then consider drug induced
|
|
|
|
OCP on liver?
|
- abnormal LFTs but no change in biopsy
|
|
|
|
dx of autoimmune hep?
|
- consider once r/o all possible causes of drug or viral- see +ANA, smooth muscle ab
|
|
|
|
wilson's dz?
|
aka hepatolenticulo degeneration- sx <30y.o., cirrhosis, neuropsych sx (parkinson, mood), kayser fleischer rings- decreased creuloplasmic => decreased Cu excretion => deposits in lier, basal ganglia, cornea- associated with Fanconi's dynrome, hemolytic anemia, neuropathy- dx: liver biopsy => hepatic Cu level > 250mcg/gram dry weight, or low ceruloplasmi + high urinary Cu excretion or K-F rings
|
|
|
|
hemochromatosis
|
- abnormally high iron abosroption => liver disease, pigmentation, DM, impotence, arthropathy
|
|
|
|
gallbladder Ca
|
- RF: southwest native american, mex-america, chronic gb inflammation, hx gallstones, porcelain gallbladder, salmonella typhi, anatomic variation- very rare
|
|
|
|
pregnant +HBV
|
- if active can tranmit to baby via placenta or during delivery esp if dvlped during 3rd trimester- + HBsAG, HBeAg, IgM, anti-HBcAb- if HBeAg negative then risk decreases from 95% to 20%- baby's risk of chronic hepB = 90%, thus give passive immunization with HBIG and active HBV vaccine
|
|
|
|
Pancreatic RF
|
- smoking, chornic pancreatitis, fhx, DM, obesity, hgih fat diet- ALCOHOL is not RF
|
|
|
|
pt with severely elevated AST, ALT, mild change in PT, albuin
|
- hepatocellular pattern injury most likely 2/2 med; e.g. pt with headahces => most likely using acetaminophen though don't say in stem- it increased PT and low albmin, think cirrhosis
|
|
|
|
pt with pancreatitis sx?
|
- do U/S, most likely 2/2 gallstones- don't do CT- only do CT when tx doesn't work
|
|
|
|
sx of chronic liver dz?
|
- weight loss, gynec, test atrophy, impotence 2/2 hyperE (low SHBG)
|
|
|
|
pt with cirrhosis now with asterixis, confusion, reversal sleep cycle?
|
- hepatic encephalopathy 2/2 increase ammonia in blood b/c can't detox to urea- increased sensitivity to GABA, false NT production- precipitating factors: increased protein diet, alkalosis, diuretic therapy, high volume paracentesis, portocaval shunts- not caused by increased urea!
|
|
|
|
chronic HBV infx?
|
- HBsAg for > 6 months - do livery biopsy to assess hepatic injury- if liver damage = chronic active, if no liver damage = chronic persistance
|
|
|
|
post cholecystectomy pain?
|
- sphincter of oddi dysfx:- sx: RUQ pain, increased LFTs during attack; do oddi manometry, see increased pressure; tx: sphincterotomy- dx of exclusion = functional pain
|
|
|
|
edema in cirrhosis?
|
- 2/2 decreased protein => indecreased intravascular oncotic pressure
|
|
|
|
types of gallstones
|
1. cholesterol, 2. pigment (calcium bilirubate) 3. mixed- 80% = cholesterol and mixed = radiolucent
|
|
|
|
pregnant and cholecystitis?
|
- repeated attacks =? cholecystecty in 2nd trimester- else give ursodeoxcholic acid to dissolve stones that will return once stop tx
|
|
|
|
travel, RUQ pain, dysentary, single cyst in right lobe liever
|
- AMEBIC livery cyst, histolyticia, cyst aspiraition = sterile, acellular, anchovy paste- usually invades colon => bloody diarrhea- tx: metronidazole
|
|
|
|
dx liver cyst
|
- amebic cyst- pyogenic liver bascess: severe presentaiton, 2nd to surgery, GI infx, acute appendicitis, tx broad spectrum abx = ceftriaxone- hydatid cyst - echinococcus granulose = dog contact- cystic ca= thick ,irregular, hpervascular wall, numerous septate
|
|
|
|
acalulous cholecystis
|
- GB inflammation without gallsontes, 2/2 extensive burns, trauma, prlonged TPN, fasting, mechanical ventilation
|
|
|
|
tx of gallstone pancreatitis?
|
- tx pancreatitis, then do cholecystitis
|
|
|
|
signs of met to liver?
|
- suggestion of GI malignancy (+occult blood), anemia 2/2 GI leed, firm hepatomegaly, increased alk phos more than increase in ast, alt = ca infiltration rather than liver injury- pleural effusion of L; note if on Rthen may be 2/2 hdrothorax = cirrhosis
|
|
|
|
post op cholestasis
|
- after major surgery 2/2 hypotension, blood loss into tissues, blood transfusion- increased pigment load from transufion, decrased liver function, decreased renal bilirubin excretion- high bili, alk phos
|
|
|
|
halothane
|
- anesthetic causes hepatotox, not used anymore
|
|
|
|
increased risk of alcohol liver injury?
|
- women > men
|
|
|
|
non-alcoholic fatty liver dz?
|
- associated with obesity, DM II- path: insulin resistance => increased at in liver => increased lipolysis => increased insulin levels- dx: biopsy- note: decreased glycogen synthesis in liver in DM II, but increased glucagon
|
|
|
|
increase in alk phos?
|
- check GGT- if high = liver- if low = other like bone
|
|
|
|
pt with mildly elevated LFTs on routine exam?
|
repeat in 6 months, if again increased then = chronic and do viral, hemochromatosis, fatty liver testing- if those are negative then test for muscle d/o polymyositis, thyroid dz
|
|
|
|
most important test of liver fx?
|
- PT! b/c all clotting factors synthesized by liver- don't interpret LFTs b/c can go down 2/2 recovery or fewer hepatocytes
|
|
|
|
left sided pleural effusion
|
pancreatitis, maligancy
|
|
|
|
dx of alpha 1 antitrypsin?
|
measure alpha one in serum => then confirm with genetic testing- testing is indicated in all premature chronic bronchitis, emphysema, dyspnea, non-smokers with COPD- tx: purified A1AT- test relative of homozygouses
|
|
|
|
mallory bodies
|
alcoholic hepatitis but is not diagnositic and not used for dx
|
|
|
|
vanishing bile duct syndrome
|
primary biliary cirrhosis, not primary sclerosing cholangitis
|
|
|
|
hbv tx
|
indications: persistance increased alt, detectable serum hbsag, hbv dna- alt is most important predictor of response to tx; BEST is 2x normal- tx: alpha interferon or lamivudine
|
|
|
|
hep A vs hep B vs hep C
|
- hep A: flu like, jaundice, dark urine, dirty place, other people with same sx- hep b, sx 1-6 mo s/o infx- acute hep C: asympt
|
|
|
|
serologic makers of hbv?
|
- hbsAg = 1st serologic marker, always dectable as long as infected- window period = period between hbsag undetected and anti-hbs undetected-anti-hbc= second serologic marker, makes IgM and IgG, IgM is present during window period- HbeAg = viral replication and infectivity, if >3mo then increased risk chronic
|
|
|
|
+bilirubin in dipstick?
|
- hyperbili 2/2 conjugated bili and not unconjugated (not water soluble)
|
|
|
|
rotor syndrome
|
- benign defect of hepatic storage of conjugated bili => leak into plasma, normal LFTs
|
|
|
|
hep C tx
|
indications: natural hx of dz, stage, liver biopsy, lfts, + hcv rna- if mild, tx is interferon- if medium e.g. increased alt, hcv rna+, chronic hep = tx with interferon and ribavirin (lamivudine is for hepb)
|
|
|
|
anaphylaxis to blood transufsions?
|
IgA deficiency
|
|
|
|
gilbert dz?
|
- decreased udp glucuronl tranferase => unconjugated hyperbili
|
|
|
|
crigler-najjar type i
|
- jaundice, neuro impairment, kernicterus (bilirubin enceph), increased indirect bili, normal LFTs- tx Liver tx, meanwhile light therapy
|
|
|
|
Crigler-Najjar type 2 |
- milder, survive into adulthood, no kernicterus- tx phenobarbital as needed
|
|
|
|
complications of pancreatitis?
|
1. hypovolemic shock: inflammatory factors => increased vascular permeability => fluid in retroperitoneum => need several L of fluid2. LV failure 2/2 vascular volume loss3. cardiac tamponade4. pseudocyst, asympt unless rupture, hemorrhage or infx5. retroperitoneal hemorrhage => see flank or umbilical ecchymoses
|
|
|
|
tx PBC?
|
- ursodeoxycholic acid, slows dz progression, reduces sx- if advanced then tx is liver transplant (eg. cirrhosis, liver damage)- 7-10 yr survival after 1st sx- symptomatic tx = cholestyramine for itching relief
|
|
|
|
intrahepatic cholestasis of pregnancy? vs normal physiologic changes? PBL?
|
- cholestatsis: 2nd, 3rd trimester => increased bile acid 2/2 genetic or hormone; see increased ALT, AST, alk phos, serum bile; must r/o viral hepatitis; dx of exclusion; tx: ursodeoxycholine, cholestyramine not as effective and SE- normal = increased alk phos, nl bili, alt, ast, ggt- PBL - see xanthomas
|
|
|
|
extrahepatic copmlications of hepC?
|
cryoglobulinemia => membranous GN, B-cell ly,mphoma (not T), plsmacytoses, AI dz e.g. sjogren, thyroiditis, lichen planus, porphyria cutanea tarda, ITP
|
|
|
|
reye's syndrome
|
- aka fatty liver with encephalopathy- kid with infx, takes salicylate => mito injury => hypoglycemia, liver failure, cns damage- liver bx: fatty vacuolation without inflammation- tx glucose, ffp, mannitol- THUS ASA IS C/I IN KIDS
|
|
|
|
path of:acute etoh hepatitis, acute viral hepatitis, chronic active viral hepatits, PBC
|
- etoh: balloon degeneration with polymorphic (neu, mono, lymph) infiltrate- acute viral hep: panlobular monoulear infiltrate with bridging necrosis- chroinc: piecemeal necrosis- PBC: inflammatory granulomatous destruction of biliary ducts
|
|
|
|
emphysematous cholecystitis
|
infx GB wall by gas forming bacteria - clostridium, escherichia, staph, strep,. pseudo, kleb - increased risk from vascular problems, immunosuppression (DM), gallstones - sx: RUQ, N/V, crepitus - KUB shows air fluid in gallbladder; U/S: curvilinear gas shadowing - tx: cholecystectomy, abx against clost (zosyn or amp-sublactam) |
|
|
|
acute cholangitis
|
- charcot's tirad: RUQ pain, jaundice fever- biliar tract obstruction => bact infx
|
|
|
|
pancreatic pseudocyst
|
- fake cyst b/c no epithelial lingin, fibrous capsuel- contains inflammatory fluid: amylase, lipase, enterokinase- tx if persists > 6wks = drain
|
|
|
|
primary sclerosis cholangitis
|
- onion skin pattern stricturing of ducts- complications = biliary stricture, cholangitis, cholelithiasis, cholangiocarcinoma, CRC- associated with UC, see high HLA-B8, IgM, pANCA- dx via cholangiography => beading pattern, U/S and biopsy aren't useful- tx: ursodeoxycholate, dilation, stenting- Liver transplant else life span 12 yrs
|
|
|
|
hydatid cyst tx
|
- 2/2 echinococccus- surgical resection under albendazole- don't aspiration else anaphylaxis
|
|
|
|
cysticercosis
|
- infx by tenia solium => brain, muscle
|
|
|
|
dubin-johnson syndrome
|
- black liver- conjugated bilirubin, sephardic jews- trigger: pregnancy, ocp- urine: Nl urine coproporphyrin but 80% is type I vs type III- normal LFT is requirement for dx- no tx
|
|
|
|
black liver
|
dubin johnson
|
|
|
|
pt with chronic hepatitis and cirrhosis now with weight loss?
|
- first step in eval is check for tumor marker AFP- some imaging must be done b/c neg AFP doesn't rule out- checking ascite fluid is useless
|
|
|
|
pt with hydrothorax?
|
- first do therapeutic thoracentesis, salt restriction, diuretics- if those don't work then do TIPS- don't do portosytemic shunt b/c increased morbidity
|
|
|
|
pt on INH
|
- will have small increase in ALT, AST which is OK- if sx of hepatitis 2/2 iNH stop INH immediately
|
|
|
|
primary liver Ca |
- HCC: increased AFP, ill defined single lesion - hepatic adneoma- benign, women on OCP, one mass - hepatic angiocarcinome: hx of exposure to vinyl chloride gas, arsenic, thorium, malignant cells line vascular sx |
|
|
|
What is presentation of sq cell Ca? Where does it hit What is treatment? x3
|
i)nonhealing ulcer ii)the lower lip and below iii)a)excision w/.5-2 cm margins b)nodal dissection if affected c)possible radiation
|
|
|
|
What is interesting about mets of melanoma? what is the timetable like?
|
i)can go anywhere, like muscle of LV ii)not predictable: can be dead in a few months to 20 years b/w resection of primary and metastasis
|
|
|
|
What are sxs of retinal detachment? x2 What is bad prognostic factor?x2 What is intervention and is it an emergency?
|
i)a)floaters b)light flashes ii)a)snow storm in the eye or b)dark cloud at top of visual field: horshoe piece of retina pulled away and can rip out retina at rest. iii)emergency intervention w/laser spot welding
|
|
|
|
What is time line of the 3 kinds of neck masses?
|
i)congenital: have had it for long time, acutely worse ii)inflammatory: days to few weeks, and resolves after few weeks. iii)neoplasm: several months of growth
|
|
|
|
Where is thyroglossal duct cyst? x2 What are they connected to? What is removed in surgery? x3
|
i)a)midline b)level of hyoid ii)tongue iii)a)cyst b)middle of hyoid c)track leading to base of tongue
|
|
|
|
Where are branchial cleft cysts?
|
along anterior edge of SCM, anywhere from in front of tragus to base of neck
|
|
|
|
where is cystic hygroma? What does it feel and look like? What is mandatory b/4 surgery?
|
i)base of neck ii)large, mushy, ill-defined mass occupying entire supraclavicular area, seemingly extending into chest iii)CT b/c may extend into chest
|
|
|
|
What do you do for recently discovered enlarged LNs?
|
usually benign, so complete H and P w/followup in 3-4 weeks. W/u if still there
|
|
|
|
who gets lymphoma? What is presentation? x3 What is first steps? x2
|
i)young people ii)a)multiple enlarged nodes b)low grade fever c)night sweats iii)a)FNA can be done, but b)node removal and give to pathology
|
|
|
|
What is the usual source of metastatic tumor to supraclavicular nodes? How to get dx?
|
i)not from head and neck but below clavicle (lung or intraabdominal tumors) ii)node removal w/pathology
|
|
|
|
Who gets sq cc of mucosae of head and neck? x2 What is diagnostic w/u? What establishes diagnosis and what demonstrates extent? What can be done of the node itself, and what shouldn't be done? Why? what is treatment? x3
|
i)a)men who smoke and drink b)AIDS pts ii)panendoscopy to find primary iii)biopsy of primary; CT shows extent iv)FNA can be done, but open BX of neck mass shouldn't v)incision in neck will interfere w/surgical approach vi)a)resection b)radical neck dissection c)radiotherapy and platinum therapy
|
|
|
|
What are some symptoms of sqCC? x3
|
i)hoarseness ii)persistent painless ulcer on floor of mouth iii)persistent unilateral earache
|
|
|
|
What is presentation of acoustic nerve neuroma? What is best diagnostic modality?
|
i)sensory hearing loss in one ear but not the other ii)MRI
|
|
|
|
what are symptoms of facial nerve tumors? What is best study?
|
i)gradual, unilateral facial nerve paralysis of forehead and lower face (paralysis suddenly=Bells palsy) ii)gadolinium enhanced MRI
|
|
|
|
What are most parotid tumors cell type? Are they benign? What are symptoms of parotid cancer? x2 What can be done to get tissue and what can't? What is the appropriate way to excise/biopsy parotid tumor? Why? What is done for malignant tumors to treat?
|
i)pleomorphic adenoma ii)yes, but malig potential iii)a)hard mass b)painful c)produces paralysis (these don't happen in benign ones) iv)FNA; open BX v)parotidectomy vi)prevents recurrence and spares facial nerve vii)nerve is sacrificed and graft is performed
|
|
|
|
What is the cause of unilateral ENT problems in toddlers? (earache, rhinorrhea, wheezing) What is tx?
|
i)foreign bodies stuck there ii)endoscopy under anesthesia
|
|
|
|
What is ludwig angina and what is the cause? What is the problem with this that is why it is an emergency? What do you do? What may be needed? x2
|
i)abscess of floor of mouth; bad tooth infxn ii)threat to the airway iii)I and D iv)intubate and tracheostomy
|
|
|
|
What do you do for bell palsy?
|
prompt administration of anti-viral meds
|
|
|
|
Do facial nerve injuries due to trauma ever have delayed paralysis? Why do they get it later, and what will happen?
|
i)no: get paralysis immediately ii)if get later, due to swelling and will resolve on own
|
|
|
|
What is symptom of cavernous sinus thrombosis? What is it due to? How to manage? x4
|
i)get diplopia ii)frontal or ethmoid sinusitis iii)a)emergent hospitalization b)IV abx c)CT scans d)drainage of affected sinuses
|
|
|
|
what can you treat epistaxis in kids with? What do kids get it from? 18 y/o? x2 What do you need to do for each of these cases? What is management of elderly and hypertensive getting epistaxis? x2 What is last line therapy?
|
i)phenylephrine spray and local pressure ii)pick nose iii)a)coke b)juvenile nasopharyngeal angiofibroma iv)a)posterior packing b)surgical resection b/c can eat at nearby structure v)a)BP control b)posterior packing vi)surgical ligation of feeding vessels
|
|
|
|
What is diff in dizziness due to inner ear disease vs cerebral disease? What is treatment for each?
|
i)inner ear: room spinning around them ii)brain: unsteady pt but room is perceived to be stable iii)a)meclizine, phenergan, or diazepam b)neurologic w/u
|
|

